Article Contents
| Korean J Pediatr > Volume 56(5); 2013 |
Abstract
Purpose
The aim of this study was to recognize the state of vitamin D among healthy infants aged 1 to 6 months in South Korea, and also to identify the risk factors affecting the level of vitamin D.
Methods
A total of 117 infants were enrolled in this study for 12 months, from March 1, 2011 to February 29, 2012. Serum levels of 25-hydroxyvitamin D (25[OH]D), calcium, phosphorus, and alkaline phosphatase were measured and data including birth weight, body weight, sex, feeding pattern, delivery mode, siblings and maternal age and occupation were collected. Data was mainly analyzed with independent t-test model.
Results
We determined that the prevalence of vitamin D deficiency (serum 25[OH]D<20 ng/mL [50 mmol/L]) was 48.7% in the population investigated. Particularly in breastfed infants, the prevalence of vitamin D deficiency was strikingly high (90.4%). The mean serum level of 25(OH)D in breastfed infants was lower than that of formula fed infants (9.35 ng/mL vs. 28.79 ng/mL). Also female infants showed lower mean serum level of 25(OH)D than male. Mean serum values of calcium and phosphorus had positive correlation with vitamin D state (P<0.001).
Conclusion
Vitamin D deficiency was found to be very common in infants aged 1 to 6 months in South Korea, and breast feeding was the most critical risk factor of vitamin D deficiency. Therefore we suggest to start vitamin D supplementation in South Korea, as soon as possible, to all infants, including breastfed and female infants.
Vitamin D is a fat-soluble vitamin that performs a key role in calcium homeostasis and bone metabolism1). In particular, vitamin D deficiency induced disorders such as rickets or osteomalacia are able to arrest normal growth and the development of infancy and childhood, and vitamin D has been currently known to influence the extraskeletomuscular system as well as the immune system1,2). Therefore, there has been a growing interest in vitamin D deficiency and its supplementation1-3). Currently, previous reports that presented a high prevalence of vitamin D deficiency of exclusively breastfed infants have aroused public opinions about how aggressive vitamin D supplement needs to be for breastfed infants1, 4-8).
However there are not any generalized statistical data of vitamin D measurement in normal babies and few comparing studies of vitamin D level between breastfed and formula-fed groups, so it is difficult to give straight answers for vitamin D deficiency of breast-fed or formula milk fed infants and an efficient method of supplementation for them. Recently, a large study in the United States (US) noticed that 9% of the pediatric population were vitamin D deficient and 61% were 25(OH)D insufficient9). In the case of East Asia, according to small-scale studies of Asian nations, 31.2% to 57.8% of Chinese adolescent girls, and 76% of Mongolian children were in a state of vitamin D insufficiency10,11). In case of South Korea, there are few reports of vitamin D state of the pediatric population and measuring value of vitamin D, particularly of asymptomatic infants or children, except a recent report that presented 29.8% of Korean children under 2 years old for vitamin D deficiency12,13). But taking into account the sporadic reports of subclinical rickets, vitamin D deficiency and hypocalcemia induced seizure14-16), it is necessary to investigate the probability of vitamin D deficiency or insufficiency of even healthy-looking infants. Besides, when considering the geographical position at the middle latitudes, Mongolian race and cultural traits like swaddling clothes, known risk factors of rickets, pediatric population in South Korea are suggested to be regarded as a high risk group of vitamin D deficiency or insufficiency with constantly increasing breast milk feeding1,8). Therefore we performed this study to determine the vitamin D state of normal Mongolian infants aged 1 to 6 months in Seongnam, South Korea (37N), and to identify the correlating factors with vitamin D deficiency using a questionnaire survey and analyzing data on laboratory findings.
Our study was performed for 12 months, from March 1, 2011 to February 29, 2012. A total of 161 infants participated in this study, among Mongolian infants aged 1 to 6 months who visited pediatric department of CHA Bundang Medical Center. All infants were taken past history and received physical examination by pediatricians. At the time of laboratory testing, admitted patients, drug using condition and cases of visiting for specific symptoms due to infection or other underlying disease (tumor, cholestasis, jaundice, hepatitis, diabetes mellitus) were excluded, and sampling failure, incomplete questionnaires, preterm babies, babies that had taken vitamin D supplements, or feeding on baby foods were also excluded. Breast milk feeding was defined as feeding breast milk more than 80% of total feeding volume per day. Finally 117 infants enrolled in our study, 57 breast milk feeding infants and 60 formula milk feeding infants. No special consideration was given to cow's milk formula, goat's milk formula, or specialized milk formula. This study was approved by the Institutional Review Board of Medical Faculty at the CHA university.
To collect demographic variables influencing vitamin D state such as age, birth weight, body weight at sampling, delivery mode, feeding pattern, season at birth and sampling, the presence of sibling, and maternal age and occupation during pregnancy were investigated by questionnaire filled out by parent.
Blood measurement of serum 25(OH)D, calcium, phosphorus, and alkaline phosphatase (ALP) was performed on subjects with permission by skilled samplers. Vitamin D deficiency was defined as serum 25(OH)D<20 ng/mL (50 mmol/L), and vitamin D sufficiency defined as ≥20 ng/mL in our study17-19). The level of serum 25(OH)D was quantitatively determined with chemiluminescent immunoassay. Also measurement of serum parathyroid hormone and wrist X-rays were carried out with further permission following notice for initial laboratory findings.
In our study, all continuous variables were indicated as mean values with standard deviation (SD) and were analyzed for correlation with vitamin D deficiency using independent t-test model. Chi-square test, correlation anaylsis and one-way analysis of variance were utilized between dichotomous variables and vitamin D state. Our data was analyzed by IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA) then statistical significance was considered at P value <0.05, for all statistical analyses.
The demographic and clinical characteristics of 117 study participants are shown in Table 1.
Sixty-four infants of the subjects (53.7%) were male and 53 infants (46.3%) were female. The mean values (±SD) of their age and birth weight were 4.00±1.57 months and 3.13±0.50 kg. The proportion of infants that had been breastfed was 44.4% of our subjects and the rest (55.6%) were fed with formula milk. Mean serum level of 25(OH)D in total sample was 20.15±13.14 ng/mL. Overall, 57 of infants (48.7%) had serum 25(OH)D level lower than 20 ng/mL in our study.
Table 2 shows the differences in distribution of characteristics between vitamin D deficient group and sufficient group. The mean serum level of 25(OH)D were 8.15 ng/mL and 31.55 ng/mL in each group (P<0.001). Correlating with sex and vitamin D state, male infants were predominant in sufficient group, and vice versa in deficient group (P=0.01). And male infants had a higher mean serum level of 25(OH)D than female infants (23.40±13.27 ng/mL, 16.23±11.95 ng/mL, P=0.003). This tendency between two sexes was shown to be similar in each vitamin D deficient and sufficient group.
Almost breastfed infants (47/52, 90.4%) had serum 25(OH) D level below 20 ng/mL, but 15.4% of formula fed infants was revealed to vitamin D deficiency. Trying to correlate mean serum level of 25(OH)D with feeding pattern, the mean serum level of 25(OH)D of breast fed infants was lower compared to formula fed infants (P<0.001). Furthermore this finding was shown even in vitamin D sufficient group.
None of multivariables such as delivery mode, birth weight, body weight at sampling, season at birth and sampling, the presence of siblings, and mother's occupation during pregnancy affected the vitamin D deficiency, except maternal age. Total mean value of maternal age of the subjects was 31.33±3.86 years, and the mean value of maternal age was statistically younger in vitamin D deficient group than vitamin D sufficient group (P=0.008). Also mean maternal age of breast fed infants was younger than formula fed infants (30.71±4.10 years vs. 31.83±3.62 years), although there was no significant correlation between two groups (P=0.051).
The mean serum levels of calcium, phosphorus, or ALP were 10.24±0.43 mg/dL, 5.63±0.71 mg/dL or 717.06±244.04 IU/L, respectively. There was statistical significance between the vitamin D state groups with regards to calcium and phosphorus levels (P<0.001). The mean values of serum ALP were 752±262.41 IU/L and 683±222.21 IU/L in each group, but there was no statistical difference (P=0.13).
Following the initial laboratory examination, 20 infants among the vitamin D deficient group (n=57) were examined for serum levels of parathyroid hormone during this study period with further parental agreement. Mean serum value of parathyroid hormone in these subjects was 32.88±27.75 pg/mL. Multiple regression analysis and correlation analysis did not show positive correlations with serum parathyroid hormone, 25(OH)D, calcium, phosphorus and ALP. Two infants with extremely low level of serum 25(OH)D, however, presented an abnormally increased level of serum parathyroid hormone (Pearson; P=0.051) (Fig. 1).
Subsequently, 13 vitamin D deficient infants who were enrolled in this study took an X-ray of the wrist to diagnosis rickets with further permission. And then 3 infants among these subjects were diagnosed with subclinical rickets.
Our study shows that there is a high prevalence of vitamin D deficiency of infants aged 1 to 6 months in South Korea, especially exclusive breast milk feeding infants. Mean serum level of 25(OH)D in total subjects was 20.15±13.14 ng/mL, which is very close to the cut-off value for vitamin D deficiency. The proportion of serum level of 25(OH)D <20 ng/mL among our subjects was 48.7% (57/117), and breastfed infants were revealed to be 47 persons, which amounted to 82.5% of the vitamin D deficient group in this study. These findings means there is a significant correlation between feeding pattern and vitamin D deficiency, in line with previous studies8,20-22).
Breastfed infants had lower level of serum 25(OH)D, on average, than formula milk feeding infants even if they were in the vitamin D sufficient group. However it was not true that formula milk feeding is sufficient to overcome the vitamin D deficiency.
Consistent with the previous researches, we found that the serum levels of 25(OH)D were lower in female than in male. But the reasons proposed by other studies, that boys tended to spend longer periods of time outdoors with less frequent use of sunscreen23-26), were not appropriate for our results. Our subjects were 1 to 6 months aged infants, who live indoors all day long, regardless of sex27). In this situation, this difference between two sex was so notable that it needs to recognize other influencing factor in the following study.
Other demographic variables in this study, such as age, delivery mode, weight at birth and study, season at birth and study, and the presence of siblings and mother's occupation during pregnancy, did not have any significance for vitamin D state. Although a previous study reported that the mean serum level of 25(OH)D was the lowest in spring for infants under 1 year old20,28), we did not find any significant differences among four seasons. Our subjects were enough young to keep indoors all day long, irrespective of the season, so it is unlikely for specific seasonal change to be an influential factor. With regard to maternal age, our study showed a different tendency from previous reports29-31), in that the younger the maternal age, the more prevalent was breast milk feeding. Therefore it is natural that younger mother with breast milk feeding had a higher prevalence of vitamin D deficiency in our subjects. To prove a definite correlation between maternal age and vitamin D state, however, requires further large scaled studies.
We also found that serum 25(OH)D level had a positive relationship with serum calcium and phosphorus. Both of serum calcium and phosphorus were known to be sensitive to vitamin D deficiency, and especially a previous study presented that hypophosphatemia at vitamin D deficient state was related to muscle weakness of rachitic patients32). Serum ALP generally tends to increase in infancy, therefore serum ALP was less effective to screen vitamin D deficiency in early infancy like our subjects, limited to 1-6 months age ,but seen as a sensitive marker of rickets1,3,33-36).
We examined two further evaluations for vitamin D deficient infants in our study, serum parathyroid hormone and wrist X-ray for checking secondary hyperparathyroidism and subclinical rickets. Several previous studies reported the association between vitamin D deficiency and abnormally increased parathyroid hormone level reading to bone loss34,37,38). As a result, there was no more correlation with vitamin D deficiency in our study, but we assumed that it was from sample limitation, due to further agreement or following loss.
In the US, the American Academy of Pediatrics (AAP) has recommended a vitamin D supplement of 400 IU/day for both breast milk fed infants and nonbreast milk fed infants starting at infancy to childhood and adolescence, and Canada has required vitamin D fortification for milk products such as milk or butter1,8). In South Korea, however, there has not been any public recommendation for vitamin D supplement for infancy, even no definite standard of vitamin D deficiency, and few statistical data of vitamin D at infancy exist13). However South Korea is situated at midlatitude in the northern hemisphere, and in particular, the amount of sunlight changes seasonally. More and more Korean infants, children and adolescents, not just adults, now use sunscreen from spring to winter in recent years. Most importantly, breast feeding has been increased by many mothers with a belief that breast milk is a perfect nutrient for babies, and some are even pressured to breastfeed 39,40). Moreover almost all babies tend to be kept indoors until 2 months and tend to be swaddled in clothes or blankets indoors due to old customs. These have resulted in interrupted exposure to the sunlight, the main source of vitamin D production in nature. Therefore many infants of South Korea are indicated to have a higher risk of vitamin D deficiency.
We believe that this study is the first research to provide the prevalent data of vitamin D deficiency of healthy infants before 6 months of age, and our study showed that the prevalence of vitamin D deficiency among them was much higher than other countries (48.7%). In this regard, we recommend to start the supplementation of vitamin D for infants, at least 400 IU/L which have been recommended by AAP and worldwidely1), and suggest it be considered for public policy. Vitamin D fortified milk products or foods also should be required.
However, our study also has several limitations. Firstly, almost all subjects have only been living in Seongnam city or Gyeonggi-do, in the middle part of South Korea; therefore the data cannot be assumed to be representative of the whole of South Korea. Moreover Seongnam is a city that has a population of almost 1 million people, so we suggest further study subjective to a population of a broader area including rural regions for appropriate population survey. Another limitation was that we did not consider poly-vitamin supplementation of lactating women or our infants. However almost poly-vitamin supplement is contained few dose of vitamin D below than vitamin D supplement, and may have insignificant effect on the vitamin D state of the subjects. Finally, although our effort to sort out healthy infants, undiagnosed clinical problem may influence the vitamin D state of subjects. Also we could not collect data with following up. Therefore it should perform following studies after vitamin D supplements with more strict subject selection and more detailed standard of vitamin D deficiency.
In conclusion, the prevalence of vitamin D deficiency among infants for 1 to 6 months in South Korea is very high, especially breast fed infants and female. Despite formula feeding, some cases are deficient for vitamin D, so that means the requirement of vitamin D supplement for formula-fed infants. There has been no policy for vitamin D fortification of any formulas or milk products in South Korea, and the foods containing vitamin D naturally, such as Atlantic herring or cod liver oil, are not common foods in South Korea, with the exception of shiitake mushrooms1). Consequently, we suggest vitamin D supplementation to infants of South Korea, both breast-fed and formula-fed.
We also found that female was a significant predictor of vitamin D deficiency. A previous study recently presented a high prevalence of vitamin D deficiency or insufficiency in Korean adolescents, particularly in girls41). It means that the high prevalence of vitamin D deficiency will continue to pregnant women and lactating women. Therefore it is very important to start vitamin D supplementation in infancy, in order to prevent vitamin D deficiency for all ages. For that purpose, public policy on vitamin D supplementation, publicity on the necessity of vitamin D supplementation, and vitamin D fortified foods will all be needed simultaneously. Further collection of data and further research is also warranted.
References
1. Misra M, Pacaud D, Petryk A, Collett-Solberg PF, Kappy M. Drug and Therapeutics Committee of the Lawson Wilkins Pediatric Endocrine Society. Vitamin D deficiency in children and its management: review of current knowledge and recommendations. Pediatrics 2008;122:398–417.


3. Taylor JA, Richter M, Done S, Feldman KW. The utility of alkaline phosphatase measurement as a screening test for rickets in breastfed infants and toddlers: a study from the puget sound pediatric research network. Clin Pediatr (Phila) 2010;49:1103–1110.


5. Lawrence RA. Lower breastfeeding rates among supplemental nutrition program for women, infants, and children participants: a call for action. Pediatrics 2006;117:1432–1433.


6. Wagner CL, Howard C, Hulsey TC, Lawrence RA, Taylor SN, Will H, et al. Circulating 25-hydroxyvitamin D levels in fully breastfed infants on oral vitamin D supplementation. Int J Endocrinol 2010;2010:235035

7. Jain V, Gupta N, Kalaivani M, Jain A, Sinha A, Agarwal R. Vitamin D deficiency in healthy breastfed term infants at 3 months & their mothers in India: seasonal variation & determinants. Indian J Med Res 2011;133:267–273.


8. Ziegler EE, Hollis BW, Nelson SE, Jeter JM. Vitamin D deficiency in breastfed infants in Iowa. Pediatrics 2006;118:603–610.


9. Kumar J, Muntner P, Kaskel FJ, Hailpern SM, Melamed ML. Prevalence and associations of 25-hydroxyvitamin D deficiency in US children: NHANES 2001-2004. Pediatrics 2009;124:e362–e370.



10. Foo LH, Zhang Q, Zhu K, Ma G, Hu X, Greenfield H, et al. Low vitamin D status has an adverse influence on bone mass, bone turnover, and muscle strength in Chinese adolescent girls. J Nutr 2009;139:1002–1007.


11. Ganmaa D, Tserendolgor U, Frazier L, Nakamoto E, Jargalsaikhan N, Rich-Edwards J. Effects of vitamin D fortified milk on vitamin D status in Mongolian school age children. Asia Pac J Clin Nutr 2008;17:68–71.

12. Yoon JH, Park CS, Seo JY, Choi YS, Ahn YM. Clinical characteristics and prevalence of vitamin D insufficiency in children less than two years of age. Korean J Pediatr 2011;54:298–303.



13. Choi HS, Oh HJ, Choi H, Choi WH, Kim JG, Kim KM, et al. Vitamin D insufficiency in Korea: a greater threat to younger generation: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008. J Clin Endocrinol Metab 2011;96:643–651.


14. Park SY, Park SW, Kang SK, Jun YH, Kim SK, Son BK, et al. Subclinical rickets in breastfed infants. Korean J Pediatr 2007;50:1188–1193.

15. Bae SN, Rho EJ, Lim JW, Cheon EJ, Ko KO, Lee YH. A case of hypocalcemia due to vitamin D deficiency in exclusively breastfed infant. J Korean Soc Pediatr Endocrinol 2006;11:205–208.
16. Seo JY, Kim C, Lee HW, Ahn YM. Eight cases of incidentally diagnosed as subclinical rickets. Korean J Pediatr 2008;51:812–819.

17. Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr 2008;87:1080S–1086S.


18. Hatun S, Ozkan B, Bereket A. Vitamin D deficiency and prevention: Turkish experience. Acta Paediatr 2011;100:1195–1199.


19. Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc 2006;81:353–373.


20. Arya SC, Agarwal N. Seasonal variation & determinants in vitamin D deficiency in healthy breastfed term infants & their mothers in India. Indian J Med Res 2011;134:123


21. Balasubramanian S. Vitamin D deficiency in breastfed infants & the need for routine vitamin D supplementation. Indian J Med Res 2011;133:250–252.


22. Nickkho-Amiry M, Prentice A, Ledi F, Laskey MA, Das G, Berry JL, et al. Maternal vitamin D status and breast milk concentrations of calcium and phosphorus. Arch Dis Child 2008;93:179
23. Sullivan SS, Rosen CJ, Halteman WA, Chen TC, Holick MF. Adolescent girls in Maine are at risk for vitamin D insufficiency. J Am Diet Assoc 2005;105:971–974.


24. Pettifor JM. Rickets and vitamin D deficiency in children and adolescents. Endocrinol Metab Clin North Am 2005;34:537–553. vii


25. Ginde AA, Liu MC, Camargo CA Jr. Demographic differences and trends of vitamin D insufficiency in the US population, 1988-2004. Arch Intern Med 2009;169:626–632.



26. Saintonge S, Bang H, Gerber LM. Implications of a new definition of vitamin D deficiency in a multiracial US adolescent population: the National Health and Nutrition Examination Survey III. Pediatrics 2009;123:797–803.


27. Mutlu GY, Kusdal Y, Ozsu E, Cizmecioglu FM, Hatun S. Prevention of Vitamin D deficiency in infancy: daily 400 IU vitamin D is sufficient. Int J Pediatr Endocrinol 2011;2011:4



28. Zhu Z, Zhan J, Shao J, Chen W, Chen L, Li W, et al. High prevalence of vitamin D deficiency among children aged 1 month to 16 years in Hangzhou, China. BMC Public Health 2012;12:126



29. Wright A, Schanler R. The resurgence of breastfeeding at the end of the second millennium. J Nutr 2001;131:421S–425S.


31. McDowell MM, Wang CY, Kennedy-Stephenson J. Breastfeeding in the United States: findings from the national health and nutrition examination surveys, 1999-2006. NCHS Data Brief 2008;(5): 1–8.
32. Schubert L, DeLuca HF. Hypophosphatemia is responsible for skeletal muscle weakness of vitamin D deficiency. Arch Biochem Biophys 2010;500:157–161.


33. Turan S, Topcu B, Gokce I, Guran T, Atay Z, Omar A, et al. Serum alkaline phosphatase levels in healthy children and evaluation of alkaline phosphatase z-scores in different types of rickets. J Clin Res Pediatr Endocrinol 2011;3:7–11.



34. D'Amour P, Rousseau L, Hornyak S, Yang Z, Cantor T. Influence of secondary hyperparathyroidism induced by low dietary calcium, vitamin D deficiency, and renal failure on circulating rat PTH molecular forms. Int J Endocrinol 2011;2011:469783


35. Harinarayan CV, Ramalakshmi T, Prasad UV, Sudhakar D, Srinivasarao PV, Sarma KV, et al. High prevalence of low dietary calcium, high phytate consumption, and vitamin D deficiency in healthy south Indians. Am J Clin Nutr 2007;85:1062–1067.


36. Schiele F, Henny J, Hitz J, Petitclerc C, Gueguen R, Siest G. Total bone and liver alkaline phosphatases in plasma: biological variations and reference limits. Clin Chem 1983;29:634–641.


37. Thacher TD, Fischer PR, Pettifor JM. Rickets: vitamin D and calcium deficiency. J Bone Miner Res 2007;22:638


38. Saliba W, Barnett O, Rennert HS, Lavi I, Rennert G. The relationship between serum 25(OH)D and parathyroid hormone levels. Am J Med 2011;124:1165–1170.


39. Chung W, Kim H, Nam CM. Breast-feeding in South Korea: factors influencing its initiation and duration. Public Health Nutr 2008;11:225–229.


40. Kim JY, Hwang SJ, Park HK, Lee HB, Kim NS. Analysis of online breast-feeding consultation on the website of the Korean Pediatric Society. Korean J Pediatr 2008;51:1152–1157.

Fig. 1
The distribution of serum 25-hydroxyvitamin D (25[OH]D) with parathyroid hormone. The serum parathyroid hormone levels of two infants were abnormally increased to 124.8 and 86.6 pg/mL each, although no positive correlation (Pearson; P=0.051).
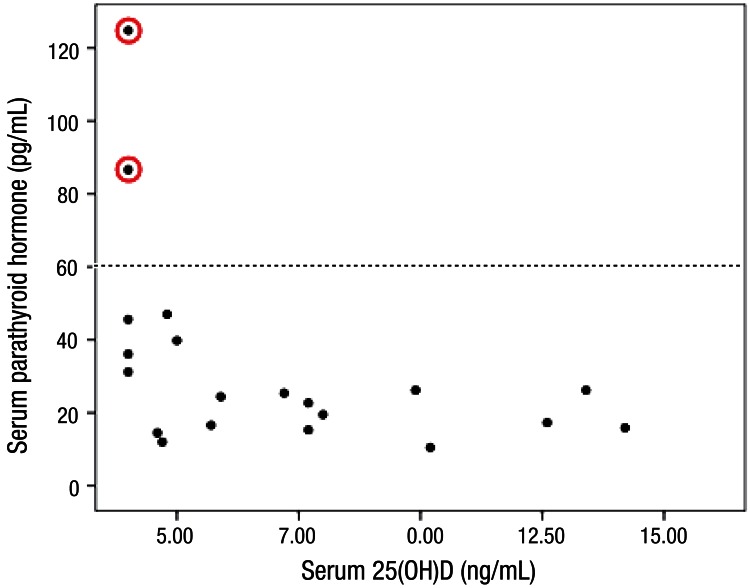
Table 2
Correlation between participants characteristics and Vitamin D deficiency
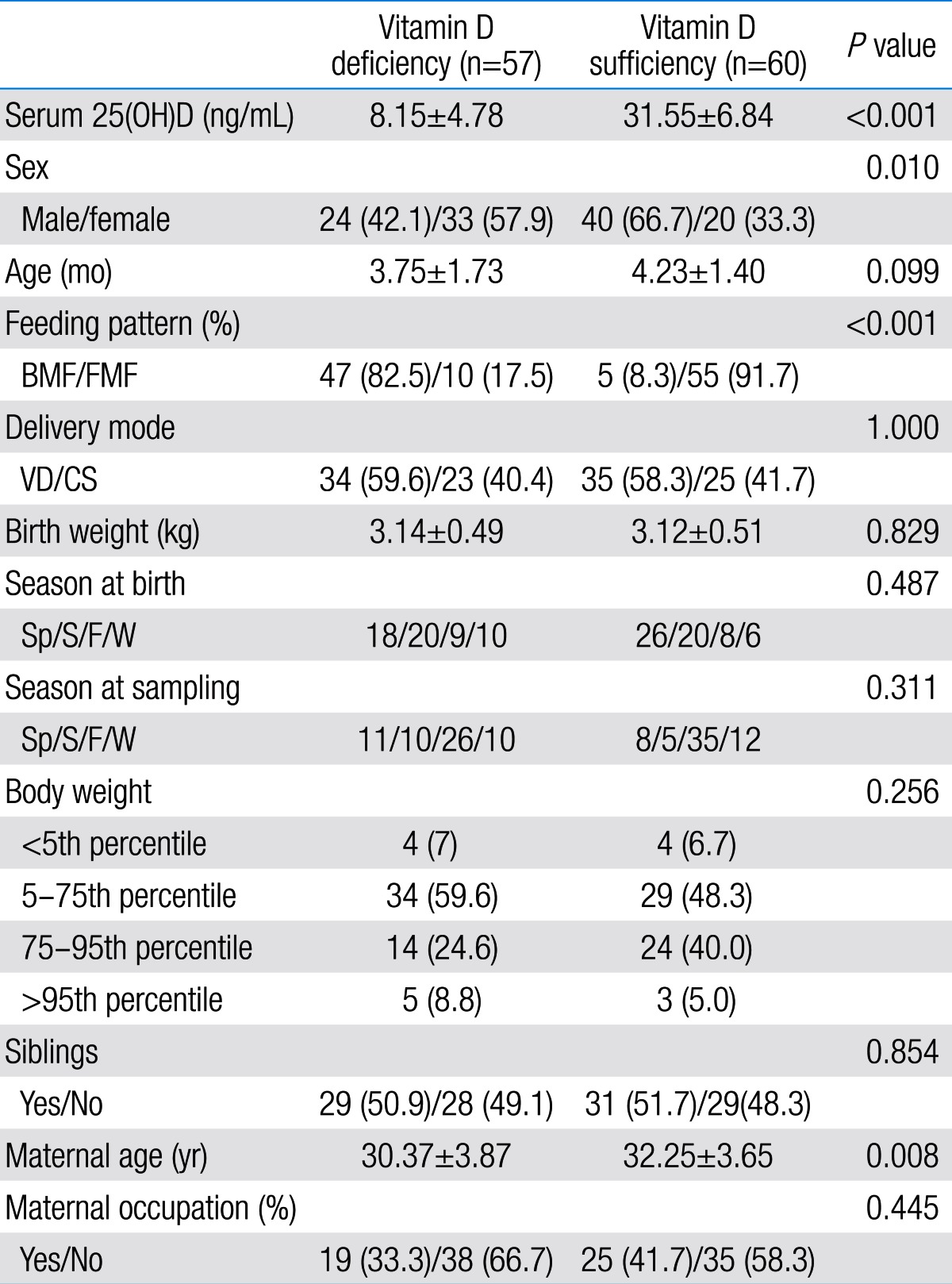
Values are presented as mean±standard deviation or number (%).
25(OH)D, 25-hydroxyvitamin D; BMF, breast milk feeding; FMF, formula milk feeding; VD, vaginal delivery; CS, cesarean section; Sp, spring; S, summer; F, fall; W, winter.
Percentile of body weight was adapted from 2007 Korean National Growth Charts42).




 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


