1. Remschmidt H, Belfer M. Mental health care for children and adolescents worldwide: a review. World Psychiatry 2005;4:147ŌĆō153.


2. Herrman H, Saxena S, Moodie R. Promoting mental health: concepts, emerging evidence, practice. A report of the World Health Organization, Department of Mental Health and Substance Abuse in collaboration with the Victorian Health Promotion Foundation and the University of Melbourne. Geneva: World Health Organization, 2005.
3. Durlak JA, Wells AM. Primary prevention mental health programs for children and adolescents: a meta-analytic review. Am J Community Psychol 1997;25:115ŌĆō152.


4. Jane-Llopis E, Hosman C, Jenkins R, Anderson P. Predictors of efficacy in depression prevention programmes. Meta-analysis. Br J Psychiatry 2003;183:384ŌĆō397.


5. Wood C, Wise M. Building Australia's capacity to promote mental health: review of infrastructure for promoting health in Australia. Canberra: National Mental Health Strategy, 1997.
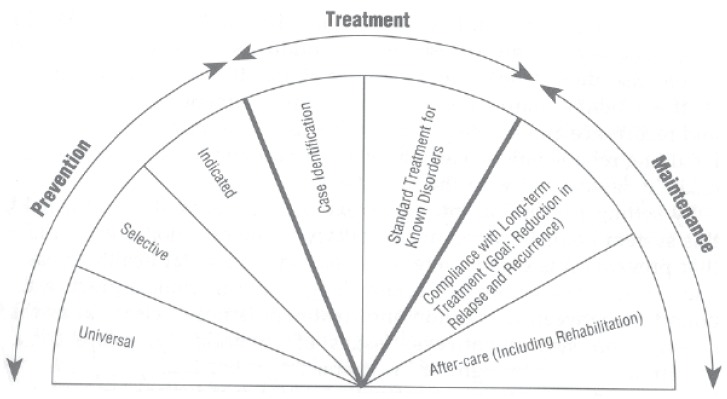
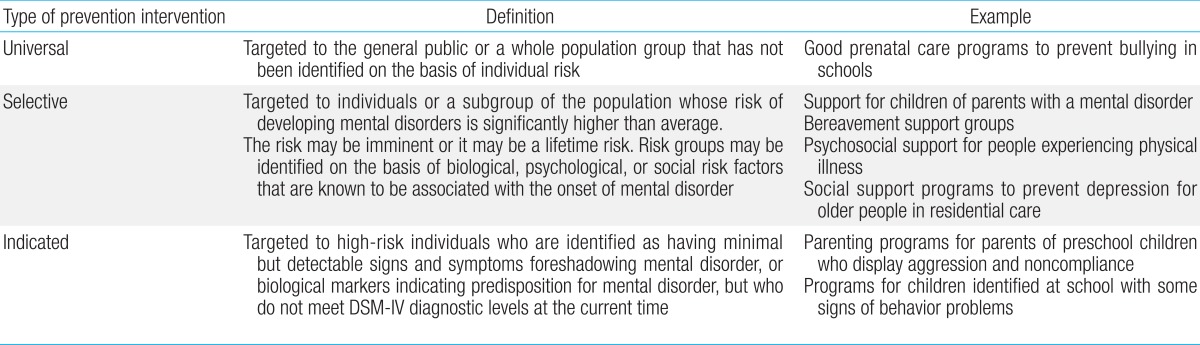
6. Saxena S, Jane-Llopis E, Hosman C. Prevention of mental and behavioural disorders: implications for policy and practice. World Psychiatry 2006;5:5ŌĆō14.


7. Caplan G. Principles of preventive psychiatry. New York: Basic Books, 1964.
8. Mrazek PB, Haggerty RJ. Reducing risks for mental disorders: frontiers for preventive intervention research. Washington: National Academies Press, 1994.
9. Gordon RS Jr. An operational classification of disease prevention. Public Health Rep 1983;98:107ŌĆō109.


10. Lee YS, Kim B, Hong HJ, Noh KS. Systems of care in child and adolescent psychiatry in Korea. Psychiatry Investig 2006;3:26ŌĆō31.
11. Cohen P, Cohen J, Kasen S, Velez CN, Hartmark C, Johnson J, et al. An epidemiological study of disorders in late childhood and adolescence--I. Age- and gender-specific prevalence. J Child Psychol Psychiatry 1993;34:851ŌĆō867.


12. Costello EJ, Egger H, Angold A. 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. J Am Acad Child Adolesc Psychiatry 2005;44:972ŌĆō986.


13. Goodman SH, Hoven CW, Narrow WE, Cohen P, Fielding B, Alegria M, et al. Measurement of risk for mental disorders and competence in a psychiatric epidemiologic community survey: the National Institute of Mental Health Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) Study. Soc Psychiatry Psychiatr Epidemiol 1998;33:162ŌĆō173.


14. Knitzer J, Cooper J. Beyond integration: challenges for children's mental health. Health Aff (Millwood) 2006;25:670ŌĆō679.


15. Burns BJ, Costello EJ, Angold A, Tweed D, Stangl D, Farmer EM, et al. Children's mental health service use across service sectors. Health Aff (Millwood) 1995;14:147ŌĆō159.


16. Sawyer MG, Arney FM, Baghurst PA, Clark JJ, Graetz BW, Kosky RJ, et al. The mental health of young people in Australia: key findings from the child and adolescent component of the national survey of mental health and well-being. Aust N Z J Psychiatry 2001;35:806ŌĆō814.


17. Cho SM, Kim HS, Kim HJ, Shin YM. Perceived need and use of child mental health services in Korea. Community Ment Health J 2009;45:56ŌĆō61.


19. Roth A, Fonagy P. What works for whom?: a critical review of psychotherapy research. New York: The Guilford Press, 2006.
20. Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 2003;289:3095ŌĆō3105.


21. Garrison CZ, Waller JL, Cuffe SP, McKeown RE, Addy CL, Jackson KL. Incidence of major depressive disorder and dysthymia in young adolescents. J Am Acad Child Adolesc Psychiatry 1997;36:458ŌĆō465.


22. Matsuura M, Okubo Y, Kojima T, Takahashi R, Wang YF, Shen YC, et al. A cross-national prevalence study of children with emotional and behavioural problems: a WHO collaborative study in the Western Pacific Region. J Child Psychol Psychiatry 1993;34:307ŌĆō315.


23. Juon HS, Nam JJ, Ensminger ME. Epidemiology of suicidal behavior among Korean adolescents. J Child Psychol Psychiatry 1994;35:663ŌĆō676.


24. Choi WK. A study on the socio-structural cause of youth suicide. Soc Welf Policy 2004;18:5ŌĆō30.
25. Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 2007;164:942ŌĆō948.


26. Biederman J, Faraone SV, Milberger S, Jetton JG, Chen L, Mick E, et al. Is childhood oppositional defiant disorder a precursor to adolescent conduct disorder? Findings from a four-year follow-up study of children with ADHD. J Am Acad Child Adolesc Psychiatry 1996;35:1193ŌĆō1204.


27. Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull 1997;121:65ŌĆō94.


28. Cho SC, Kim BN, Kim JW, Rohde LA, Hwang JW, Chungh DS, et al. Full syndrome and subthreshold attention-deficit/hyperactivity disorder in a Korean community sample: comorbidity and temperament findings. Eur Child Adolesc Psychiatry 2009;18:447ŌĆō457.


29. Yang SJ, Cheong S, Hong SD. Prevalence and correlates of attention deficit hyperactivity disorder: school-based mental health services in Seoul. J Korean Neuropsychiatr Assoc 2006;45:69ŌĆō76.
30. Rigby K. New perspectives on bullying. London: Jessica Kingsley Publishers, 2002.
31. Smith PK, Cowie H, Olafsson RF, Liefooghe AP, Almeida A, Araki H, et al. Definitions of bullying: a comparison of terms used, and age and gender differences, in a fourteen-country international comparison. Child Dev 2002;73:1119ŌĆō1133.


32. Koo H. The nature of school bullying in South Korea. London: Goldsmiths, University of London, 2005;[unpublished doctoral dissertation].
33. Yang SJ, Kim JM, Kim SW, Shin IS, Yoon JS. Bullying and victimization behaviors in boys and girls at South Korean primary schools. J Am Acad Child Adolesc Psychiatry 2006;45:69ŌĆō77.


34. Kim YS, Koh YJ, Leventhal B. School bullying and suicidal risk in Korean middle school students. Pediatrics 2005;115:357ŌĆō363.


35. Jang KS, Hwang SY, Choi JY. Internet addiction and psychiatric symptoms among Korean adolescents. J Sch Health 2008;78:165ŌĆō171.


36. Yoo HJ, Cho SC, Ha J, Yune SK, Kim SJ, Hwang J, et al. Attention deficit hyperactivity symptoms and internet addiction. Psychiatry Clin Neurosci 2004;58:487ŌĆō494.


37. Ryu EJ, Choi KS, Seo JS, Nam BW. The relationships of Internet addiction, depression, and suicidal ideation in adolescents. J Korean Acad Nurs 2004;34:102ŌĆō110.

38. Committee on the Prevention of Mental Disorders and Substance Abuse Among Children, Youth, and Young Adults: Research Advances and Promising Interventions. O'Connell ME, Boat T, Warner KE, editors. Preventing mental, emotional, and behavioral disorders among young people: progress and possibilities. Washington, D.C.: National Academies Press, 2009.
39. Farmer EM, Burns BJ, Phillips SD, Angold A, Costello EJ. Pathways into and through mental health services for children and adolescents. Psychiatr Serv 2003;54:60ŌĆō66.


40. Ringeisen H, Henderson K, Hoagwood K. Context matters: schools and the" research to practice gap" in children's mental health. School Psychol Rev 2003;32:153ŌĆō168.

41. Rones M, Hoagwood K. School-based mental health services: a research review. Clin Child Fam Psychol Rev 2000;3:223ŌĆō241.


42. Harrington R, Clark A. Prevention and early intervention for depression in adolescence and early adult life. Eur Arch Psychiatry Clin Neurosci 1998;248:32ŌĆō45.


43. Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Br J Psychiatry 2000;177:534ŌĆō539.


44. Oh K, Lee H. Development of Korean version of child behavior checklist (K-CBCL). Seoul: Korean Research Foundation Report, 1990.
45. Hwang JW, Lyoo IK, Kim BN, Shin MS, Kim SJ, Cho SC. The relationship between temperament and character and psychopathology in community children with overweight. J Dev Behav Pediatr 2006;27:18ŌĆō24.


46. Kim YS, So YK, Noh JS, Choi NK, Kim SJ, Koh YJ. Normative Data on the Korean ADHD Rating Scales (K-ARS) for Parents and Teacher. J Korean Neuropsychiatr Assoc 2003;42:352ŌĆō359.
47. Shin NY, Shin MS. Body dissatisfaction, self-esteem, and depression in obese Korean children. J Pediatr 2008;152:502ŌĆō506.


49. Ra HJ, Park GS, Do HJ, Choi JK, Joe HG, Kweon HJ, et al. Factors influencing the impulse of suicide in adolescence. J Korean Acad Fam Med 2006;27:988ŌĆō997.
50. Ha JH, Chin B, Park DH, Ryu SH, Yu J. Characteristics of excessive cellular phone use in Korean adolescents. Cyberpsychol Behav 2008;11:783ŌĆō784.






 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


