Article Contents
| Clin Exp Pediatr > Volume 69(1); 2026 |
|
A term male infant was delivered by emergency caesarean section for cord prolapse to a 31-year-old gravida 2, para 1 mother following an uncomplicated pregnancy. The antenatal mid-trimester ultrasound was unremarkable. At birth, a large anterior cervical mass measuring approximately 16 cm×11 cm was noted. It had not been detected antenatally during the second trimester and may have rapidly progressed in size during the third trimester (Fig. 1A). Due to the unexpected nature of the mass, only one team member was present for resuscitation in the delivery room. Bag-mask ventilation and continuous positive airway pressure were initiated, resulting in partial improvement in oxygenation. Two senior members of the resuscitation team were urgently called to assist and secure a stable airway. Despite good visualization of the glottis during direct laryngoscopy, the endotracheal tube could not be advanced beyond the vocal cords due to external compression.
An on-call otolaryngologist was urgently consulted and successfully intubated the infant using a video laryngoscope while manually lifting the mass. This maneuver effectively relieved the airway compression, allowing smooth passage of the endotracheal tube and safe transfer to the neonatal intensive care unit (NICU). The lesion was firm, multinodular, and did not transilluminate. The infant exhibited poor tone, weak spontaneous respiratory effort, and restricted neck flexion. Postnatal magnetic resonance imaging (MRI) revealed a well-demarcated midline submandibular lesion exerting significant mass effect on the trachea, without invasion of adjacent structures (Fig. 1B). Echocardiography was normal.
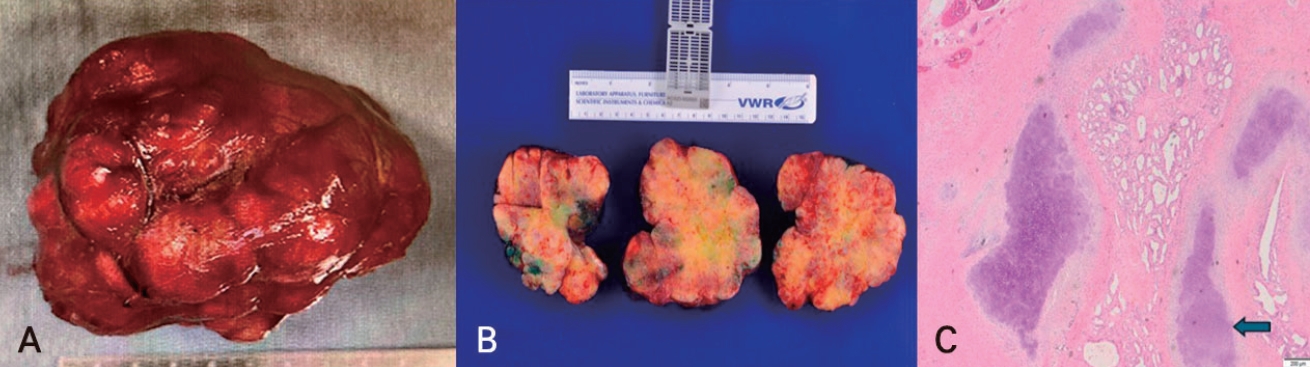
On day 8 of life, the mass was surgically excised en bloc. The specimen was received fresh in the laboratory and consisted of a single, firm, irregular, multinodular mass weighing 303 g and measuring 9.4 cm×9.2 cm×9.1 cm (Fig. 2A). A cross-section of a specimen and histopathology confirmed an immature teratoma (Fig. 2B and C), and comprehensive DNA panel testing for tumor markers was negative. The infant was extubated on postoperative day 2 but immediately developed intermittent stridor. Bronchoscopy revealed subglottic granulation tissue, attributed to pressure necrosis from prolonged external tracheal compression and contact with the endotracheal tube. Topical ciprofloxacin-dexamethasone was administered, resulting in complete resolution within 1 week. The infant was discharged home on day 21, feeding normally and thriving.
Written parental consent was obtained to publish this case. According to the Conjoint Health Research Ethics Board at the University of Calgary, case reports describing unique clinical scenarios do not meet the definition of research under the Tri-Council Policy Statement and therefore do not require ethics board approval.
Neonates are vulnerable to external airway compression, especially from cervical masses, which can prevent advancement of the endotracheal tube [1,2]. In this case, the mass was undetected antenatally, and the resuscitation team was not fully prepared for the airway emergency. Intubation was ultimately successful after the otolaryngologist manually elevated the mass, relieving the compression on the pliable neonatal airway and restoring patency.
This simple yet effective maneuver highlights the importance of mechanical strategies in airway management. Similar techniques are described in ex-utero intrapartum treatment (EXIT) procedures and postnatal emergencies, where relieving pressure can be as critical as the intubation technique itself [3-5].
Sustained extrinsic compression may compromise the vascular supply to the tracheal mucosa and cartilage, leading to ischemic injury, inflammation, and granulation tissue formation. In this case, bronchoscopy confirmed subglottic granulation tissue, likely caused by the trachea being compressed between the mass and the endotracheal tube. Similar sequelae have been reported in neonates and older children, where extrinsic narrowing predicted perioperative complications [6,7].
Prenatal imaging has significantly improved the management of such cases. Advances in ultrasound and fetal MRI allow for early detection of cervical masses, often with evidence of tracheal deviation or compression. These findings enable neonatologists to anticipate airway difficulties and prepare for EXIT procedures, which provide controlled conditions for intubation [8].
However, when antenatal detection is lacking, safe outcomes depend on rapid recognition of neck masses in the delivery room, prompt airway maneuvers such as mass elevation, and the availability of expert resuscitation teams. The presence of a video laryngoscope and an otolaryn gologist at delivery or in the operating room can be critical.
The differential diagnosis for midline neck masses includes malignant teratoma, neuroblastoma, rhabdomyosarcoma, and lymphomas. In this case, lymphomas were excluded due to the absence of cervical lymphadenopathy or splenomegaly, and congenital goiter was ruled out based on imaging. Soft tissue tumors remained a possibility, and pathological examination confirmed the mass as an immature teratoma. The negative tumor marker panel ruled out Tier 1 and Tier 2 variants.
The main learning point from this case is the importance of being prepared for difficult airway management in neonates with undiagnosed cervical masses. External compression can pose a significant challenge during intubation, and simple maneuvers such as lifting the mass can be lifesaving. Early recognition and intervention are essential to stabilize the neonate before transfer to the NICU for further evaluation and management.
Following surgical excision, long-term outcomes are excellent if tracheal injury is identified and treated early. An otolaryngologist should be involved prenatally when such conditions are known, as this is the cornerstone of safe outcomes and effective airway management.
Footnotes
Conflicts of interest
No potential conflict of interest relevant to this article was reported. Funding: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Fig. 1.
(A) Shows a midline neck mass (measuring 16 cm×11 cm) obstructing the airway and causing respiratory distress in a newborn. (B) The magnetic resonance imaging shows a large, fairly well-defined, heterogeneous solid soft tissue mass centered in the midline submandibular region. There is a local regional mass effect, with no intrinsic calcification observed.
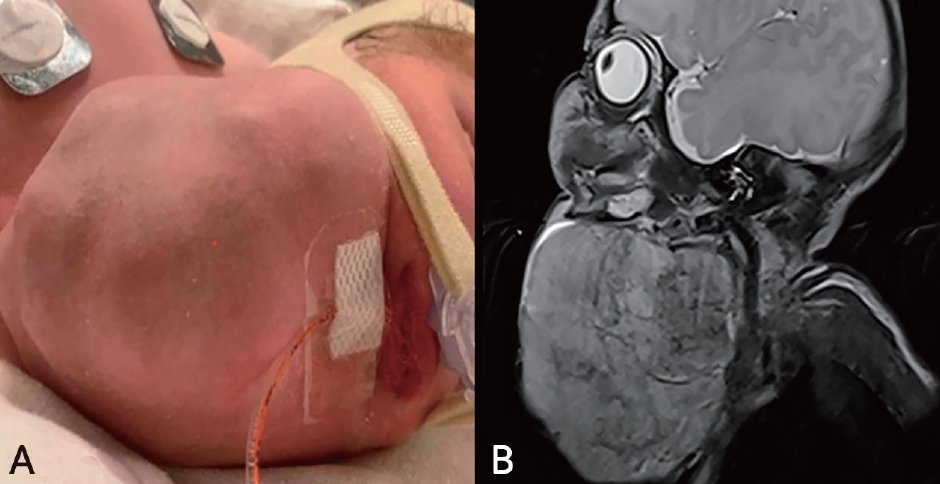
Fig. 2.
(A) Shows a midline neck mass (measuring 16 cm×11 cm) obstructing the airway and causing respiratory distress in a newborn. (B) The magnetic resonance imaging shows a large, fairly well-defined, heterogeneous solid soft tissue mass centered in the midline submandibular region. (C) Pathology slide showing components of immature teratoma and myxoid mesenchymal tissue, with innumerable foci of immature and mature cartilage (black arrow), and interspersed foci of immature fat. Glandular and tubuloglandular foci are also noted (H&E, ×2).
References
1. Mikovic Z, Simic R, Egic A, Opincal TS, Koprivsek K, Stanojevic D, et al. Intrauterine treatment of large fetal neck lymphangioma with OK-432. Fetal Diagn Ther 2009;26:102-6.



2. Zeng Z, Liao H, Hu F, Zhao F, Liu H, Hu Q, et al. Outcome of sclerotherapy in a preterm infant with a giant fetal neck lymphatic malformation: a case report. Int J Womens Health 2023;15:1771-8.




3. Cruz-Martinez R, Moreno-Alvarez O, Garcia M, Méndez A, Pineda H, Cruz-Martinez MA, et al. Fetal endoscopic tracheal intubation: a new fetoscopic procedure to ensure extrauterine tracheal permeability in a case with congenital cervical teratoma. Fetal Diagn Ther 2015;38:154-8.



4. Özcan R, Karagöz A, Hakalmaz AE, Adaletli İ, Madazlı R, Altındaş G. Approach to prenatal diagnosed giant cervical mass with extrauterine intrapartum treatment (EXIT) method. Turkish J Ped Surg 2022;36:50-4.
5. Steigman C, Copel J, Zamudio S, Weiner H, Campbell W. Prenatal diagnosis of cervical teratoma: Clinical predictors of outcome. Fetal Diagn Ther 2009;25:181-5.
6. Anghelescu DL, Burgoyne LL, Liu T, Li CS, Pui CH, Hudson MM, et al. Clinical and diagnostic imaging findings predict anesthetic complications in children presenting with malignant mediastinal masses. Paediatr Anaesth 2007;17:1090-8.








 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


