Article Contents
| Clin Exp Pediatr > Volume 65(12); 2022 |
|
Abstract
Footnotes
Funding
The surveillance study of the Korean Childhood Community-Acquired Pneumonia Study Group (KoC-CAPS) was supported by a grant from the Korea Disease Control and Prevention Agency, Republic of Korea (grant number: 4800- 4821-304). This fund provides financial support in the investigation, design of the study, data collection, data analysis, and interpretation of data.
Acknowledgments
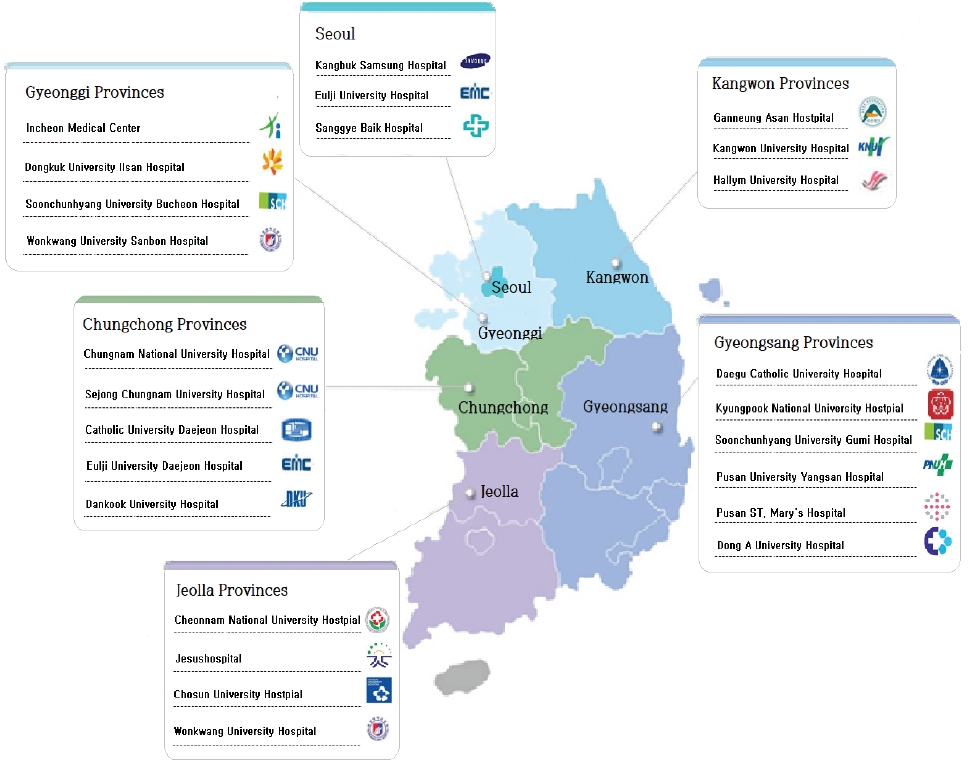
Fig. 1.
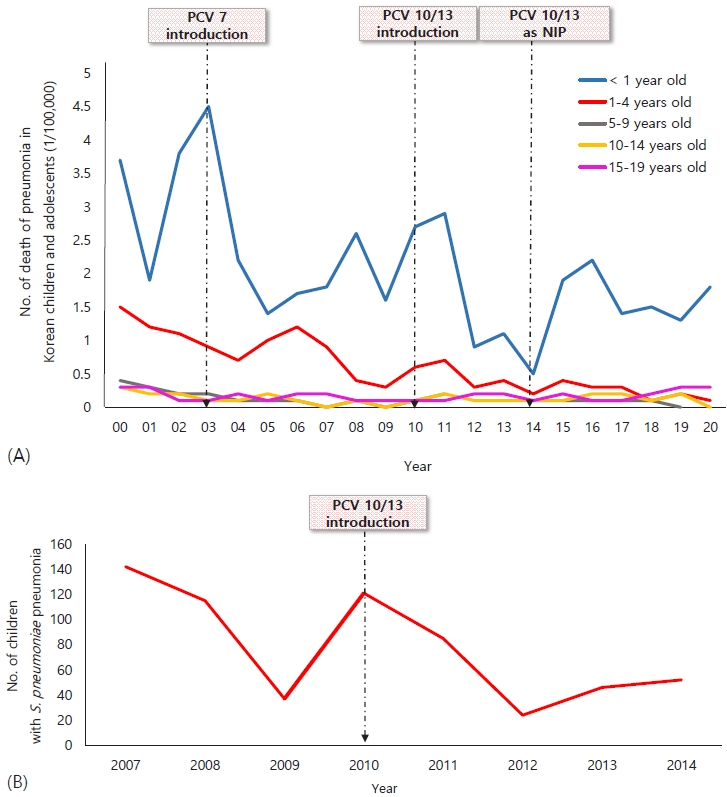
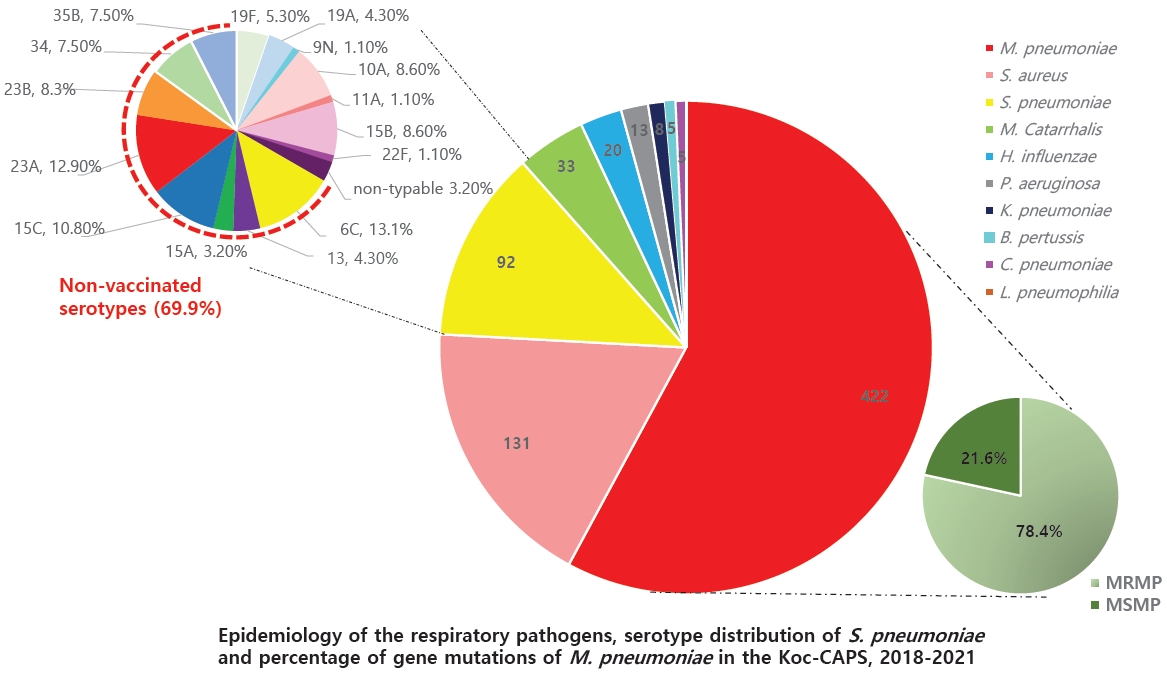
Fig. 2.
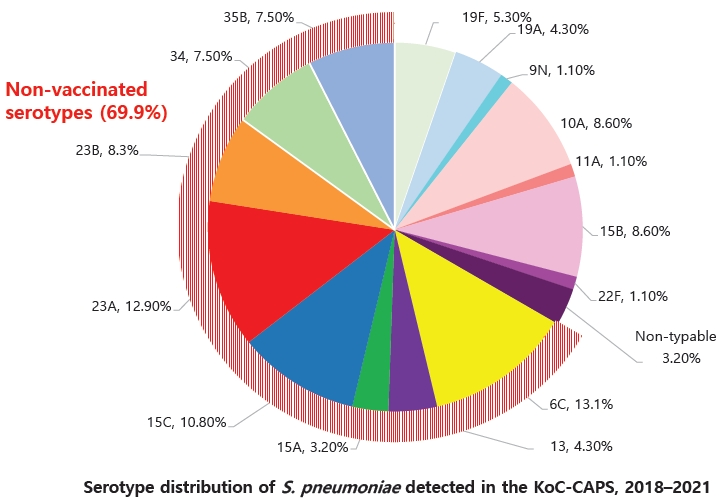
Fig. 4.
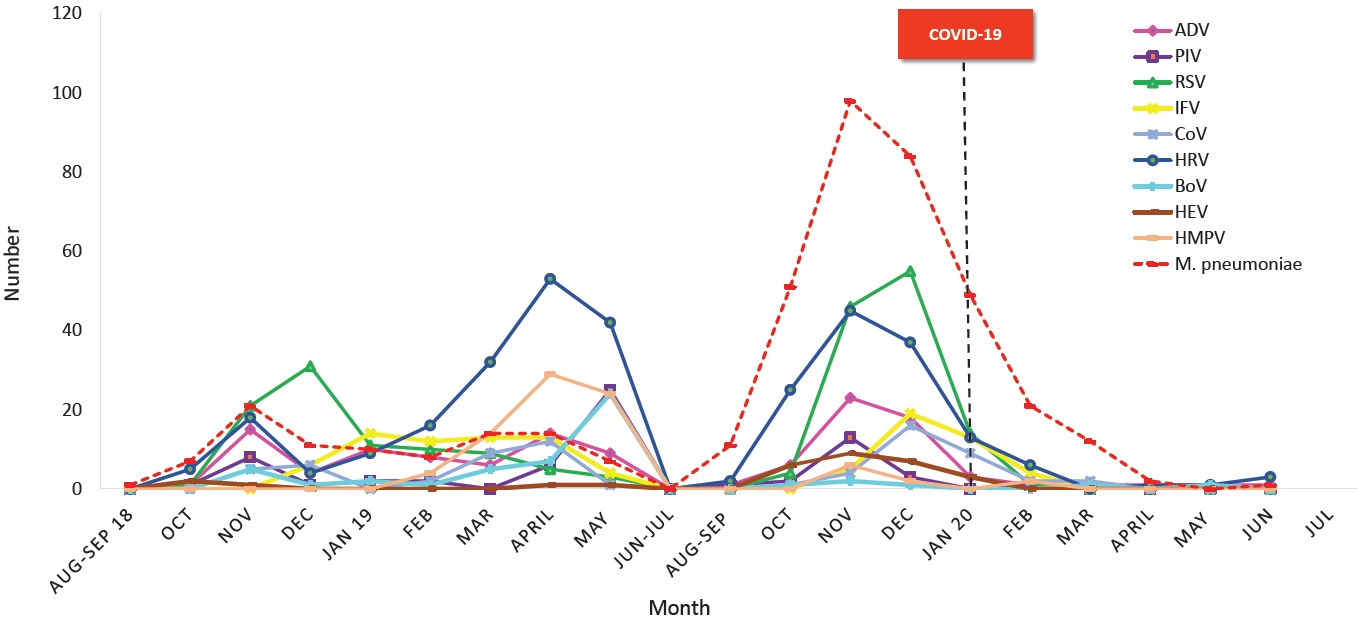
Fig. 5.
Table 1.
| Country | Study | No. of institutions | Origin of samples | Research period | No. of subjects | Age group (yr) | Population | Bacterial pathogen | Atypical bacterial pathogen | Viral pathogen |
|---|---|---|---|---|---|---|---|---|---|---|
| US | Jain et al. [12] | Multicenter (3 centers) | Naso/oropharyngeal swab | 2010–2012 | 2,358 | 0–18 | Hospitalized with CAP | 175 (8%) | 178 (8%) | 1,462 (66%) |
| BAL | S. pneumoniae (M/C) | M. pneumonia | RSV (M/C) | |||||||
| Sputum | ||||||||||
| PF | ||||||||||
| ET aspirate | ||||||||||
| Blood culture | ||||||||||
| Blood PCR | ||||||||||
| Singapore | Chiang et al. [48] | Single center | Sputum | For 3 yr | 1,702 | 0–18 | Hospitalized with CAP | 175 (10.3%) | 350 (20.6%) | 94 (5.5%) |
| Nasopharyngeal aspirates | S. pneumoniae (M/C) | M. pneumoniae | RSV (M/C) | |||||||
| PF | ||||||||||
| Blood culture | ||||||||||
| Taiwan | Chi et al. [49] | Multicenter (8 centers) | Blood culture | 2010–2013 | 1,032 | 0–18 | Hospitalized with CAP | 326 (31.6%) | 233 (22.6%) | 180 (17.4%) |
| PF | S. pneumoniae (M/C) | M. pneumoniae | ADV (M/C) | |||||||
| Nasopharyngeal swab | ||||||||||
| China | Oumei et al. [50] | Blood culture | 2015 | 1,500 | 0–18 | Hospitalized with CAP | 486 (32.4%) | 291 (33.5%) | ||
| Oropharyngeal swab | M. pneumoniae | RSV (M/C) | ||||||||
| Peru | del Valle-Mendoza et al. [51] | Single center | Nasopharyngeal swab | 2009–2010 | 146 | 0–18 | Hospitalized with CAP | 58 (39.7%) | 52 (35.6%) | |
| M. pneumoniae (M/C) | RSV (M/C) | |||||||||
| Australia | Bhuiyan et al. [52] | Multicenter | Nasopharyngeal swab | 2015–2017 | 230/230 | 0–17 | Hospitalized with CAP/attended clinic without URI | 19 (8.2%) | 130 (56.5%) | |
| M. pneumoniae | RSV (M/C) |
CAP, community-acquired pneumonia; BAL, bronchoalveolar lavage; PF, pleural fluid; ET, endotracheal; PCR, polymerase chain reaction; S. pneumoniae, Streptococcus pneumoniae; M. pneumoniae , Mycoplasma pneumoniae; M/C, most common; RSV, respiratory syncytial virus; ADV, adenovirus; URI, upper respiratory tract infections.
Table 2.
| Study | No. of institutions | Origin of samples | Research period | No. of subjects | Age group | Population | Pneumonia incidence | Bacterial pathogen | Atypical bacterial pathogen | Viral pathogen |
|---|---|---|---|---|---|---|---|---|---|---|
| Moon et al. [53] | 2 Centers | Nasopharyngealaspirates | 2000–2001 | 796 | 0–18 yr | Hospitalized with ALRI | 75 (36%) | 208 (26.1%) | ||
| ADV (Seoul) | ||||||||||
| RSV (Masan) | ||||||||||
| Choi et al. [54] | 2 Centers | Nasopharyngealaspirates | 2000–2005 | 2,198 | 0–5 yr | Hospitalized with ALRI | RSV (M/C) | |||
| Cheong et al. [57] | Single center | Nasopharyngealaspirates | 2005 | 654 | 0–15 yr | Hospitalized with ALRI | 169 (72.2%) | 234 (35.4%) | ||
| ADV (M/C) | ||||||||||
| Eun et al. [59] | Single center | Serologic diagnosis | 1986–2004 | 2,405 | 0–18 yr | Diagnosed with CAP | 568 (23.6%) | |||
| M. pneumoniae | ||||||||||
| Kwon et al. [58] | Single center | Nasopharyngeal aspirates | 2002–2006 | 3,854 | 0–17 yr | Hospitalized with ALRI | 276 (73%) | 98 (35.5%) | ||
| PIV3 (M/C) | ||||||||||
| Chun et al. [55] | Single center | Nasopharyngeal aspirates | Nov 2007–April 2008 | 297 | 0–5 yr | Hospitalized with ALRI | 222 (75%) | 120 (54%) | ||
| RSV (M/C) | ||||||||||
| Kim et al. [56] | 3 Centers | Nasopharyngeal aspirates | 2008–2009 | 418 | 0–5 yr | Hospitalized with ALRI | 225 (53.8%) | 154 (68.4%) | ||
| RSV (M/C) | ||||||||||
| Lee et al. [60] | Single center | Blood culture | 2006–2008 | 288 | 0–15 yr | Hospitalized with CAP (lobar/lobular form) | 27 (9.4%) | 146 (50.7%) | 17 (5.9%) | |
| Nasopharyngeal aspirates | S. pneumoniae (M/C) | M. pneumoniae | ||||||||
| Sputum | ||||||||||
| Urinary S. pneumoniae | ||||||||||
| Ag | ||||||||||
| Kim [61] | 2 Centers | Nasopharyngeal aspirates | 2010–2011 | 1,520 | 0–18 yr | Hospitalized with ALRI | 595 (52.3%) | 210 (67.7%) | ||
| RSV (M/C) | ||||||||||
| Lee et al. [62] | Multicenter (146 EDs) | 2012 | 38,415 | 0–18 yr | Diagnosed with CAP from ED | 2,039 (5.3%) | 1,732 (4.5%) | 11,146 (29%) | ||
| M. pneumoniae | IFV (M/C) | |||||||||
| Shin et al. [63] | Multicenter (117 EDs) | 2007–2014 | 329,380 | 1 mo–18 yr | Diagnosed with CAP from ED | 4,316 (1.3%) | 12,635 (3.8%) | 27,607 (8.4%) | ||
| S. pneumoniae (M/C) | M. pneumoniae | IFV (M/C) | ||||||||
| An et al. [65] | Multicenter (5 centers) | Nasopharyngeal aspirates | 2015–2016 | 428 | 0–18 yr | Hospitalized with CAP | 298 (69.6%) | 261 (61%) | ||
| Blood culture | M. pneumoniae | RV, RSV | ||||||||
| Lee et al. [64] | Multicenter (23 centers) | Nasopharyngeal aspirates | 2010–2015 | 30,944 | 0–18 yr | Hospitalized with CAP | 9,183 (29.6%) | 16,895 (54.5%) | ||
| Blood culture | M. pneumoniae | RSV (M/C) | ||||||||
| Roh et al. [66] | Multicenter (27 centers) | Nasopharynx | 2018–2020 | 1,023 | 1 mo–18 yr | Hospitalized or ambula- tory with CAP | 264 (25.8%) | 432 (42.2%) | 65.70% | |
| Nasal swab | S. aureus (M/C) | M. pneumoniae (M/C)) | RSV (M/C) | |||||||
| Throat swab | ||||||||||
| Sputum | ||||||||||
| BAL | ||||||||||
| Transtracheal aspirates |
CAP, community-acquired pneumonia; ALRI, acute lower respiratory tract infection; ADV, adenovirus; RSV, respiratory syncytial virus; M. pneumoniae , Mycoplasma pneumoniae; PIV3, parainfluenza virus type 3; M/C, most common; S. pneumoniae , Streptococcus pneumoniae; EDs, emergency departments; IFV, influenza virus; BAL, bronchoalveolar lavage; S. aureus, Staphylococcus aureus.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


