Article Contents
| Korean J Pediatr > Volume 61(4); 2018 |
|
Abstract
We report a unique case of intestinal duplication detected on posterior reversible encephalopathy syndrome (PRES) in a 13-year-old girl. She was admitted to the pediatric Emergency Department because of generalized seizures. Radiological assessment revealed a large, well-defined, thick-walled cystic lesion in the mid abdomen, suggestive of duplication cyst associated to a PRES. Exploration confirmed the diagnosis of ileal duplication cyst, and the mass was resected. The postoperative course was uneventful. Both hypertension and neurological dysfunction resolved after the mass resection. A followup brain magnetic resonance imaging was performed 9 months later and showed complete resolution of the cerebellar changes. Although extrinsic compression of the retroperitoneal structures has not been reported in the literature as a complication of duplication cyst, we strongly believe that this is the most logical and plausible hypothesis that would explain the pathogenesis of PRES in our patient.
In pediatric patients with headaches, seizures or encephalopathy, posterior reversible encephalopathy syndrome (PRES) is considered as an essential treatable diagnosis. Missing this clinico-radiological entity can have serious consequences. This pathology has been associated with several conditions predominantly hypertension, eclampsia, and immunosuppressive therapy. The pathogenesis remains controversial. Cerebral blood perfusion abnormalities and blood-brain barrier dysfunction are thought to be the cause of PRES. Although cases of PRES without hypertension have been reported, the latter remains the key to most mechanisms proposed.
The list of conditions associated with PRES is increasing progressively. We add our case report about intestinal duplication to this list and hypothesize the possible mechanism involved in its pathogenesis.
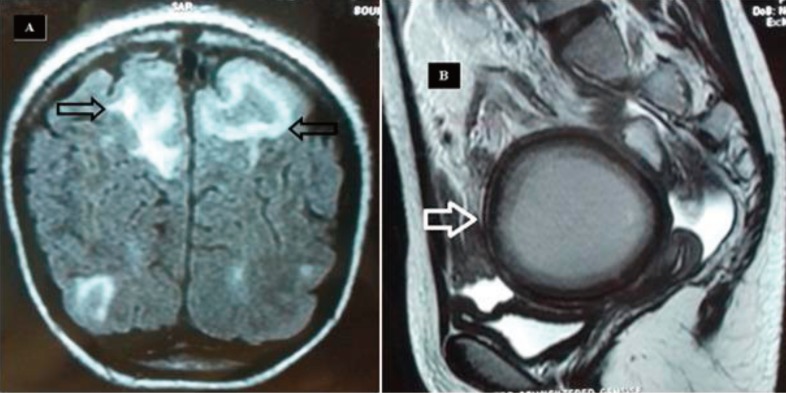
A 13-year-old girl was admitted to the pediatric Emergency Department because of generalized seizures. The history of the disease dated back to a week when the patient complained about intermittent abdominal pain and vomiting. The parents were questioned about the different drugs and chemicals received recently by the infant. We found then the notion of automedication, 3 days ago, by metoclopramide (MTC). Physical examination revealed a unconscious girl with normal temperature, heart rate 90 beats/min, respiratory rate 19/min, blood pressure 150/90 mmHg, and a median mobile abdominal mass of 10 cm large. Abdominal X-ray did not reveal any pathology. Radiological assessment revealed a large well defined thick walled cystic lesion in mid abdomen suggestive of duplication cyst associated to a PRES (Fig. 1).
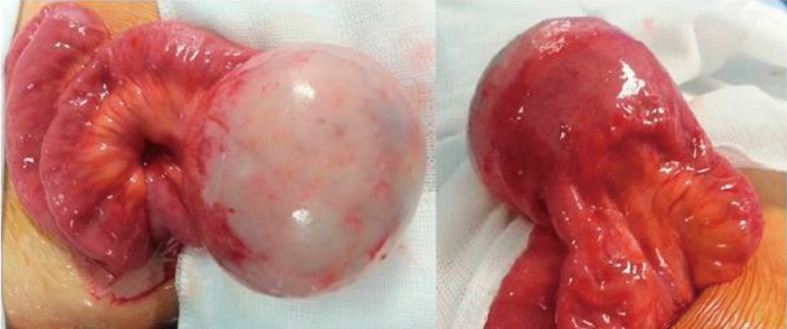
After stabilization, the patient was operated. Surgical exploration revealed a 13×6-cm noncomplicated duplication cyst with a common wall with the ileum, 30 cm proximal to the ileocecal valve (Fig. 2). A resection of the mass and end-to-end ileal anastomosis was performed. Histopathology examination of the specimens showed duplication cyst lined with ileal mucosa without any ectopic tissue. The postoperative course was uneventful. Both hypertension and neurologic dysfunction resolved after the mass resection. The blood pressure returned to normal and during follow-up visits it has remained in the 110–100/70–80 range.
A follow-up magnetic resonance imaging brain was performed 9 months later and it showed complete resolution of the cerebellar changes.
Duplications are defined as a very rare congenital malformation, mostly located in the Ileum. Their usual complications are infection, perforation, intestinal obstruction, intussusception, or volvulus.1) However, intestinal duplication has not been previously described in association with the development of PRES.
PRES which has been described in adults more than in children is a set of clinical and radiological manifestations. It combines neurologic symptoms with usually reversible bilateral posterior hemispheric edema on neuroimaging.2) Many pathological conditions and treatments have been associated with this syndrome.2,3) However it is the acute hypertension that remains the most reported. Our patient had no previous history of hypertension or preexisting pathology that could explain this hypertensive peak responsible of PRES.
Prevalence of hypertension in children is less than 1%. It can be of renal or extrarenal origin. Ahn et al.4) evaluated 33 pediatric patients who were diagnosed as having hypertensive encephalopathy. It appeared that renal artery stenosis was the first responsible etiology of renal origin hypertension. Essential hypertension was the first responsible etiology of nonrenal origin hypertension. Some sporadic reports of PRES following surgery exist in the literature. Gopalakrishnan et al.5) describe the case of a 14-year-old girl presented with clinical and imaging findings consistent with PRES after spinal surgery, and postulate that acute spinal cord compression must be included as one of the possible etiologies for PRES.
The most likely hypothesis in our case is that hypertension was of renal origin, and precisely due to external compression of the renal arteries by the duplication. Hypertension induced breakdown in cerebral autoregulation, leading to leakage of fluid into the brain with neurologic complications. This hypothesis is supported by the fact that after resection of the mass the obstruction was relieved and both hypertension and neurologic dysfunction were resolved. In a reported case similar to ours, the compression syndrome was due to severe chronic constipation and fecal impaction.6) Aureli et al.7) report the case of a 2-year-old baby with PRES due to neuroblastoma. They announce a new variant of PRES that is directly related to neuroblastoma and not due to its treatment. One of the hypotheses proposed is that the hypertension could be related to the compression of the renal arteries bilaterally by the tumor.
In our patient, there is another less likely hypothesis related to MTC intake. This drug is known as a widely used antiemetic.8) This drug was administrated by the mother, without prescription, to manage nausea and vomiting which were probably caused by the duplication. MTC has been shown to produce hypertensive crises in patients with phaeochromocytoma possibly by causing catecholamine release from the tumor.9) The evidence supporting MTC induced hypertension in our patient is scarce. A review of the literature resulted in only 4 published reports of MTC-induced increase of blood pressure unrelated to phaeochromocytoma.10,11,12,13) The mechanism that causes hypertension with MTC is not known.
Although extrinsic compression of retroperitoneal structures has not been reported in the literature as a complication of duplication cyst, we strongly believe that this is the most logical and plausible hypothesis that would explain the pathogenesis of PRES in our patient.
Notes
Conflicts of interest:
No potential conflict of interest relevant to this article was reported.
References
1. Tiwari C, Shah H, Waghmare M, Makhija D, Khedkar K. Cysts of gastrointestinal origin in children: varied presentation. Pediatr Gastroenterol Hepatol Nutr 2017;20:94–99.



2. Gümüş H, Per H, Kumandaş S, Yikilmaz A. Reversible posterior leukoencephalopathy syndrome in childhood: report of nine cases and review of the literature. Neurol Sci 2010;31:125–131.


3. Zuccoli G, Fitzgerald RT, Nardone R, Furtado AD, Abdel-Hamid H. The link between arterial blood pressure and vasogenic edema in pediatric PRES. Neuroradiology 2015;57:865–866.


4. Ahn CH, Han SA, Kong YH, Kim SJ. Clinical characteristics of hypertensive encephalopathy in pediatric patients. Korean J Pediatr 2017;60:266–271.



5. Gopalakrishnan CV, Vikas V, Nair S. Posterior reversible encephalopathy syndrome in a case of postoperative spinal extradural haematoma: case report and review of literature. Asian Spine J 2011;5:64–67.



6. Prasad M, Wetzler G, Holtmann J, Dapul H, Kupferman JC. Constipation, renovascular hypertension, and posterior reversible encephalopathy syndrome (PRES). Eur J Pediatr 2016;175:421–425.


7. Aureli V, Giammattei L, Maduri R, Daniel RT, Messerer M. Posterior reversible encephalopathy syndrome (PRES) due to neuroblastoma in a child presenting with acute hydrocephalus. Childs Nerv Syst 2018;34:15–17.


8. Nguyen TT, Petzel Gimbar RM. Sustained hypotension following intravenous metoclopramide. Ann Pharmacother 2013;47:1577–1580.


9. Sheinberg R, Gao WD, Wand G, Abraham S, Schulick R, Roy R, et al. Case 1--2012. A perfect storm: fatality resulting from metoclopramide unmasking a pheochromocytoma and its management. J Cardiothorac Vasc Anesth 2012;26:161–165.


10. Sheridan C, Chandra P, Jacinto M, Greenwald ES. Transient hypertension after high doses of metoclopramide. N Engl J Med 1982;307:1346

Fig. 1
Radiological assessment. (A) Brain magnetic resonance image showing bilateral, subcortical, white matter on T2 lesions in the frontal and occipital lobes (black arrows), suggesting posterior reversible encephalopathy syndrome. (B) Abdominal magnetic resonance image showing a large well-defined, thick-walled cystic lesion (white arrow).





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


