Article Contents
| Clin Exp Pediatr > Volume 66(7); 2023 |
|
Abstract
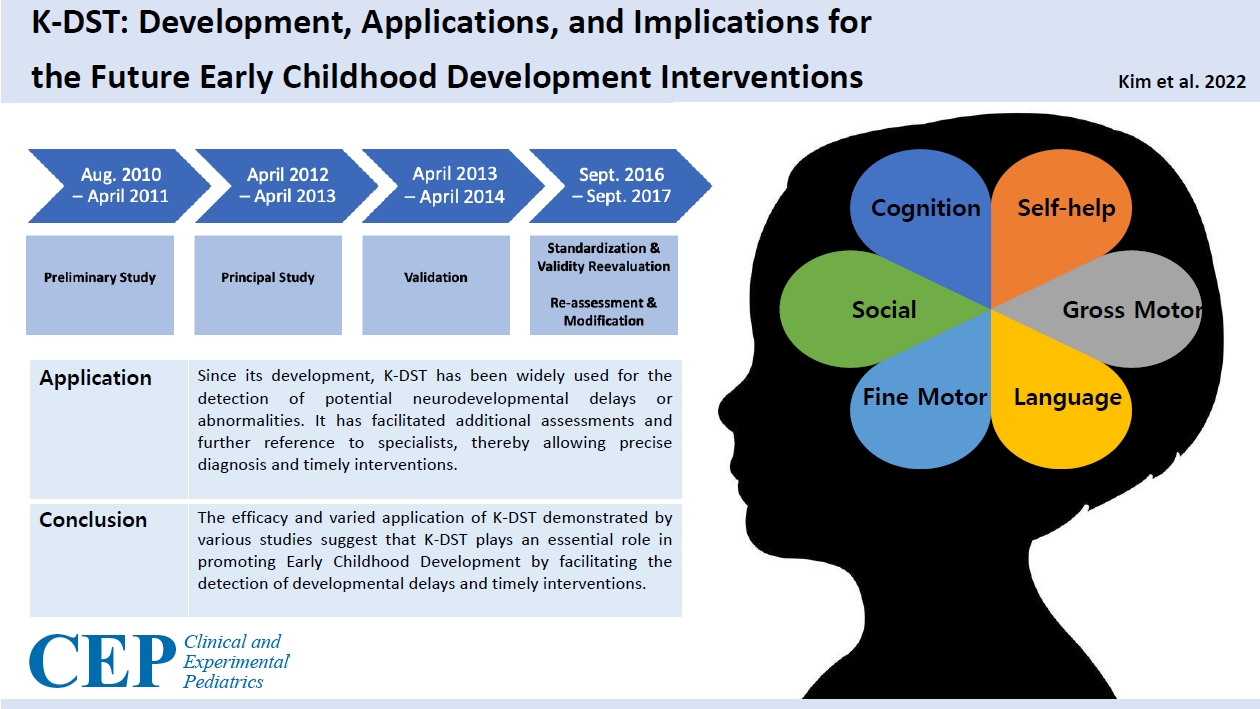
Evidence of the importance of early childhood development (ECD) has transformed child health monitoring and screening tools. Development of the Korean Developmental Screening Test for Infants and Children (K-DST) has expanded the applications of child health screening to a large number of infants and children in Korea and is contributing to the early detection of neurodevelopmental disorders and delivery of timely interventions. The previous screening tool (Korean Ages and Stages Questionnaire) raised some concerns, as its lack of consideration of the cultural background of the Korean population can lead to inaccurate or imprecise diagnoses. The K-DST, a tailored tool for Korean infants and children, is a simple and cost-efficient solution for child health monitoring and screening. This review focuses on the development and role of the K-DST in ensuring ECD. Here we review use of the K-DST for ECD screenings and discuss the best strategy for its use in other countries.
Graphical abstract. K-DST, Korean Developmental Screening Test for Infants and Children.
Early childhood development (ECD) consists of cognitive, socioemotional, and motor development that occurs between 0 and 8 years of age [1]. These early years, especially up to 3 years of age, are critical as the brain develops at a remarkable speed that is never repeated later in life [2]. ECD serves as the foundation for sustainable development as it has a direct effect on the overall development of children and the adults they will become [3]. Thus, ensuring that every child develops to the maximum extent possible and achieves their full developmental potential through multidisciplinary investments in ECD has been prioritized by governments and United Nations agencies including the United Nations Children’s Fund (UNICEF) and the World Health Organization [4,5].
Developmental screening is a crucial component of ensuring ECD, as it allows the early identification of any abnormal neurodevelopmental process. The effectiveness of interventions increases when they are initiated early [6,7]. Caregivers and pediatricians are able to examine how a child is developing, including their language, motor skills, cognition, socioemotional, and behavior, using a brief, well-structured screening test. Developmental screenings are powerful tools, especially when applied for children who are at higher risk of neurodevelopmental problems due to preterm birth, malnutrition, low birth weight, or environmental risks such as lead exposure, all of which are more prevalent in low-income countries [8]. As such, developmental screenings for infants and children can serve as important tools to enhance ECD as they enable the prompt identification of any abnormalities and the administration of early intervention treatment services including special education [9].
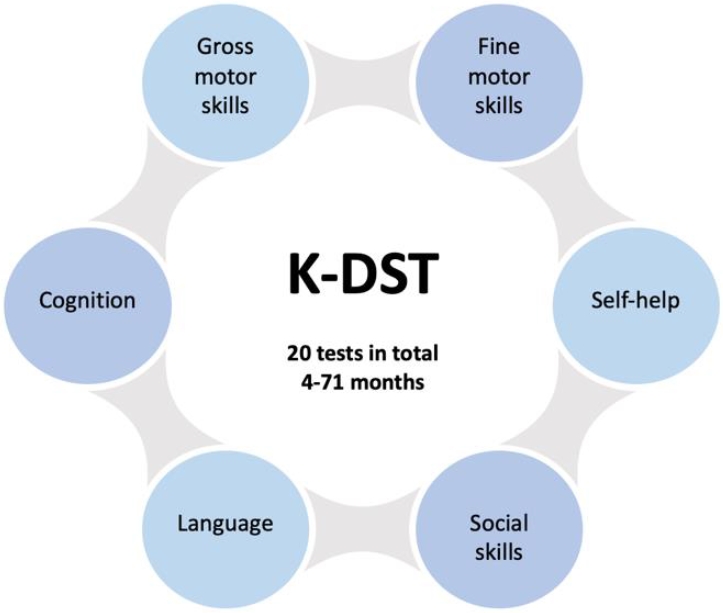
The first edition of the Korean Developmental Screening Test (K-DST) was sponsored by the Ministry of Health and Welfare and the Korean Centers for Disease Control and Prevention in 2014. Since then, the K-DST has been administered to approximately 1.8 million infants and children each year to examine ECD in the gross motor, fine motor, cognition, language, social skills, and self-help domains by the National Health Screening Program for Infants and Children (NHSPIC) (Fig. 1). Since then, test restandardization and revalidation were conducted in 2017 using 3.06 million infants and children who were checked as part of the NHSPIC in 2015–2016. The revised K-DST was subsequently published.
This article primarily aims to provide insight into the development of the K-DST and its incorporation into Korea’s national healthcare system. It also notes its further applicability for strengthening screening and monitoring programs in developing countries to better foster ECD through horizontal cooperation and knowledge sharing.
The K-DST was developed through the NHSPIC, which was introduced in Korea in 2007 [10]. The NHSPIC plays a significant role as it is the key infrastructure that supports the normal growth of infants and children through tracking and managing their growth and development, detecting abnormalities, and educating their parents or caregivers. When the NHSPIC was initiated in 2007, the Korean Ages and Stages Questionnaire (K-ASQ), a Korean version of the Ages and Stages Questionnaire developed in the United States, or the Denver Development Screening test was used instead. It is a relatively reliable tool, as it has been standardized to Korean and modified accordingly, but it had several limitations (Supplementary Table 1). First, the K-ASQ had to be purchased by each screening institution, and its use was limited because of copyright issues. Furthermore, as the K-ASQ did not incorporate cultural differences between Korea and the United States, it was not optimal for the screening the growth and development of Korean children [10]. Finally, only children younger than 60 months of age could be screened through the K-ASQ, while the NHSPIC can be used for children up to 71 months of age. Considering these limitations, the Korean government developed the K-DST tailored to Korean infants and children by following 5 steps as described below (Fig. 2).
First, a preliminary study was conducted to examine the tasks regarding the screening of Korean infants and children and the currently available developmental tests and screening tools through a series of literature reviews. The adequacy of the K-ASQ was also evaluated. Second, based on the results, a roadmap for the development of the K-DST was proposed. In the principal study, preliminary questions that test growth and development in 6 domains (gross motor, fine motor, cognition, language, social skills, and self-help) were selected and standardized through surveys and analysis of questions (level of difficulty discrimination) and reliability (consistency, test-retest reliability). Third, the K-DST was validated through an analysis of its validity, sensitivity, specificity, receiver operating characteristic curve, and criterion-related validity. Fourth, test restandardization and revalidation were conducted based on the data collected from 3.06 million infants and children who were checked as part of the NHSPIC in 2015–2016. And finally, after modifications and revision, the revised K-DST was finalized in 2017.
The NHSPIC, which is conducted 8 times, includes physical measurements and examinations, developmental evaluations, health education for caregivers, and oral examinations. Developmental screenings using the K-DST are conducted 6 times for infants and children aged 4–71 months. The K-DST can be completed both online through the website and offline through the printed questionnaire, thereby ensuring easy application regardless of technical factors related to the screening institutions or caregivers. For each of the 6 domains, a set of 8 questions was asked, and the total score was calculated based on the answers: 3 points – Can do well; 2 points – Can do; 1 point – Cannot do well; and 0 point – Absolutely cannot do. The total score was evaluated based on the transfer points of each domain. The KDST results are broadly grouped into 5 categories: (1) good, (2) requires follow-up examination, (3) requires detailed assessment, (4) continued care, and (5) other. This allows for timely referral to developmental specialists in cases in which growth or developmental abnormalities are detected.
As the K-DST was developed, standardized, and validated based on data from Korean infants and children, it serves as an ideal developmental screening tool that incorporates the developmental characteristics and cultural traits of this population [10]. It also fosters a simple and wide application for general practitioners for monitoring, screening, and evaluation of the developmental status of Korean infants and children. This allows us to obtain baseline data on the growth and development of infants and children that can be used for further research and adaptation of the screening system [11,12]. With its own right as the national intellectual property developed independently by the Korean government, it can be easily distributed and adapted as necessary.
Several studies have demonstrated the efficacy and accuracy of the K-DST for detecting neurodevelopmental delays and disabilities (Table 1) [13]. By indicating potential neurodevelopmental delays or abnormalities in one or more categories, the K-DST has facilitated further examinations of infants and children through novel technologies such as chromosomal microarray [14], next-generation sequencing [15,16], and the Infant Comprehensive Evaluation for Neurodevelopmental Delay [17]. The K-DST has also facilitated the administration of additional and complementary assessment tools such as the Parental Questionnaire for Cerebral Visual Impairment [18] and the Korean version of the Developmental Snapshot [19]. Several studies have also indicated and validated that the K-DST allows further reference and evaluation of children with speech sound disorder and language impairment [20,21], motor development [22], and cerebral visual impairment [18]. The application of the K-DST is correlated with increased reporting of neurodevelopmental conditions such as autism spectrum disorder [23], ADHD [13], and sleep disorder [24], pointing to the importance of screening tools in detecting neurodevelopmental delays and disabilities.
An infant's birth weight is a crucial measurement factor associated with mortality and neurodevelopment. Very low birth weight (VLBW) infants are at an increased risk of neurodevelopmental delays and disabilities, including long-term neurodevelopmental outcomes [25,26]. Therefore, the importance of effective developmental screening is even more pronounced in VLBW infants. The K-DST is effective for assessing the neurodevelopment of cognitive and language domains in VLBW infants [27,28]. Studies have demonstrated that the K-DST allows the accurate assessment of language and motor developmental delay [29] and has further neurodevelopmental implications among VLBW infants [30]. VLBW infants are also at higher risk for pathologies that may have neurodevelopmental implications [31]. The K-DST has facilitated the examination of pathologies such as retinopathy [32,33], respiratory diseases [34,35], brain injuries (cystic periventricular leukomalacia [36], hypoxic-ischemic encephalopathy [37]; and thyroid dysfunction [38], all of which can affect the neurodevelopment of VLBW infants.
The K-DST is an effective and valid screening tool. The studies presented here underscore the importance of screening and monitoring to ensure ECD. Although several developmental screening tools are currently available, such as the Ages and Stages Questionnaire, Parents' Evaluation of Developmental Status, and Child Development Inventories, a large number of countries, particularly low- and low- to middle-income countries (LMICs), do not have the resources to develop or conduct screenings based on context-specific measures [39] despite evidence of the benefits of ECD screening. This is particularly concerning, as LMICs are associated with an increased incidence of VLBW infants who are at higher risk of neurodevelopmental delay.
The prolonged coronavirus disease 2019 pandemic has been associated with negative implications on child growth and development [40]. Social restrictions, lockdowns, school closures, increased media use, and reduced access to healthcare services can be risk factors that threaten ECD, thereby highlighting the increased need for cost-effective growth and development screenings. Studies have also indicated that elevated levels of maternal anxiety negatively influence ECD [41].
The key value of the K-DST is that it screens and monitors a comprehensive range of ECD while maintaining simplicity, allowing caregivers and health professionals to easily administer it and understand its results. The development process of the K-DST based on existing screening tools (ASQ and K-ASQ) and its tailoring to Korean infants and children points to the promising possibility that other countries may translate and adapt the K-DST to their local populations. The K-DST may require adjustment; however, especially for low-capacity countries, certain questionnaire sets of the K-DST can be grouped so it may be administered less frequently. This may facilitate its implementation in countries lacking primary healthcare professionals, including pediatricians.
In this context, the UNICEF Seoul Liaison Office hosted a global dialogue in a hybrid format on December 14, 2020. More than 120 UNICEF experts from various backgrounds ranging from education to neurology attended and discussed ways to transfer Korea’s experience developing and implementing the K-DST at the national level. The participants also shared common challenges implementing a developmental screening tool that is associated with the limited resources of both caregivers and healthcare professionals. These challenges underline the strengths of the K-DST and its potential for use outside of Korea. Several potential strategies to transfer the K-DST to other countries were proposed during the dialogue, including bilateral or multilateral capacity-building programs in which Korean pediatricians train pediatricians in countries that need technical assistance. Another strategy is to launch a series of knowledge-sharing workshops that can serve as a channel for pediatricians across countries to connect and discuss ways to adopt and implement the K-DST.
Going forward, the K-DST will continue to support ECD and may serve as the best practice for developing a tailored and resource-efficient screening tool.
Supplementary material
Supplementary Table 1 can be found via https://doi.org/10.3345/cep.2022.00906.
Footnotes
Conflict of interests
The opinions expressed in this study are those of the authors. They do not reflect the opinions or views of the FATF, OECD, or other member countries. No potential conflict of interest relevant to this article was reported.
Acknowledgments
The authors would like to thank Dr. Pia Rebello Britto (UNICEF Representative of the Lao People’s Democratic Republic) and Ana Nieto (Early Childhood Development Specialist, UNICEF Headquarters) for their excellent support and guidance.
Fig. 2.
Overview of the Korean Developmental Screening Test for Infants and Children (K-DST) development process (revised version). K-ASQ, Korean Ages and Stages Questionnaire.
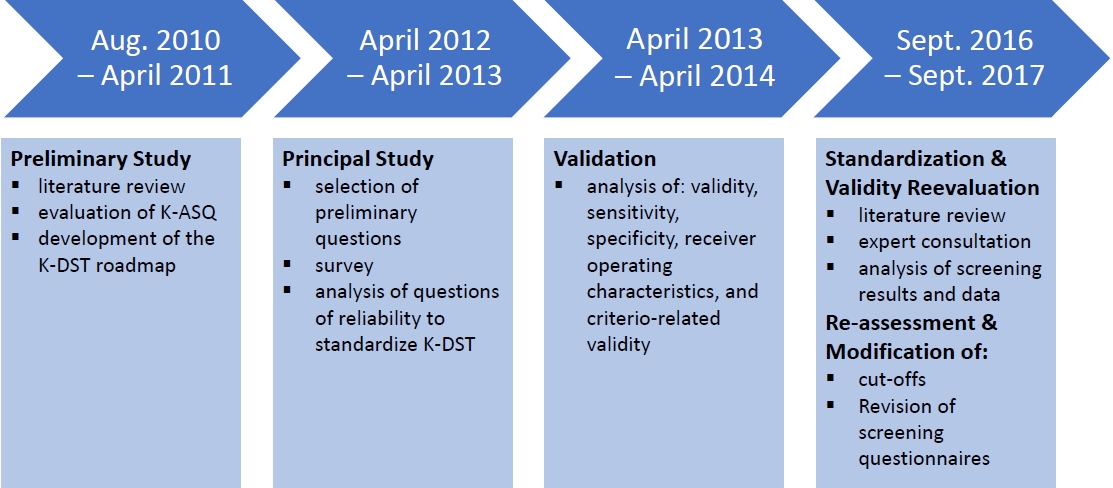
Table 1.
Application areas of Korean Developmental Screening Test for Infants and Children (K-DST) in detecting developmental delays and abnormalities and assessing the impact of pathologies on development of very low birth weight infants
References
1. United Nations International Children's Emergency Fund (UNICEF). UNICEF Programme guidance for early childhood development [Internet]. New York: UNICEF; c2017 [cited 2021 Sep 21]. Available from: https://www.unicef.org/documents/unicef-programme-guidance-early-childhood-development.
2. Tierney AL, Nelson CA 3rd. Brain development and the role of experience in the early years. Zero Three 2009;30:9–13.


3. Leckman J, Britto P. Steps toward peace and violence prevention across generations: the potential early child development in the context of the 2030 sustainable development goals. New Direct Child Adolesc Devel 2018;159:5–12.
4. United Nations International Children's Emergency Fund (UNICEF). Global Annual Results Report 2021: every child survives and thrives [Internet]. New York: UNICEF; c2022 [cited August 2021 Aug 25]. Available from: https://www.unicef.org/reports/global-annual-results2021-goal-area-1.
5. World Health Organization. Improving early childhood development. WHO guideline [Internet]. Geneva (Switzerland): World Health Organization; c2020 [cited 2021 Sep 25]. Available from: https://www.who.int/publications/i/item/97892400020986.
6. Wu YT, Tsou KI, Hsu CH, Fang LJ, Yao G, Jeng SF. Taiwan Infant Developmental Collaborative Study Group. Brief report: Taiwanese infants' mental and motor development--6-24 months. J Pediatr Psychol 2008;33:102–8.

7. Rispoli K, Norman M, Nelson S. Implementation of developmental screening in early childhood education: an investigation of process variables and acceptability. Top Early Child Spec Educ 2021;02711214211057010. https://doi.org/10.1177/02711214211057010.

8. Gil JD, Ewerling F, Ferreira LZ, Barros AJ. Early childhood suspected developmental delay in 63 low- and middle-income countries: large within- and between-country inequalities documented using national health surveys. J Global Health 2020;10:010427.



9. Vitrikas K, Savard D, Bucaj M. Developmental delay: when and how to screen. Am Fam Physician 2017;96:36–43.

10. Chung HJ, Yang D, Kim GH, Kim SK, Kim SW, Kim YK, et al. Development of the Korean Developmental Screening Test for Infants and Children (K-DST). Clin Exp Pediatr 2020;63:438–46.




11. Eun BL, Suh CR, Sohn SY, Kim GH, Jung SK. Single-center experience of the Korean-Developmental Screening Test for infants and children. Korean J Pediatr 2016;59:483–9.




12. Yim CH, Kim GH, Eun BL. Usefulness of the Korean Developmental Screening Test for infants and children for the evaluation of developmental delay in Korean infants and children: a single-center study. Korean J Pediatr 2017;60:312–9.




13. Kim S. Worldwide national intervention of developmental screening programs in infant and early childhood. Clin Exp Pediatr 2022;65:10–20.




14. Yang EH, Shin YB, Choi SH, Yoo HW, Kim HY, Kwak MJ, et al. Chromosomal microarray in children with developmental delay: the experience of a tertiary center in Korea. Front Pediatr 2021;15:9:690493.



15. Lee Z, Lee BJ, Park S, Park D. Relationship between clinical parameters and chromosomal microarray data in infants with developmental delay. Healthcare (Basel) 2020;27:8:305.



16. Lee J, Lee C, Ki CS, Lee J. Determining the best candidates for next-generation sequencing-based gene panel for evaluation of early-onset epilepsy. Mol Genet Genomic Med 2020;8:e1376.




17. Hong M, Lee KS, Park JA, Kang JY, Shin YW, Cho YI, et al. Preliminary report of validity for the Infant Comprehensive Evaluation for Neurodevelopmental Delay, a newly developed inventory for children aged 12 to 71 months. Soa Chongsonyon Chongsin Uihak 2022;33:16–23.



18. Moon JH, Kim GH, Kim SK, Kim S, Kim YH, Kim J, et al. Development of the Parental Questionnaire for Cerebral Visual Impairment in children younger than 72 months. J Clin Neurol 2021;17:354–62.




19. Pae SY, Yoon HJ, Seol AY, Gilkerson J. The validity and reliability of the Korean version of the developmental snapshot. Commun Sci Disord 2015;20:355–63.

20. Han MJ, Kim SJ. Characteristics of functional speech sound disorders in Korean children. Ann Child Neurol 2022;30:8–16.


21. Jang CH, Kim SW, Jeon HR, Jung DW, Cho HE, Kim J, et al. Clinical usefulness of the Korean Developmental Screening Test (K-DST) for developmental delays. Ann Rehabil Med 2019;43:490–6.




22. Hwang YJ, Lee EK. Validation of K-DST about motor and language development in children with developmental disabilities. J Speech Lang Hear Disord 2020;29:111–5.

23. Sunwoo HJ, Noh DH, Kim KM, Kim JH, Yoo HJ. A study on practitioner’s perceptions on early screening of autism spectrum disorder. J Korean Acad Child Adolesc Psychiatry 2017;28:96–105.

24. Tchah N, Yang DH, Kim HD, Lee JS, Kim SH, Kang HC. Clinical spectrum and treatment outcomes of patients with development and/or epileptic encephalopathy with spike-and-wave activation in sleep. Ann Child Neurol 2022;30:189–96.


25. Yoon SJ, Lim JH, Han JH, Shin JE, Lee SM, Eun HS, et al. Identification of growth patterns in low birth weight infants from birth to 5 years of age: nationwide Korean cohort study. Int J Environ Res Pub Health 2021;18:1206.



26. Scharf R, Stroustrup A, Conaway M, DeBoer M. Growth and development in children born very low birthweight. Arch Dis Child Neonatal Ed 2016;101:433–8.



27. Barros F, Barros A, Villar J, Matijasevich A, Domingues M, Victora C. How many low birthweight babies in low- and middle-income countries are preterm? Rev Saúde Pública 2011;45:607–16.

28. Kim CY, Jung E, Lee BS, Kim KS, Kim EA. Validity of the Korean Developmental Screening Test for very-low-birth-weight infants. Korean J Pediatr 2019;62:187–92.




29. Youn Y, Lee SM, Hwang JH, Cho SJ, Kim EK, Kim EA. Korean Neonatal Network. National registry data from Korean Neonatal Network: two-year outcomes of Korean very low birth weight infants born in 2013- 2014. J Korean Med Sci 2018;33:e309.


30. Han S, Kim OH, Yoo CR, Heo JS, Lee HS, Jeon JH. Neurodevelopmental correlations between the Korean Developmental Screening Test and Bayley Scale III in very-low-birth-weight infants. Neonat Med 2020;27:167–73.


31. Anil C, Basel PL, Singh S. Low birth weight and its associated risk factors: health facility-based case-control study. PLoS ONE 2020;15:e0234907.



32. Ahn JH, Lee KM, Kim MJ. Neurodevelopmental outcomes in very low birthweight infants with retinopathy of prematurity in a nationwide cohort study. Sci Rep 2022;12:5053.




33. Han G, Lim DH, Kang DB, Cho JH, Guallar E, Chang YS, et al. Association between retinopathy of prematurity in very-low-birth-weight infants and neurodevelopmental impairment. Am J Ophthalmol 2022;244:205–15.


34. Jeon GW, Oh MK, Chang YS. Definitions of bronchopulmonary dysplasia and long-term outcomes of extremely preterm infants in Korean Neonatal Network. Sci Rep 2021;11:24349.




35. Han YS, Kim SH, Sung TJ. Impact of the definition of bronchopulmonary dysplasia on neurodevelopmental outcomes. Sci Rep 2021;11:22589.




36. Cha JH, Choi NY, Kim JY, Lee HJ, Na JY, Park HK. Cystic periventricular leukomalacia worsens developmental outcomes of very-low-birth-weight infants with intraventricular hemorrhage – a nationwide cohort study. J Clin Med 2022;11:5886.



37. Hong KT, Shin SH, Choi YH, Kim EK, Kim HS. Case series of isolated deep gray matter injuries in preterm infants. Neonatal Med 2022;29:117–22.


38. Cho JY, Park JH, Yeom JS, Jun SJ, Park JS, Park ES, et al. Thyroid dysfunction and the effect of iodine-deficient parenteral nutrition in very low birth weight infants; a nationwide analysis of a Korean Neonatal Network database. Nutrients 2022;14:3043.



39. Naveed A. Addressing measurement challenges in early childhood development research in low- and middle-income countries London: The British Academy; 2020 Avaiable from: https://www.thebritishacademy.ac.uk/documents/2537/Addressing-measurement-challenges-earlychildhood-development-low-middle-incom_Ui4BHx7.pdf.
40. Araújo LA, Veloso CF, Souza MC, Azevedo JMC, Tarro G. The potential impact of the COVID-19 pandemic on child growth and development: a systematic review. J Pediatr (Rio J) 2021;7:369–77.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


