Article Contents
| Clin Exp Pediatr > Volume 69(2); 2026 |
|
Abstract
Background
Purpose
Methods
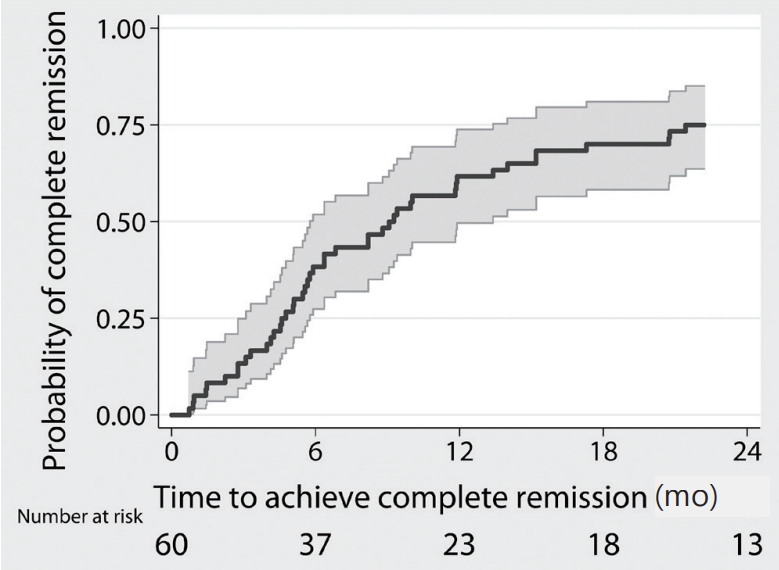
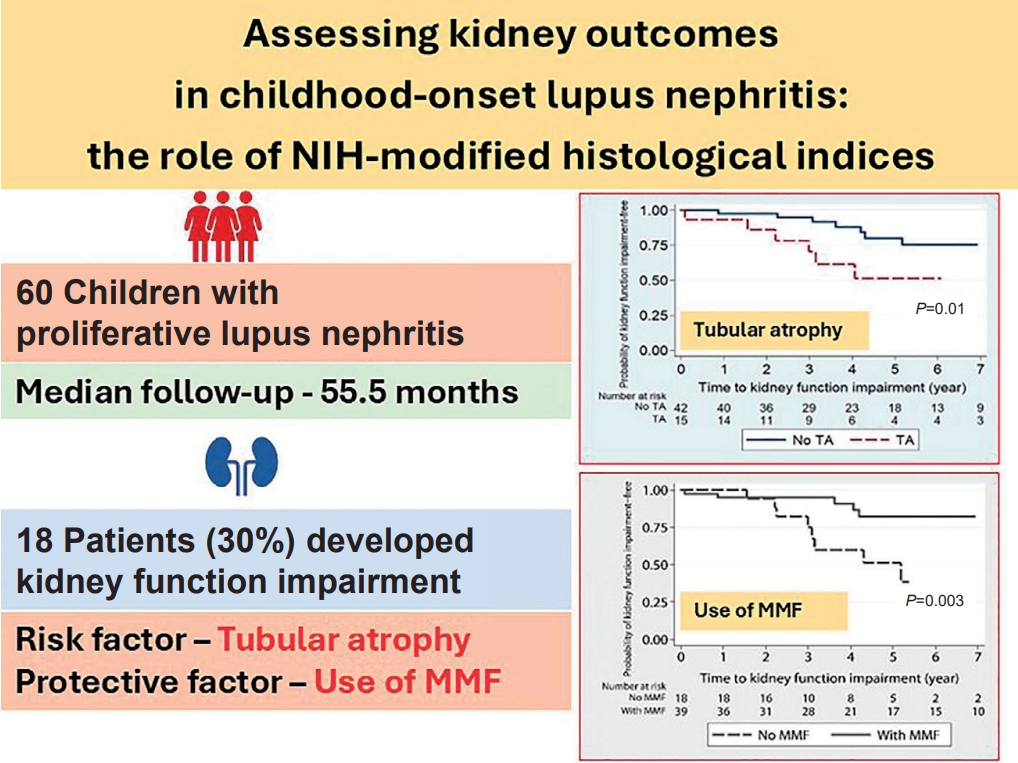
Results
Conclusion
Supplementary materials
Supplementary Table 1.
Footnotes
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Acknowledgments
We would like to thank the English Editing Service, Research Affairs, Faculty of Medicine, Chulalongkorn University, for their editorial support. We also extend our sincere thanks to Dr. Kroonpong Iampenkhae, MD, and Dr. Jerasit Surintrspanont, MD, for their valuable assistance in the interpretation of kidney biopsy specimens.
Fig. 1.
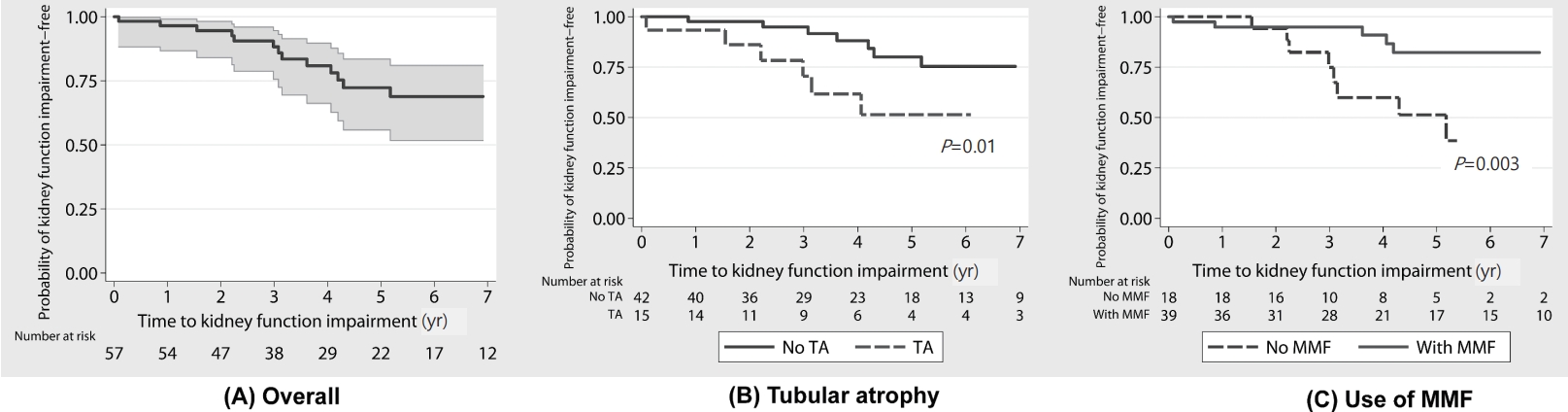
Table 1.
Values are presented as number (%) or median (interquartile range).
KFI, kidney function impairment; LN, lupus nephritis; C3, complement C3; C4, complement C4; SLEDAI, Systemic Lupus Erythematosus Disease Activity Index 2000; dsDNA, double-stranded DNA; eGFR, estimated glomerular filtration rate; AKI, acute kidney injury; UPCR, urine protein-to-creatinine ratio.
Boldface indicates a statistically significant difference with P<0.05.
Table 2.
| Findings | Total (N=60) | KFI (N=18, 30%) | No-KFI (N =42, 70%) | P value |
|---|---|---|---|---|
| No. of glomeruli | 28 (18–36) | 28 (22–30) | 28 (18–42) | 0.67 |
| Histologic class | 0.16 | |||
| III | 19 (31.7) | 8 (44.4) | 11 (26.2) | |
| IV | 28 (46.7) | 9 (50.0) | 19 (45.2) | |
| Mixed (III+V/IV+V) | 13 (21.7) | 1 (5.6) | 12 (28.6) | |
| Activity index | 3 (2–7) | 3.5 (1–10) | 3 (2–7) | 0.97 |
| Endocapillary hypercellularitya) | 51 (85.0) | 14 (77.8) | 37 (88.1) | 0.43 |
| Neutrophil infiltrationa) | 26 (43.3) | 6 (33.3) | 20 (47.6) | 0.31 |
| Hyaline depositsa) | 16 (26.7) | 6 (33.3) | 10 (23.8) | 0.45 |
| Cellular/fibrocellular crescentsa) | 30 (50.0) | 9 (50.0) | 21 (50.0) | 1.00 |
| Fibrinoid necrosisa) | 6 (10.0) | 2 (11.1) | 4 (9.5) | 1.00 |
| Interstitial inflammationa) | 25 (41.7) | 10 (55.6) | 15 (35.7) | 0.17 |
| Chronicity index | 1 (0–2.5) | 3 (1–4) | 1 (0–1) | <0.001 |
| Glomerulosclerosisa) | 32 (53.3) | 13 (72.2) | 19 (45.2) | 0.09 |
| Fibrous crescentsa) | 11 (18.3) | 5 (27.8) | 6 (14.3) | 0.28 |
| Tubular atrophya) | 18 (30.0) | 11 (61.1) | 7 (16.7) | 0.001 |
| Mild | 16 | 9 | 7 | |
| Moderate | 1 | 1 | 0 | |
| Severe | 1 | 1 | 0 | |
| Interstitial fibrosisa) | 13 (21.7) | 9 (50.0) | 4 (9.5) | 0.001 |
| Mild | 11 | 7 | 4 | |
| Moderate | 1 | 1 | 0 | |
| Severe | 1 | 1 | 0 |





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


