Article Contents
| Korean J Pediatr > Volume 57(2); 2014 |
|
Abstract
Purpose
This study aimed to assess the characteristics of thyroid nodules among infants diagnosed with congenital hypothyroidism.
Methods
A retrospective study of 660 infants (374 males, 286 females) diagnosed with congenital hypothyroidism was carried out at the Pediatric Endocrine Clinic in Soonchunhyang University Hospital, Korea, between May 2003 and February 2013. The average age at diagnosis was 1.16±1.68 months.
Results
Of the 28 patients (4.2%) with thyroid nodules, 17 (2.6%) had cystic thyroid nodules and 11 (1.6%) had solid thyroid nodules. There were no significant differences in gender or age between congenital hypothyroidism patients who hadthyroid nodules and those who did not. All nodules were asymptomatic. The average age at diagnosis of congenital hypothyroidism with nodules was 1.42±1.39 months. All detected nodules measured less than 1 cm in diameter. Twenty-two of the 28 infants (78.6%) had only one nodule, while multiple nodules were found in 6 infants (21.4%). Of the 28 infants diagnosed with nodules, 16 underwent thyroid ultrasonography during follow-up and 8 of them (50%) showed no signs of nodules at thyroid ultrasonography.
Conclusion
The prevalence of thyroid nodules in infants with congenital hypothyroidism was 4.2%. Most thyroid nodules were small in size and benign, disappearing during follow-up observation. We therefore conclude that thyroid nodules in infants with congenital hypothyroidism can simply be observed and do not require direct treatment.
The frequency of thyroid nodules in adults was observed to be in the range of 2% to 6 % by palpation; through ultrasonography, the rates become 19% to 35% and from autopsy analysis, 8% to 65%1). Although the frequency of thyroid nodules in children and adolescents observed was 1.79%, the current investigation shows that a frequency from 0.2% to 5.1%, which is lower than that in adults1,2). The malignant rate of thyroid nodules is assumed to be 5% in adults and 25% in children. For this reason, a more aggressive approach is required for thyroid nodules found in children1,3,4,5,6). In children with congenital hypothyroidism due to dyshormogenesis or iodide organification defect, their risk of developing thyroid nodules increases, and changes from nodules to tumors can arise if the level of thyroid-stimulating hormone (TSH) increases for a long period of time due to inappropriate L-thyroxine treatment3,7).
There have been few reports on the frequency, characteristics or meaning of thyroid nodules associated with congenital hypothyroidism in children. Additionally, since there is no study on thyroid nodules in infants with congenital hypothyroidism, the present authors tried to determine the relationship between thyroid nodules and congenital hypothyroidism in infants.
The patient population comprised of infants, who were diagnosed with congenital hypothyroidism at the Pediatric Endocrine Clinic in Soonchunhyang University Hospital from May 2003 to February 2013. Children who visited the clinic had been sent from other departments of the primary, secondary, and tertiary hospitals when congenital hypothyroidism was suspected at the newborn screening test. Their average age when they were first diagnosed with congenital hypothyroidism was less than 12 months. All patients had treatment with L-thyroxine.
This study was an observational study, which incorporated a review of medical records in a retrospective manner. Patients' information on sex, age, type of congenital hypothyroidism, and symptoms associated with nodules was studied. All patients had thyroid ultrasonography at first visit. Thyroid ultrasonographic examinations were performed using 7- to 12-MHz linear transducers (ATL Ultramark 9, HDI 5000, IU-22, Philips, Bothell, WA, USA). The maximum diameter of nodules, the number of nodules (solitary nodule or multiple nodules), and the echogenicity and the locations of nodules were checked by thyroid ultrasonography. Nodules were divided into three groups by diameter: smaller than 0.5 cm, 0.5-0.9 cm, and equal or larger than 1 cm. Patients with thyroid nodules underwent thyroid ultrasonography every year. Patients without thyroid nodules underwent thyroid ultrasonography every 2-3 years for further evaluation to decide whether to discontinue medication.
All statistical analyses were performed with SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA), the Fisher exact test and Mann-Whitney U test were used to compare variables between both case and control groups. A value of P<0.05 was considered significant.
The study protocol was reviewed and approved by the Institutional Review Board (IRB) of the Soonchunhyang University Hospital (IRB No. 2013-025).
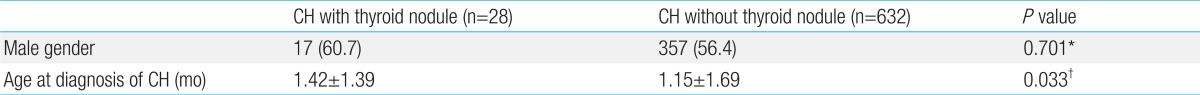
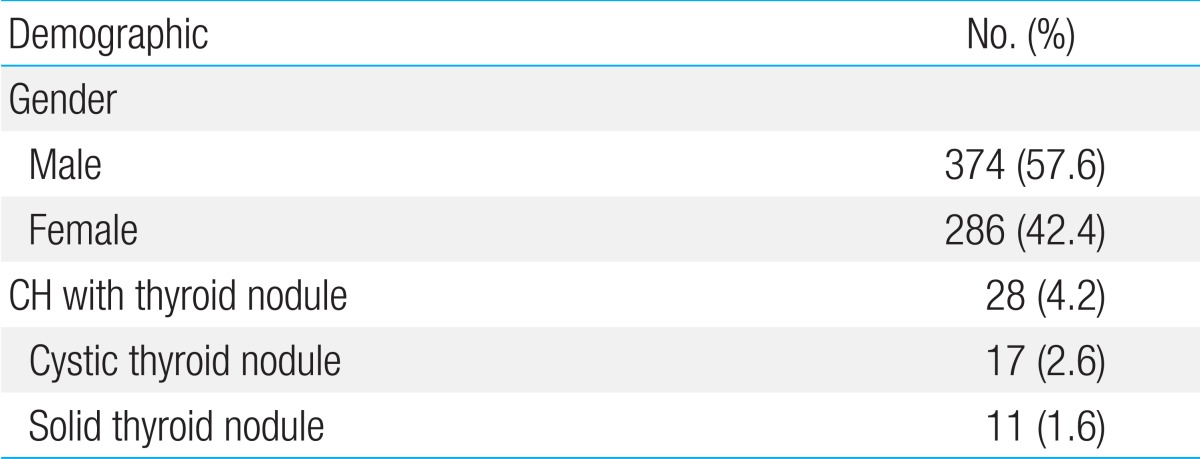
Among 660 patients, 374 were males and 286 were females. Their average age when they were first diagnosed with congenital hypothyroidism was 1.16±1.68 months. Average duration of observation of thyroid nodules in the participants was 3.91 years. Twenty-eight out of 660 patients (4.2%) had thyroid nodules, of whom, 17 (2.6%) had cystic thyroid nodules and 11 (1.6%) had solid thyroid nodules (Table 1). The ultrasonographic pattern of nodules was hyperechoic, isoechoic, or hypoechoic, and the pattern of cystic nodules was anechoic (Fig. 1). The number of male infants diagnosed with congenital hypothyroidism in the groups with and without thyroid nodule were 17 (60.7%) and 357 (56.4%), respectively. The average age of infants diagnosed with congenital hypothyroidism in the groups with and without thyroid nodule were 1.15±1.69 months and 1.42±1.39 months, respectively. There was no significant difference in gender between the two groups. However there was significant difference in age between the two groups (Table 2).
The average age at the time of congenital hypothyroidism diagnosis was 1.15±1.69 months. Among infants with thyroid nodules, there was not a single child who had a neck mass or showed symptoms related to thyroid nodules, including dysphagia, dysphonia, discomfort, and dyspnea caused by local compression. Among the 28 patients with thyroid nodule, 17 patients (2.6%) had cystic thyroid nodules and 11 (1.6%) had solid thyroid nodules. One patient in the group of cystic thyroid nodules had multiple thyroid nodules, which were multiple cystic nodules and one solid nodule. There were 22 infants (78.6%) with the maximal diameter of nodules of smaller than 0.5 cm, and 6 infants (21.4%) with the maximal diameter of the nodule of 0.5-0.9 cm; there was no nodule that was equal or larger than 1 cm. Regarding the number of nodules found through thyroid ultrasonography among 28 infants, solitary nodules were found in 22 infants (78.6%), and multiple nodules in six infants (21.4%). All solid nodules in 11 infants were solitary nodules. The location of nodules was the right lobe in 14 infants (50%), the left lobe in 10 infants (35.7%), and the bilateral lobe in four infants (14.3%). The types of congenital hypothyroidism were thyroid hypoplasia in 16 infants (57.2%), transient hypothyroidism in six infants (21.5%), congenital hypothyroidism by maternal antibodies in four infants (14.2%), and dyshormogenesis in two infants (7.1%). The size of cystic nodule was observed to be smaller than that of solid nodules (Table 3).
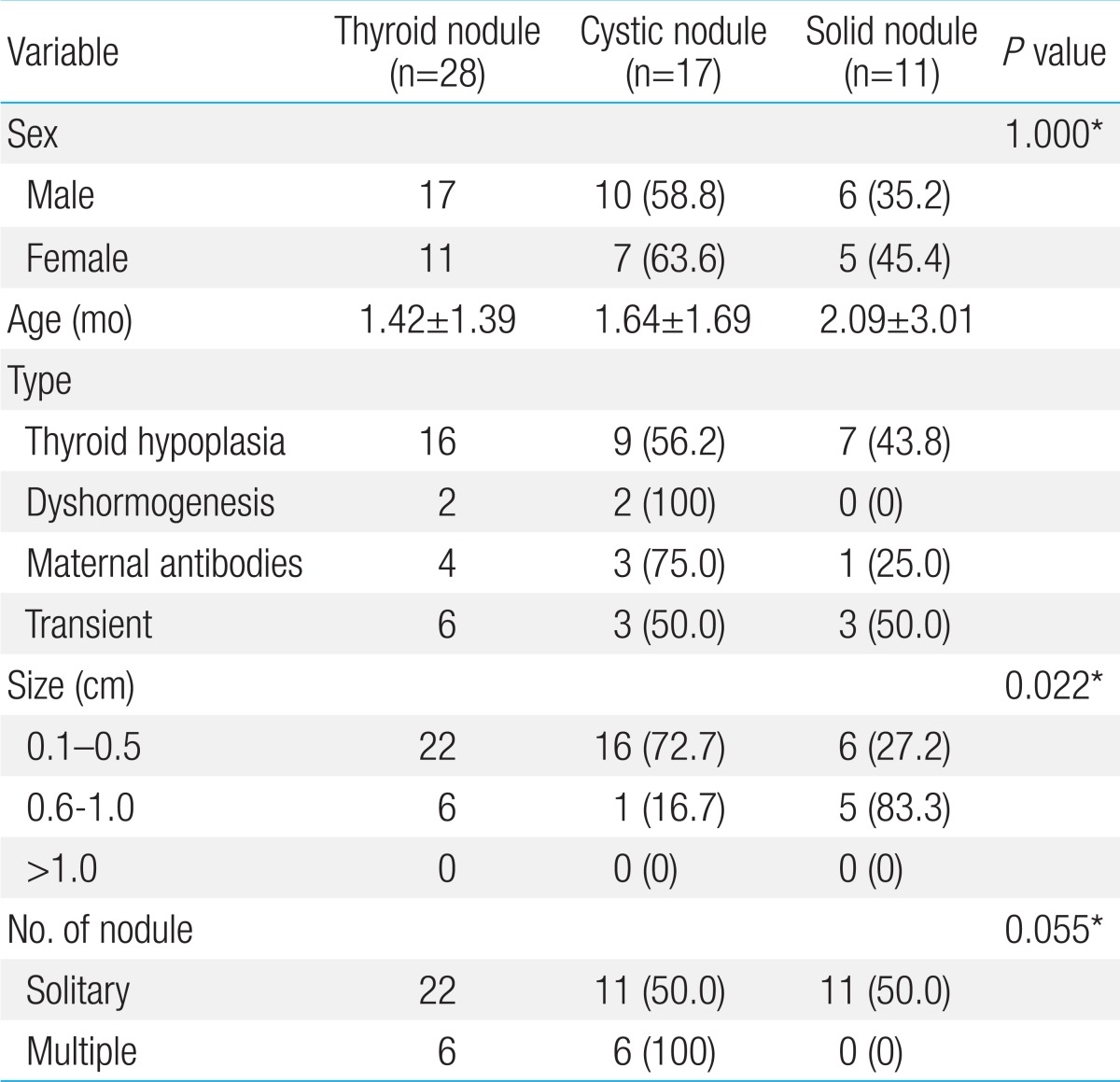
Patients with thyroid nodule underwent thyroid ultrasonography every year. Sixteen out of 28 infants with thyroid nodules underwent thyroid ultrasonography during the follow-up period. Average duration of observation of thyroid nodules in these infants was 3.75±1.29 years. Four hundred fifty-nine out of 632 infants with thyroid nodules underwent thyroid ultrasonography during the follow-up period (Fig. 2). The level of TSH returned to normal due to appropriate L-thyroxine treatment. No patient who showed symptoms related to thyroid nodules, including dysphagia, dysphonia, discomfort, and dyspnea during follow up.
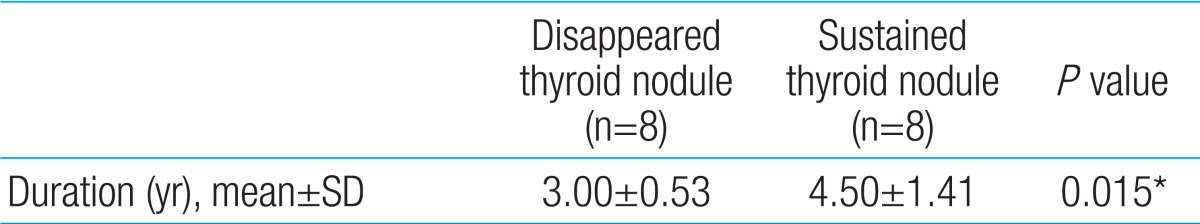
There were 12 infants who had less than1 year after the first visit, so they did not have thyroid ultrasound follow-up; thus, 16 out of 28 infants with thyroid nodules underwent follow up thyroid ultrasonography. Through this, it was verified that thyroid nodules in eight out of 16 infants (50%) disappeared. Average duration of observation of thyroid nodules in these infants was 3.00±0.53 years. Among these eight, seven nodules were disappeared by 1 year old and one nodule was disappeared by 2 years old. Thyroid nodules in eight out of 16 infants were sustained. Average duration of observation of thyroid nodules in these infants was 4.50±1.41 years. There was significant difference in duration between the two groups. Infants with sustained nodules had longer duration of observation than infants with disappeared nodules (Table 4).
Among the 16 infants, there were eight with cystic thyroid nodules. It was confirmed that five of these (62.5%) had their cystic thyroid nodules disappear, one infant (12.5%) showed a decrease in size, and two infants (25%) showed no change. Among the 16 infants, there were eight infants with solid thyroid nodules. It was confirmed through tracking observation that three infants' nodules (37.5%) disappeared and three infants (37.5%) showed no change. However, solid thyroid nodules in one infant changed into cystic thyroid nodules. Additional cystic thyroid nodules were found in one infant (Fig. 3).
Among the 16 infants who had follow up, 12 had maximal nodule diameter of smaller than 0.5 cm. It was confirmed that those nodules in six infants (50%) disappeared, and one infant (8.3%) showed a decrease in size. Four infants had the maximal diameter of the nodules of 0.5-0.9 cm. It was confirmed that those nodules in two infants (50%) disappeared. Among the 16 infants, there were three with multiple thyroid nodules. It was confirmed that multiple thyroid nodules in two infants (66.7%) disappeared and a decrease in size was shown in one infant (33.3%). Among the 16 infants, there were 13 with solitary thyroid nodules. It was confirmed through tracking observation that six infants (46.1%) had their nodules disappear, five infants (38.5%) showed no change, one infant (7.7%) showed a cystic change, and one infant (7.7%) was found to have an additional nodule.
Out of all 660 infants, 459 did not have thyroid nodules. Among those 459 infants, 286 infants, had thyroid ultrasound follow-up (173 infants had less than 2 years after their first visit, so they did not have thyroid ultrasound follow-up). Of the 286 infants, eight had their thyroid nodules found in thyroid ultrasonography during follow-up, although their thyroid ultrasonography results were normal during infancy (Fig. 2). Average duration of observation of thyroid nodules in these infants was 6.25±2.05 years. There were cystic thyroid nodules in seven infants and solid thyroid nodules in one infant. Among these eight, four were 5 years old, two were 3 years old, and two were 2 years old. Among these eight, three infants had follow up thyroid ultrasonography: thyroid nodules disappeared in two infants, and the size of the thyroid nodule in one infant decreased. One nodule was found with a patient aged was 2 years old which disappeared by 5 years old. The other nodule was found when the patient was 3 years old and disappeared by 4 years old. Another nodule was found when the patient was 6 years old and had decreased by 7 years old.
The prevalence of thyroid nodules detected by thyroid ultrasonography was 4.2% in the results of a study conducted between May 2003 and February 2013 in infants with congenital hypothyroidism. Compared with the present study, Corrias et al.8) reported prevalence of thyroid nodules in 365 juvenile autoimmune thyroiditis case series of 31.5%, and prevalence of thyroid cancer of 3.0%.
In this study, there was significant difference in age between the groups with and without thyroid nodule. However only 28 patients (4.2%) had nodules, which is very small group. In addition, one of them was 11 months old, which was much older than the other patients. Thus, even though there was significant difference in nodule presence with age, there is limitation in cohort size.
Thyroid nodules are classified into cystic type, mixed type, and solid type depending on the internal conditions of the thyroid nodule. Although it has been known that the portion of cystic thyroid nodules among all thyroid nodules perceived by palpitation comprise 15%-30%, many thyroid nodules among all the thyroid nodules not perceived by palpitation were cystic type9,10,11). In this study, the result showed that the portion of cystic thyroid nodules in infants with congenital hypothyroidism was 60%. Changes to cystic nodules have frequently occurred through hemorrhagic degeneration of pre-existing solid thyroid nodules12). This study also showed that a solid thyroid nodule changed into a cystic thyroid nodule in one infant.
Although there are associated symptoms of thyroid nodules, including pain, dysphagia, dysphonia and dyspnea, these symptoms are not found in most children1,3). In this study, there were no infants with thyroid nodules who showed symptoms related to thyroid nodules (i.e., dysphagia, dysphonia, discomfort, and dyspnea by local pressure).
Studies on solitary thyroid nodules are common; however, studies on multiple thyroid nodules are rare. Additionally, theses studies do not distinguish multiple thyroid nodules from cystic and solid nodules. In our study, one infant with multiple thyroid nodules had multiple cystic nodules and one solid nodule. Patients with multiple thyroid nodules have the same risk of malignancy as those with a solitary nodule13,14). However, some studies found that thyroid multiple nodules are not common and not related to malignancy15,16). The present study also showed that in thyroid nodules found by ultrasonography in 28 infants with thyroid nodules, the number of single nodules (78.6%) was significantly larger than the number of multiple nodules (21.4%). This study also showed that multiple thyroid nodules in all infants who had ultrasonography during follow-up disappeared or decreased in size.
In thyroid or nonthyroid cervical diseases, the frequency of thyroid nodules found by chance during ultrasonography has increased3,11,17,18). Adults who have thyroid nodules less than 1.5 cm in size and have had no radiation exposure without any family history are recommended to have ultrasonography once a year. Many researchers emphasize that simple tracking observation is needed without further examination, because the malignancy rate for thyroid incidentalomas is as low as 0%-0.2%; the size of thyroid incidentalomas is usually small, and the lesions have a good prognosis of slow growth, despite the state of malignancy17,18,19,20,21,22,23).
While the frequency of malignancy of thyroid nodules in adults is 5%, its frequency in children is assumed to be 25%1,23). Although endocrine tumors in children are rare, 0.5%-3.0% of all childhood cancers are thyroid tumors1,23). In the United States, the incidence of thyroid cancer in 5- to 9-year-old children is one per million; in 10- to 14-year-old children, it is five per million; and in 15- to 19-year-old children it is 18 per million1,24).
Malignancy should be suspected if there is a familial history of thyroid cancer. Thyroid cancer is likely to be characterized by solitary solid lesion, hypoechogenic, subcapsular localization, irregular margins of the lesion, invasive growth, heterogeneous nature of the lesion, multifocal lesions within an otherwise clinically solitary nodule, microcalcifications, high intranodular flow by Doppler, or suspicious regional lymph nodes accompanying thyroid nodule by ultrasonography1,25). Therefore, aspiration is recommended for all thyroid nodules unless the lesion is completely cystic or autonomous by scintigraphic finding25).
When there are cases of children who have congenital hypothyroidism due to dyshormogenesis or iodide organification defect, thyroid cancer can arise if TSH is consistently increased due to inappropriate L-thyroxine treatment1,3,4,5,6,24). Therefore, it is thought that a more aggressive approach is needed for thyroid nodules found in children with congenital hypothyroidism. Fine-needle aspiration biopsy (FNAB) is recommended for thyroid nodules found in children and adolescents if the thyroid nodule is more than 1 cm in diameter or if its size is observed to increase. FNAB needs to be applied when the thyroid nodule is less than 1 cm in diameter; however, malignancy should be suspected clinically or in ultrasonography or the nodule that accompanies cervical lymph node enlargement1,16). In the present study, there were no cases of infants with congenital hypothyroidism in which FNAB was applied when the size of thyroid nodules was more than 1 cm in diameter with increasing size accompanied by cervical lymph node enlargement.
Infants with sustained nodules had longer duration of observation than infants with disappeared nodules. However it was verified that thyroid nodules disappeared in eight out of 16 infants (50%) who followed up among all 28 infants with thyroid nodules, and there were no cases that showed increasing size. Therefore, it can be concluded that incidental thyroid nodules can be observed in infants with congenital hypothyroidism.
In this study, thyroid nodules were founded in eight infants who did not have abnormal finding on initial ultrasonography. Among these eight, three infants had follow up thyroid ultrasonography, and thyroid nodules disappeared in two of these three (66%). Therefore, it can be concluded that their thyroid nodules can be observed. However, it is thought that further image study is recommended for the five infants who did not have follow up ultrasonography.
Consequently, in this study, the prevalence of thyroid nodules in infants with congenital hypothyroidism is 4.2%. Most thyroid nodules had a small size and were benign, disappearing during tracking observation. Because the patients of this study were infants with congenital hypothyroidism, further studies of infants without congenital hypothyroidism are still needed. However, the present is limited in terms of observation time period as well as cohort size.
References
1. Corrias A, Mussa A. Thyroid nodules in pediatrics: which ones can be left alone, which ones must be investigated, when and how. J Clin Res Pediatr Endocrinol 2013;5(Suppl 1): 57–69.




2. Wiersinga WM. Management of thyroid nodules in children and adolescents. Hormones (Athens) 2007;6:194–199.

3. Niedziela M. Pathogenesis, diagnosis and management of thyroid nodules in children. Endocr Relat Cancer 2006;13:427–453.


4. Ridgway EC. Clinical review 30: Clinician's evaluation of a solitary thyroid nodule. J Clin Endocrinol Metab 1992;74:231–235.


5. Canadian Pediatric Thyroid Nodule (CaPTN) Study Group. The Canadian Pediatric Thyroid Nodule Study: an evaluation of current management practices. J Pediatr Surg 2008;43:826–830.


6. Raab SS, Silverman JF, Elsheikh TM, Thomas PA, Wakely PE. Pediatric thyroid nodules: disease demographics and clinical management as determined by fine needle aspiration biopsy. Pediatrics 1995;95:46–49.



7. Chang YW, Lee DH, Hong YH, Hong HS, Choi DL, Seo DY. Congenital hypothyroidism: analysis of discordant US and scintigraphic findings. Radiology 2011;258:872–879.


8. Corrias A, Cassio A, Weber G, Mussa A, Wasniewska M, Rapa A, et al. Thyroid nodules and cancer in children and adolescents affected by autoimmune thyroiditis. Arch Pediatr Adolesc Med 2008;162:526–531.


9. McHenry CR, Slusarczyk SJ, Khiyami A. Recommendations for management of cystic thyroid disease. Surgery 1999;126:1167–1171.


10. Oh SK, Lee JY, Lee DH, Moon IH, Kwon KN, Park KN, et al. The utility of sono-guided sclerotherapy for benign thyroid cyst: prospective study. Korean J Otorhinolaryngol-Head Neck Surg 2012;55:777–781.

11. Kim EK, Park CS, Chung WY, Oh KK, Lee JT, Yoo HS. Incidentally found thyroid nodules in women with no previous thyroid disease: its significance. J Korean Radiol Soc 2002;46:449–453.

12. Lee SK, Kwon SY, Woo SK. Cystic change of thyroid mass: a useful sign in differentiating benign from malignant thyroid lesions? J Korean Soc Ultrasound Med 2007;26:33–40.
13. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009;19:1167–1214.


14. Marqusee E, Benson CB, Frates MC, Doubilet PM, Larsen PR, Cibas ES, et al. Usefulness of ultrasonography in the management of nodular thyroid disease. Ann Intern Med 2000;133:696–700.


15. Millman B, Pellitteri PK. Nodular thyroid disease in children and adolescents. Otolaryngol Head Neck Surg 1997;116(6 Pt 1): 604–609.

16. Frates MC, Benson CB, Doubilet PM, Kunreuther E, Contreras M, Cibas ES, et al. Prevalence and distribution of carcinoma in patients with solitary and multiple thyroid nodules on sonography. J Clin Endocrinol Metab 2006;91:3411–3417.


17. Ezzat S, Sarti DA, Cain DR, Braunstein GD. Thyroid incidentalomas. Prevalence by palpation and ultrasonography. Arch Intern Med 1994;154:1838–1840.


18. Castro MR, Gharib H. Continuing controversies in the management of thyroid nodules. Ann Intern Med 2005;142:926–931.


19. Carroll BA. Asymptomatic thyroid nodules: incidental sonographic detection. AJR Am J Roentgenol 1982;138:499–501.


20. Brander A, Viikinkoski P, Nickels J, Kivisaari L. Thyroid gland: US screening in a random adult population. Radiology 1991;181:683–687.


21. Miki H, Inoue H, Komaki K, Uyama T, Morimoto T, Monden Y. Value of mass screening for thyroid cancer. World J Surg 1998;22:99–102.


22. Tan GH, Gharib H. Thyroid incidentalomas: management approaches to nonpalpable nodules discovered incidentally on thyroid imaging. Ann Intern Med 1997;126:226–231.


23. Goldfarb M, Gondek SS, Sanchez Y, Lew JI. Clinic-based ultrasound can predict malignancy in pediatric thyroid nodules. Thyroid 2012;22:827–831.


Fig. 1
Transverse scan image of the thyroid gland. (A) A 0.3 cm anechogenic cyst is seen in the right lobe of the thyroid gland. (B) An incidentally detected 0.4 cm hypoechogenic nodule is seen in the left lobe of the thyroid gland. (C) A 0.5 cm isoechogenic nodule with a peripheral low echogenic rim is seen in the left lobe of the thyroid gland. (D) Hypoechogenic multiple nodules is seen in the left lobe of the thyroid gland.
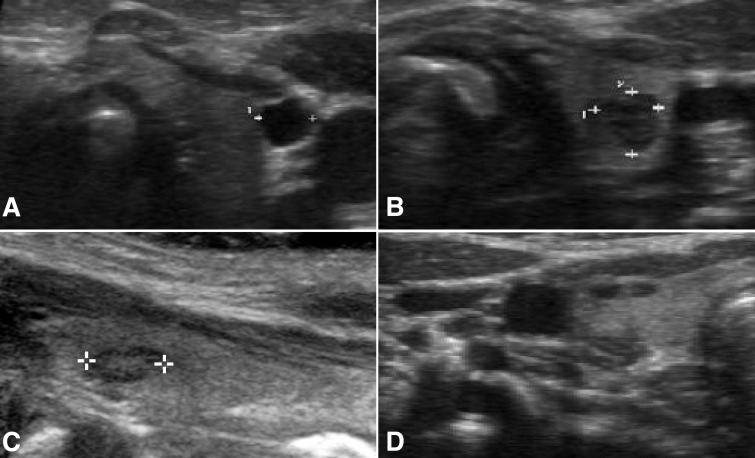
Fig. 2
Diagram showing the results of thyroid ultrasonography in all infants with congenital hypothyroidism. Sixteen of 28 infants with thyroid nodules underwent thyroid ultrasonography during follow-up. Of 632 infants without thyroid nodules, 459 underwent thyroid ultrasonography during follow-up. New nodules were found in 8 of these infants, although their thyroid ultrasonography results were normal during infancy.
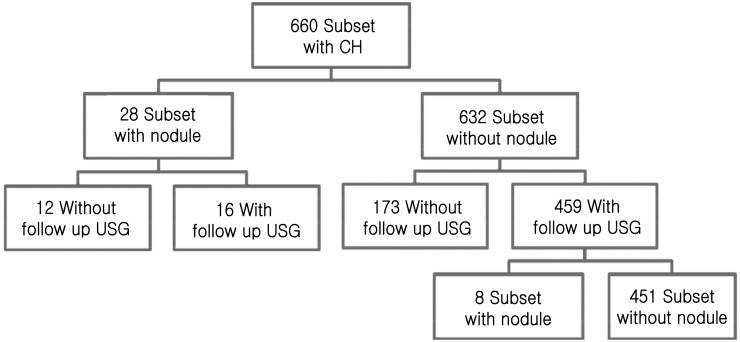
Fig. 3
Thyroid ultrasonography at follow-up. Sixteen of 28 infants with thyroid nodules underwent thyroid ultrasonography during follow-up. Thyroid nodules in 8 infants were not observable at follow-up ultrasonography. A decrease in size was detected in 1 infant, and no change was seen in 5 infants. There was a cystic change in 1 infant with a solid nodule. A new cystic nodule was found in 1 infant.
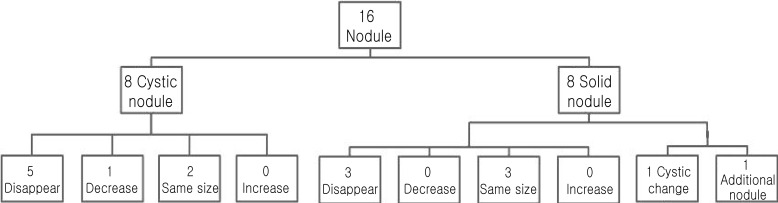
Table 2
Differences between patients diagnosed with congenital hypothyroidism with thyroid nodules and those diagnosed with congenital hyperthyroidism without thyroid nodules



 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


