Article Contents
| Korean J Pediatr > Volume 56(8); 2013 |
Abstract
Purpose
Allergic disease and its comorbidities significantly influence the quality of life. Although the comorbidities of allergic diseases are well described in adult populations, little is known about them in preschool children. In the present study, we aimed to assess the prevalence and comorbidity of allergic diseases in Korean preschool children.
Methods
We conducted a cross-sectional study comprising 615 Korean children (age, 3 to 6 years). Symptoms of allergic diseases were assessed using the Korean version of the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire that was modified for preschool children. Comorbidities of allergic diseases were assessed by 'In the last 12 months, has your child had symptoms?'.
Results
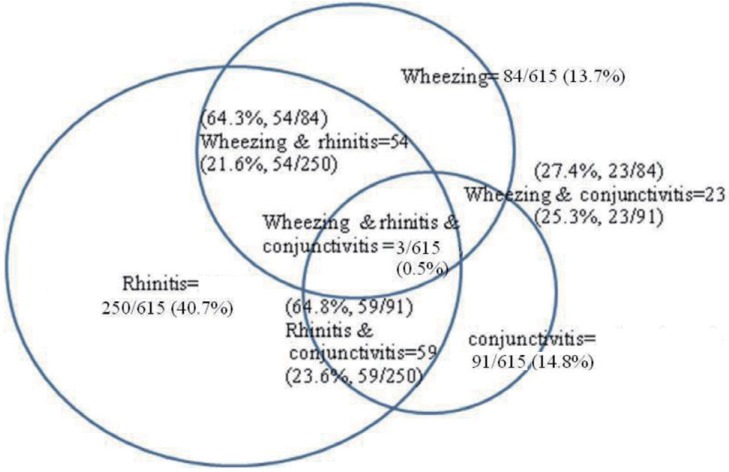
The prevalence of symptoms of asthma, allergic rhinitis, and atopic dermatitis as recorded using the ISAAC questionnaire, within the last 12 months was 13.8%, 40.7%, and 20.8%, respectively. The symptom rates of allergic conjunctivitis, food allergy, and drug allergy were 14.8%, 10.4%, and 0.8%, respectively. The prevalence of allergic rhinitis in children with asthma was 64.3% and that of asthma in children with allergic rhinitis was 21.6%. The prevalence of rhinitis in children with conjunctivitis was 64.8% and that of conjunctivitis in children with rhinitis was 23.6%.
Conclusion
The prevalence of current rhinitis in our preschool children is shown to be higher than that previously reported. Allergic conjunctivitis is closely associated with asthma and allergic rhinitis. However, further studies are warranted to determine the prevalence and effects of these comorbidities on health outcomes in preschool children.
Asthma and allergic diseases are among the most common disorders in children, and their prevalence has increased in most parts of the world1,2). The International Study of Asthma and Allergies in Childhood (ISAAC) found that the prevalence of allergic diseases in children aged 6 and 14 years varies significantly from 0.3% to 20.5%, but is gradually increasing3,4). A National Survey on the prevalence of symptoms of allergic diseases on Korean children aged 6 and 14 years has demonstrated that the prevalence of asthma and allergic diseases is on the rise5). However, little data are available on the prevalence of allergic diseases in preschool children.
There are distinct epidemiological parallels between atopic dermatitis, asthma, and allergic rhinitis. Generally, childhood eczema precedes the development of asthma and allergic rhinitis in the so-called atopic march6). Furthermore, asthma and allergic rhinitis frequently coexist7-10). In adult studies, allergic rhinitis is found in 30% to 90% of patients with asthma9,10). Thus, the clinical signs of asthma and allergic diseases follow each other and can co-occur11,12).
Although the comorbidities of allergic diseases have been well described in adult and children populations, less is known about such conditions in preschool children7,8,13). A few previous studies have indicated that comorbidities in Western countries differ from those in Korean populations14,15). Little data are available in preschool children to evaluate prevalence of asthma, allergic rhinitis, atopic dermatitis, allergic conjunctivitis, food allergy, drug allergy, and comorbidities. In addition, assessing the comorbidities of allergic diseases may help clinicians recognize symptoms of allergic diseases early and prompt treatment. Therefore, we hypothesized that asthma and other allergic diseases might coexist in preschool children and the prevalence of allergic diseases in our children differed from those of other regions. The aim of the present study was to determine the prevalence of allergic diseases and their comorbidities in preschool children using the standard ISAAC questionnaire, and to compare our results with previous studies.
The source population comprised 629 preschool children aged 3 to 6 years who were recruited from randomly selected 5 daycare centers in Seongnam from April to June of 2009. We used the Korean version of ISAAC questionnaire and the questionnaires were distributed and collected through each daycare center. Their parents filled out the ISAAC questionnaire at home and returned it within few days. A total of 615 subjects (97.7%) returned the questionnaires with valid answers. The study was approved by the ethics committee of the CHA University, and written informed consent was obtained from the parents of all participating children.
The Korean version of the ISAAC questionnaire16) was used to determine the presence of symptoms of wheezing, allergic rhinitis, atopic dermatitis, allergic conjunctivitis, food allergy, and drug allergy. Questions regarding body mass index (BMI), a family history of allergic disease, secondhand smoking, and pet ownership were also asked.
In this study, we estimated the prevalence of allergic diseases, such as, asthma, allergic rhinitis and atopic dermatitis, based on positive answers to written questions per Hong et al.17): 1) 'Has your child ever had symptoms?' (symptom, ever); 2) 'In the last 12 months, has your child had symptoms?' (symptom, last 12 months); 3) 'Has your child been diagnosed by a physician as ever having the disorder?' (diagnosis, ever); and 4) 'In the last 12 months, Has your child been treated by a physician for the disorder?' (treatment, last 12 months). "Current" was defined as a positive response to 'symptom, last 12 months.'
To diagnose allergic conjunctivitis, food allergy, and drug allergy, which were not included in the ISAAC questionnaire, we considered a child to have allergic conjunctivitis if he responded yes to the question 'Has your child had itchy watery eyes without having acute hemorrhagic conjunctivitis?' A child had a food allergy if he responded yes to the question 'Has your child had allergic symptoms after ingesting certain foods?' A child had a drug allergy if he responded yes to the question 'Has your child had allergic symptoms provoked by certain drugs?'
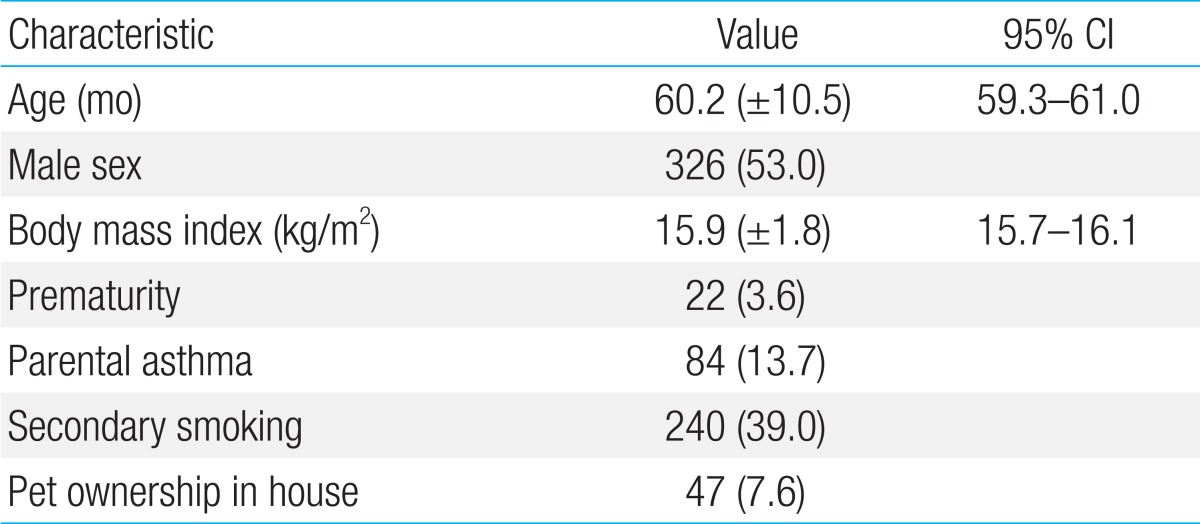
Table 1 shows the basic characteristics of the 615 preschool children from whom questionnaire data were available. The mean age of the subjects was 60.2±10.5 months (male; n=326, 53%).
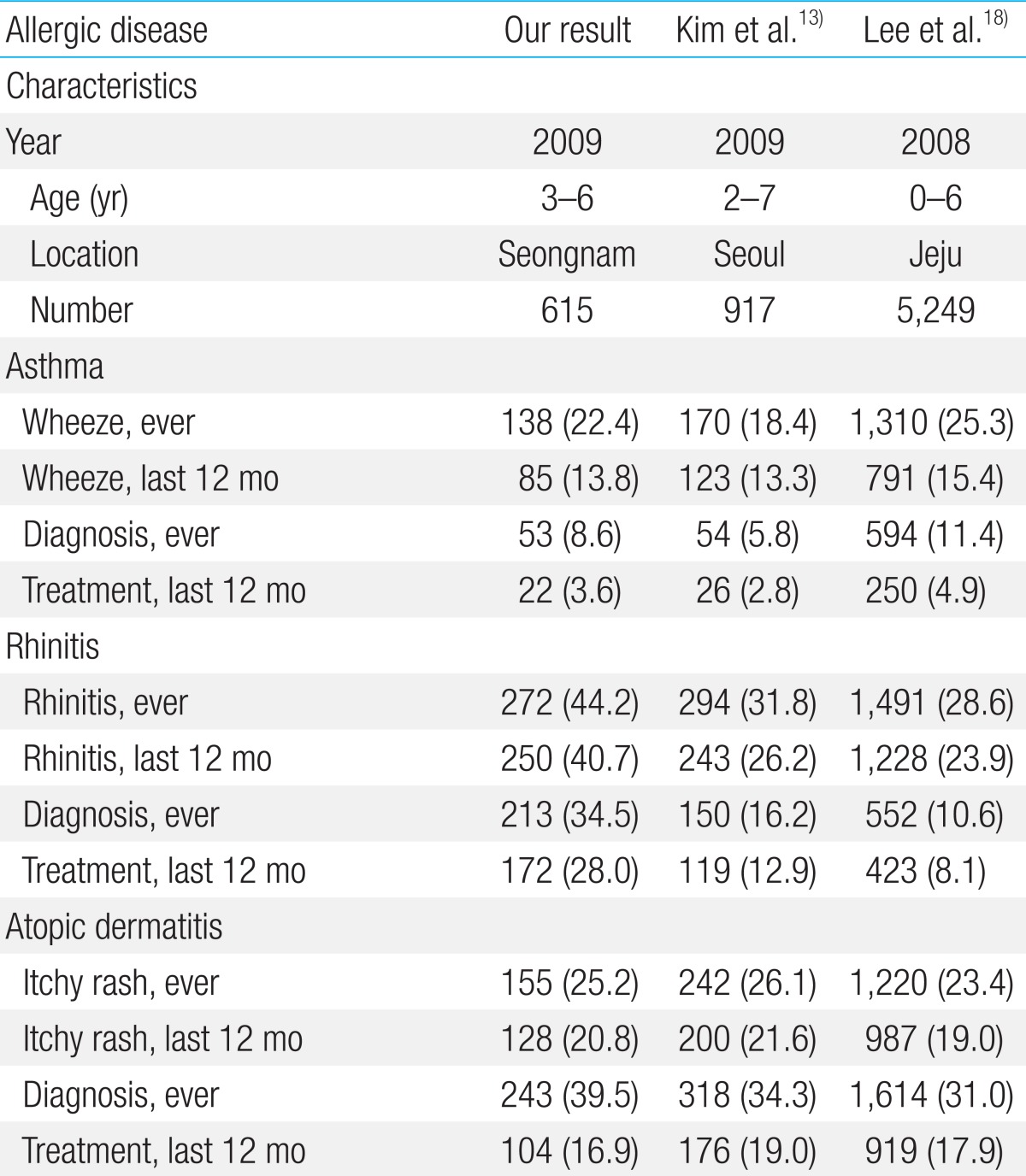
The prevalence of symptoms related to asthma, allergic rhinitis, and atopic dermatitis are presented in Table 2. The prevalence of current asthma, current allergic rhinitis, and current atopic eczema were 13.8%, 40.7%, and 20.8%, respectively. In addition, we compared these rates with those of previous studies from various regions of Korea. Specifically, the prevalence of current allergic rhinitis (40.7%) was higher in our study than in previous studies13,18).
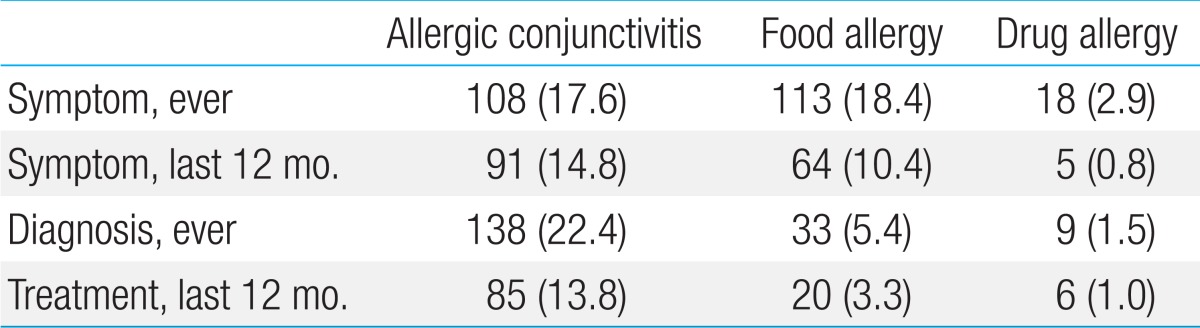
Table 3 presents the prevalence of symptoms related to allergic conjunctivitis, food allergy, and drug allergy, according to the positive answers to written questions per Hong et al.17). We could not compare our results with previous studies due to a lack of data on allergic conjunctivitis, food allergy, and drug allergy in preschool children using the ISAAC questionnaire.
Comorbidity of wheezing, rhinitis, and conjunctivitis was assessed by 'In the last 12 months, has your child had symptoms?' (symptom, last 12 months). Of the 615 subjects, 292 (47.5%) had current symptoms of wheezing, rhinitis, and conjunctivitis. The comorbidity of each allergic disease is shown in Fig. 1. In 138 subjects with 'wheeze, current' the prevalence of 'rhinitis, current' was 64.3% (54 subjects). In 91 subjects with 'itchywatery eyes, current', 'wheeze, current' was combined in 23 (25.3%) and 'rhinitis, current' in 59 (64.8%). Conversely, in 250 subjects with 'rhinitis, current', 'itchy-watery eyes, current' was combined in 23.6% versus 21.6% with 'wheeze, current'.
We investigated the prevalence of allergic diseases and their comorbidities in Korean preschool children and found that asthma and other allergic diseases often coexist in preschool children, a finding consistent with previous studies14,19). We also found that preschool children in Seongnam have higher prevalence of allergic rhinitis compared with previous studies13,17,18,20).
Allergic rhinitis and asthma share common and possibly linked pathophysiology and thereby frequently coexist7-10,19). The prevalence of 'wheeze, current' was combined in 64.3% of 'rhinitis, current' subjects, which was similar to a previous study14). Conversely, the prevalence of 'rhinitis, current' was combined in 21.6% of 'wheeze, current' subjects. Further, the prevalence of allergic conjunctivitis was 27.4% of 'current wheeze' and 23.6% of 'current rhinitis,' subjects-i.e., if a subject has airway symptoms, it is likely that he or she has concomitant allergic inflammatory responses in other parts of the body, namely conjunctival surfaces21). The ISAAC study also demonstrated that there is a close correlation between asthma and allergic rhinoconjunctivitis4,22). Furthermore, the presence of comorbidities of allergic diseases may aggravate symptoms. Assessing the comorbidities of allergic diseases may help clinicians recognize allergic symptoms early and prompt treatment. These findings have important clinical implications because the prevalence of allergic disease in preschool children is on the rise. Thus, the prevalence of allergic conjunctivitis should be assessed in preschool children with allergic symptoms, because asthma and allergic rhinitis often coexist19,21).
The prevalence and risk factors for allergic diseases can be compared between age groups and different regions through a standardized epidemiological study of the ISAAC3,4). The prevalence of 'wheeze, last 12 months' was 13.8%, which is lower than that (12.8% to 22.2%) in children in Western countries in the ISSAC phase III3,13) and is similar to that of preschool children in Korea13,18). The prevalence of 'wheeze, last 12 months' in the present study (13.8%) was higher compared with that in a previous study of school children (4.7% to 4.9%)17,20), possibly due to the fact that we could not completely exclude transient wheezers in the preschool period23,24). This assumption was confirmed by the finding that 'wheeze, last 12 months' (13.8%) was higher than the rate of 'treatment, last 12 months' (3.6%).
The large variations in the worldwide prevalence of symptoms of allergic diseases were recorded, even in genetically similar groups3-5). Also, our results showed that the prevalence of 'rhinitis, last 12 months,' 40.7%, was higher in our study than for children in Taiwan (24.2%) and New Zealand (11.4%)3), as well as for preschool children (23.9% to 26.2%) and children aged 6 to 13 years from different regions of Korea (29% to 33%)13,17-18,20). These differences, despite identical genetic predispositions, could be attributed to the finding that the prevalence of allergic diseases is influenced by environmental factors, such as air pollution, and factors related to social status, such as housing25,26). Further research on air pollution and economic indices in subjects is needed to determine the effect of these factors on the prevalence of allergic diseases. Previous studies in Korea reported the risk factors for allergic diseases in children to be presence of a history of other allergic disease, parental history of allergic diseases, dwelling pattern, indoor humidity, number of family members, cesarean delivery, use of antibiotics, and a history of bronchiolitis13,18). These factors and the response error of the questionnaire may have influenced the prevalence of rhinitis.
The prevalence of 'itchy rash, last 12 months' in our study was 20.8%, similar to previous studies (21% to 22%)13,27). The prevalence of 'itchy-watery eye, last 12 months' was 15%, lower than in the general population (20% to 40%)28) and approximating that in preschool children (11% to 19%)29,30). Our study demonstrated that the prevalence of allergic conjunctivitis in 292 children with current allergic diseases was 31.2%, close to the rate of ocular allergy (32%)28). The prevalence of allergic rhinoconjunctivitis (20.2%, 59 subjects) in this current symptomatic group was similar to that in the ISAAC phase III study (2.2% to 24.2%) in children aged 6 to 7 years3,13).
The limitations of our study are that 1) it does not represent the entire Korean preschool population; 2) we used the ISAAC questionnaire for preschool children, although it was originally designed for primary and middle school children; 3) there was a wide range of ages of the subjects; 4) allergic conjunctivitis, food allergy, and drug allergy were diagnosed using an unconfirmed ISAAC questionnaire, which we speculated could be used in population-based epidemiological studies; and 5) we investigated the prevalence of current allergic disease using the current allergic symptoms on questionnaire. Our method could not reflect the accurate prevalence of allergic disease than physician-diagnosed allergic disease. But, the prevalence of current allergic symptoms was commonly used to compare the trend of prevalence of allergic disease in worldwide ISAAC studies. Despite these limitations, our results merit attention, because there are little data on the prevalence of allergic diseases in this age group. Further research is warranted to determine the prevalence of allergic diseases in the entire Korean preschool population using valid questionnaires.
In conclusion, preschool children in Seongnam have a higher prevalence of allergic rhinitis and a similar prevalence of the other allergic diseases compared with previous studies. The prevalence of allergic conjunctivitis is relatively high in preschool children and even higher in preschool children with asthma and allergic rhinitis. Our data build on previous work, by suggesting that there is a substantial proportion of preschool children with concomitant allergic diseases.
Acknowledgments
The Korean version of ISAAC was provided by the Korean Pediatric Allergy and Respiratory Society.
References
1. Aberg N, Hesselmar B, Aberg B, Eriksson B. Increase of asthma, allergic rhinitis and eczema in Swedish schoolchildren between 1979 and 1991. Clin Exp Allergy 1995;25:815–819.


2. Lundback B. Epidemiology of rhinitis and asthma. Clin Exp Allergy 1998;28(Suppl 2): 3–10.
3. Asher MI, Montefort S, Bjorksten B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet 2006;368:733–743.


4. The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet 1998;351:1225–1232.


5. Ahn K, Kim J, Kwon HJ, Chae Y, Hahm MI, Lee KJ, et al. The prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in Korean children: nationwide cross-sectional survey using complex sampling design. J Korean Med Assoc 2011;54:769–778.

6. Spergel JM, Paller AS. Atopic dermatitis and the atopic march. J Allergy Clin Immunol 2003;112(6 Suppl): S118–S127.


7. Lack G. Pediatric allergic rhinitis and comorbid disorders. J Allergy Clin Immunol 2001;108(1 Suppl): S9–S15.


8. Rondon C, Romero JJ, Lopez S, Antunez C, Martin-Casanez E, Torres MJ, et al. Local IgE production and positive nasal provocation test in patients with persistent nonallergic rhinitis. J Allergy Clin Immunol 2007;119:899–905.


9. Gaugris S, Sazonov-Kocevar V, Thomas M. Burden of concomitant allergic rhinitis in adults with asthma. J Asthma 2006;43:1–7.


10. Casale TB, Amin BV. Allergic rhinitis/asthma interrelationships. Clin Rev Allergy Immunol 2001;21:27–49.


11. Meltzer EO, Blaiss MS, Derebery MJ, Mahr TA, Gordon BR, Sheth KK, et al. Burden of allergic rhinitis: results from the Pediatric Allergies in America survey. J Allergy Clin Immunol 2009;124(3 Suppl): S43–S70.


12. Yuksel H, Dinc G, Sakar A, Yilmaz O, Yorgancioglu A, Celik P, et al. Prevalence and comorbidity of allergic eczema, rhinitis, and asthma in a city in western Turkey. J Investig Allergol Clin Immunol 2008;18:31–35.

13. Kim YH, Urm SH, Kim WK. Prevalence of allergic diseases and risk factors in preschool children, 2009. Pediatr Allergy Respir Dis 2011;21:165–175.

14. Kocabas CN, Civelek E, Sackesen C, Orhan F, Tuncer A, Adalioglu G, et al. Burden of rhinitis in children with asthma. Pediatr Pulmonol 2005;40:235–240.


15. Bertelsen RJ, Carlsen KC, Carlsen KH. Rhinitis in children: comorbidities and phenotypes. Pediatr Allergy Immunol 2010;21(4 Pt 1): 612–622.


16. Choi SW, Ju YS, Kim DS, Kim JY, Kwon HJ, Kang DH, et al. Reliability and validity of the Korean version of ISAAC questionnaire. Korean J Prev Med 1998;31:361–371.
17. Hong SJ, Ahn KM, Lee SY, Kim KE. The prevalences of asthma and allergic diseases in Korean children. Pediatr Allergy Respir Dis 2008;18:15–25.
18. Lee HS, Lee J, Hong SC, Kim JW, Kim SY, Lee KH. Prevalence and risk factors for allergic diseases of preschool children living in Seogwipo, Jeju, Korea. Korean J Asthma Allergy Clin Immunol 2012;32:107–114.
19. Bousquet J, Van Cauwenberge P, Khaltaev N. Aria Workshop Group. World Health Organization. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol 2001;108(5 Suppl): S147–S334.


20. Jee HM, Kim KW, Kim CS, Sohn MH, Shin DC, Kim KE. Prevalence of asthma, rhinitis and eczema in Korean children using the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaires. Pediatr Allergy Respir Dis 2009;19:165–172.
21. Rosario N, Bielory L. Epidemiology of allergic conjunctivitis. Curr Opin Allergy Clin Immunol 2011;11:471–476.


22. Strachan D, Sibbald B, Weiland S, Ait-Khaled N, Anabwani G, Anderson HR, et al. Worldwide variations in prevalence of symptoms of allergic rhinoconjunctivitis in children: the International Study of Asthma and Allergies in Childhood (ISAAC). Pediatr Allergy Immunol 1997;8:161–176.


23. Peroni DG, Piacentini GL, Bodini A, Rigotti E, Pigozzi R, Boner AL. Prevalence and risk factors for atopic dermatitis in preschool children. Br J Dermatol 2008;158:539–543.


24. Taussig LM, Wright AL, Holberg CJ, Halonen M, Morgan WJ, Martinez FD. Tucson Children's Respiratory Study: 1980 to present. J Allergy Clin Immunol 2003;111:661–675.


25. Zhao J, Bai J, Shen K, Xiang L, Huang S, Chen A, et al. Self-reported prevalence of childhood allergic diseases in three cities of China: a multicenter study. BMC Public Health 2010;10:551



26. Li F, Zhou Y, Li S, Jiang F, Jin X, Yan C, et al. Prevalence and risk factors of childhood allergic diseases in eight metropolitan cities in China: a multicenter study. BMC Public Health 2011;11:437



27. Oh JW, Kim KE, Pyun BY, Lee HR, Choung JT, Hong SJ, et al. Nationwide study for epidemiological change of atopic dermatitis in school aged children between 1995 and 2000 and kindergarten aged children in 2003 in Korea. Pediatr Allergy Respir Dis 2003;13:227–237.
28. Bielory L, Friedlaender MH. Allergic conjunctivitis. Immunol Allergy Clin North Am 2008;28:43–58.





 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


