Article Contents
| Clin Exp Pediatr > Volume 64(9); 2021 |
|
Abstract
Acknowledgments
Fig. 1.
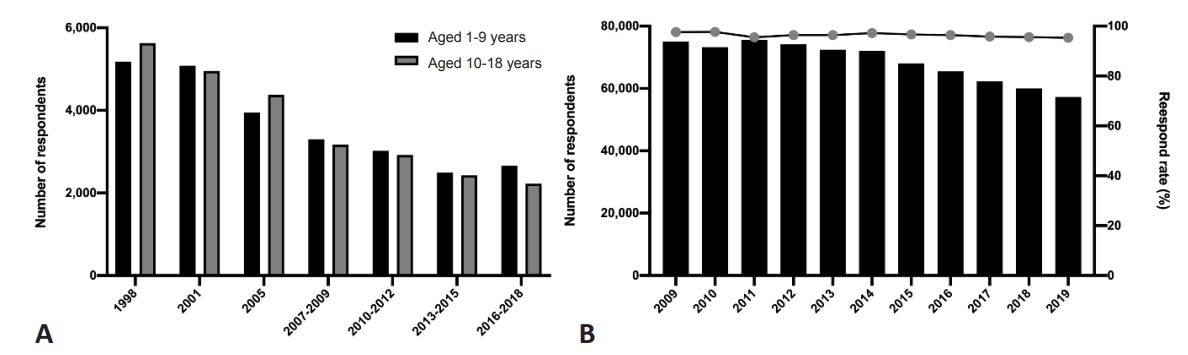
Table 1.
Table 2.
Table 3.
| Study | Survey | No. of subjects | Age (yr) | Key variables | Main findings | |
|---|---|---|---|---|---|---|
| Breakfast | ||||||
| Kim et al. (2019) [52] | KNHANES (2013–2015) | 1,281 | 12–18 | Frequency of breakfast, dietary intakea), nutrient intakeb) | EB group consumed significantly higher levels of most nutrients than SB group, except for vitamin A. | |
| Hong et al. (2019) [49] | KNHANES (2013–2014) | 1,831 | 6–17 | Frequency of breakfast, dietary intakea), nutrient intakeb), DD score | Percentages of subjects consuming less than 1/4 of the EAR of vitamins A, B1, B2, C, niacin, and iron were significantly lower in the FBG than the EB group. | |
| Yu and Yang (2019) [50] | KNHANES (2013–2015) | 1,325 | 6–11 | Frequency of breakfast, dietary habitsc), nutrient intakeb) | Significant association between frequency of EB and dietary factors of the parents | |
| Kye (2019) [53] | KYRBS (2018) | 53,642 | 12–18 | Frequency of breakfast, lifestyle factors, dietary habitsc) | Overweight or obese subjects were more numerous in the SB group than in the EB group. | |
| Risks of SB: intake of fruit less than one per day, intake of carbonated beverages more than one per day, intake of sugar-sweetened beverages more than three times per week in those who had not received nutritional and dietary education in school | ||||||
| Bae (2017) [51] | KNHANES (2013–2015) | 1,300 | 12–18 | Frequency of breakfast, dietary intakea), nutrient intakeb) | Significant association between EB and high nutrient intake | |
| Kim et al. (2016) [154] | KYRBS (2009–2013) | 359,264 | 12–18 | Frequency of breakfast, school performance, dietary intakea) | Significant positive association between school performance and EB and frequent consumption of fruits and milk | |
| Fast/processed food intake | ||||||
| Cha (2020) [61] | KYRBS (2018) | 28,911 | 16–18 | Frequency of fast-food intake, BMI | Positive association between intake of fast foods and BMI | |
| Park and Lee (2020) [155] | KYRBS (2019) | 57,303 | 12–18 | Frequency of fast-food intake, perceived stress, depression, suicidal ideation | Significant association between frequent consumption of convenience foods and poor mental health | |
| Hong (2019) [60] | KYRBS (2018) | 26,338 | 12–18 | Frequency of fast-food intake, smoking, alcohol, physical activity, BMI | Significant association between obesity and lifestyle factors: frequent consumption of fast foods, smoking, alcohol consumption, eating breakfast fewer than four times a week, eating fruit fewer than four times a week | |
| Lee and Kwon (2018) [62] | KYRBS (2017) | 62,276 | 12–17 | Frequency of fast-food intake, subjective happiness | Significant association between unhappiness and frequently eating at a convenience store | |
| An (2018) [63] | KYRBS (2016) | 65,528 | 12–18 | Frequency of fast-food intake, depression | Significant association between depression and frequent fast food consumption | |
| Kim et al. (2016) [154] | KYRBS (2009–2013) | 359,264 | 12–18 | Frequency of fast-food intake, dietary intakea) | Significant negative association between school performance and frequent intake of soft drinks, instant noodles, and fast- and convenience store foods | |
| Sugar beverage intake | ||||||
| Oh and Chung (2019) [68] | KYRBS (2014–2017) | 267,907 | 12–18 | Energy drink consumption, dietary intakea), dietary habitsc) | Significant association between higher energy drink consumption and higher intake of soda, sweet drinks, and fast food; skipping breakfast; and lower vegetable intake | |
| Wang et al. (2018) [67] | KNHANES (2013–2015) | 1,520 | 6–11 | Nutrient intakeb) | Average daily beverage intake: 131.75 g/day | |
| Average daily total sugar intake from beverages: 13.76 g/day | ||||||
| Significant association between high beverage intake and obesity | ||||||
| Hwang and Kye (2018) [70] | KYRBS (2015–2016) | 104,750 | 12–18 | Subjective health status | Significant association between high intake of soft drinks and subjective health status | |
| An et al. (2018) [63] | KYRBS (2016) | 65,528 | 12–18 | Depression | Significant association between depression and frequent consumption of carbonated drinks | |
| Kim et al. (2018) [76] | KYRBS (2017) | 62,276 | 12–18 | Parental education levels, subjective household economic status, subjective academic achievement, alcohol consumption, smoking, dietary habits | Significant association between high rate of sugar-sweetened beverage consumption and boys, higher household income, smoking, alcohol consumption, and SB | |
| Excess sodium | ||||||
| Lee et al. (2018) [77] | KNHANES (2008–2011) | 1,476 | 10–18 | Urinary sodium levels, BMI | Significant association between high urinary sodium excretion during 24 hr and overweight or central obesity | |
| Kim et al. (2018) [80] | KNHANES (2009–2010) | 718 | 10–18 | UNa/Ucr, fasting insulin level, glucose | Significant association between sodium excretion and insulin resistance | |
| Han et al. (2018) [81] | KNHANES (2010) | 578 | 12–18 | UNa/Ucr, fasting insulin level, glucose | Significant positive association between increased Na excretion and high risk of insulin resistance | |
| Kim (2018) [76] | KNHANES (2015) | 405 | 7–18 | Parents’ and children’s sodium dietary intake | Significant positive association between dietary sodium intake in study subjects and maternal dietary sodium intake | |
| So et al. (2017) [79] | KNHANES (2010–2013) | 1,738 | 10–18 | UNa/USG, BMI, WC, BP, total cholesterol, HDL-C, TG, LDL-C | Significant association between UNa/USG and MetS | |
| Nakitto et al. (2017) [156] | KNHANES (2013–2015) | 1,453 | 12–18 | Food insecurity, DD score, nutrient intakeb) | Both food secure and insecure subjects showed insufficient intake of vitamin A, vitamin C, and calcium and excessive sodium intake | |
| Lee and Kim (2016) [78] | KNHANES (2010–2011) | 1,467 | 10–18 | UNa/Ucr, sodium dietary intake, TBPF | Significant positive association between urinary and dietary sodium and adiposity | |
| Chun et al. (2016) [82] | KNHANES (2009–2010) | 1,353 | 12–19 | UNa/Ucr, UNa/USG, fasting insulin level and glucose | Significant positive association between urinary sodium excretion and insulin resistance | |
KNHANES, Korea National Health and Nutrition Examination Survey; KYRBS, Korean Youth Risk Behavior Web-based Survey; EB, eating breakfast; SB, skipping breakfast; EAR, estimated average requirements; FBG, family breakfast group; BMI, body mass index; WU, waist circumference; BP, blood pressure; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; LDL-C, low-density lipoprotein cholesterol; DD, dietary diversity; MetS, metabolic syndrome; TBPF, total body percent fat; UNa/Ucr, urinary sodium to urinary creatinine ratio; UNa/USG, urinary sodium to urinary specific gravity ratio.
a) Dietary intake of cereals, sugars and sweeteners, vegetables, fruit, milk, beverages, prepared and processed foods.
Table 4.
| Study | Survey | No. of subjects | Age (yr) | Key variables | Main findings | |
|---|---|---|---|---|---|---|
| Prevalence and trends in vitamin D status | ||||||
| Jung et al. (2018) [91] | KNHANES (2008–2014) | 39,759 | >10 | Serum 25(OH)D | Significant decreasing trend in mean serum 25(OH)D level of all age groups older than 7 yr | |
| Park et al. (2018) [92] | KNHANES (2008–2014) | 39,759 | >10 | Serum 25(OH)D | Significant decreasing trend in mean serum 25(OH)D level and increasing trend in prevalence of vitamin D deficiency in those older than 7 yr | |
| Hong et al. (2018) [157] | KNHANES (2008–2012) | 28,551 | All ages | Serum 25(OH)D | Parental influence on vitamin D status of offspring was greater in adolescents than in adults | |
| Byun et al. (2017) [93] | KNHANES (2008–2010) | 2,515 | 10–18 | Serum 25(OH)D | 73.3% of subjects had serum 25(OH)D lower than 20 ng/mL | |
| Significant association between low serum 25(OH)D levels and older age, female sex, urban residence, higher BMI, and sampling in winter | ||||||
| Association between vitamin D status and diseases | ||||||
| Cho et al. (2019) [97] | KNHANES (2008–2014) | 3,878 | 12–18 | Serum 25(OH)D, BMI, ALT, WC, fasting glucose, cholesterol, TG | Significant association between vitamin D deficiency and suspected NAFLD | |
| Choi et al. (2018) [100] | KNHANES (2010–2014) | 2,655 | 10–18 | Serum 25(OH)D, dental clinic visits, tooth brushing | Significant positive association between vitamin D status and risk of dental caries in boys | |
| Byun et al. (2017) [93] | KNHANES (2008–2010) | 2,515 | 10–18 | Serum 25(OH)D, AD, asthma | No significant association between vitamin D status and AD or asthma | |
| Yoo et al. (2016) [96] | KNHANES (2010) | 870 | 10–18 | Serum 25(OH)D, BP, BMI, WC, TG, cholesterol, fasting glucose | Significant association between high vitamin D level and decreased WC and BP | |
| Lee et al. (2015) [103] | KNHANES (2010–2012) | 2,526 | 10–20 | Serum 25(OH)D, Hb, BMI | Significant association between vitamin D deficiency and an increased risk of iron deficiency anemia in healthy females | |
Table 5.
| Study | Survey | No. of subjects | Age (yr) | Key variables | Main findings | |
|---|---|---|---|---|---|---|
| Prevalence and trends in iron status | ||||||
| Oh et al. (2018) [158] | KNHANES (2010–2012) | 2,487 | 10–20 | Dietary iron intake, menarche status, serum iron, TSAT, TIBC, ferritin, Hb | Sharply increasing trend in serum ferritin levels with progression to puberty | |
| Significant sex differences in ferritin from the age of 14 yr | ||||||
| Lim et al. (2015) [159] | KNHANES (2010–2012) | 2,196 | 10–20 | Serum iron, Hb, TIBC | Prevalence of anemia according to WHO criteria and own criteria (Hb level <2 standard deviations of age- and sex-specific values) was 3.5% and 3.8%, respectively | |
| Lee et al. (2014) [112] | KNHANES (2010) | 6,758 | >10 | Hb, transferrin saturation, serum ferritin, MCV, BMI, dietary intake | The overall prevalence of ID and IDA was 12.1% and 4.3%, respectively | |
| Significant association between IDA and low income, underweight or iron- or vitamin C-poor diet | ||||||
| Association between iron status and diseases | ||||||
| Chueh et al. (2018) [114] | KNHANES (2010–2012) | 2,918 | 10–18 | Serum ferritin, Hb, transferrin saturation, family history of IDA | Significant association between IDA and family history of IDA | |
| Jung et al. (2017) [160] | KNHANES (2009–2010) | 1,321 | 10–18 | Serum 25(OH)D, serum ferritin, Hb, BMC, daily intakes of total energy, protein, fat, and calcium | Significant positive association between the levels of Hb and BMC of the total femur and lumbar spine in boys | |
| Hong et al. (2017) [161] | KNHANES (2010–2012) | 619 | 8–15 (mo) | Serum iron, MCV, Hb, TIBC, feeding type, red meat intake, iron-rich food intake | Significant association between ID/IDA and prolonged breastfeeding and perceived inadequacy of red meat intake | |
| Lee et al. (2014) [115] | KNHANES (2010–2011) | 396 | 10–19 | BMI, serum ferritin, Hb, urinary cotinine, blood cadmium levels | Significant negative association between serum ferritin levels and blood cadmium concentration | |
| No significant association between anemia status and blood cadmium concentration | ||||||
| Sim et al. (2014) [116] | KNHANES (2010–2011) | 396 | 10–19 | Serum ferritin, urine cotinine, blood lead levels, BMI | Significant negative association between serum ferritin levels and blood lead levels in boys and premenarche girls | |
KNHANES, Korea National Health and Nutrition Examination Survey; TSAT, transferrin saturation; TIBC, iron-binding capacity; Hb, hemoglobin; WHO, World Health Organization; ID, iron deficiency; IDA, iron deficiency anemia; BMI, body mass index; MCV, mean corpuscular volume; 25(OH)D, 25-hydroxyvitamin D; BMC, bone mineral content.
Table 6.
| Study | Survey | No. of subjects | Age (yr) | Key variables | Main findings | |
|---|---|---|---|---|---|---|
| Association between obesity and environmental factors | ||||||
| Kim and Moon (2020) [120] | KNHANES (2001, 2005, 2007–2017)/NSHE (2007–2017) | 23,343/1,301,681 | 2–18/6–18 | BMI | Prevalence of overweight and obese subjects increased from 15.3% to 23.7% over the past 10 years | |
| Lee et al. (2020) [121] | KNHANES (2007–2015) | 14,482 | 2–18 | BMI, WHR, parental BMI, SES | Significant association between obesity and current maternal smoking habits, paternal education, and low family income | |
| Shin et al. (2018) [162] | KNHANES (2010–2013) | 1,567 | 10–19 | BMI, blood mercury levels | Significant association between total blood mercury quartile and abdominal obesity in boys | |
| Kang et al. (2018) [163] | KNHANES (2010–2011) | 1,304 | 12–18 | Birth weight, BMI, fat mass, lean mass | High birth weight can lead to obesity and increased fat mass but not lean mass | |
| Kim et al. (2017) [130] | KNHANES (2009–2010) | 982 | 12–19 | Lean mass, fat mass, bone mass, BMD, BMAD, total cholesterol, HDL-C, fasting glucose, insulin, serum 25(OH)D | Significant association between overweight/obese and bone mass and density | |
| Association between obesity and chronic diseases | ||||||
| Lee and Song (2020) [124] | KNHANES (2010–2014) | 8,153 | 10–18 | BMI, WC, BP, total cholesterol, HDL-C, TG, LDL-C, fasting glucose | Significant association between high WC in adolescents and increased CVR | |
| Park et al. (2020) [164] | KNHANES (2001–2005, 2015–2017) | 4,448 | 10–19 | ALT, BMI, WC | Prevalence of suspected NAFLD continues to increase in Korean adolescents | |
| Lee (2019) [165] | KNHANES (2016–2017) | 1,256 | 10–18 | BMI, WC, BP, total cholesterol, HDL-C, TG, LDL-C, fasting glucose, serum uric acid | Significant association between hyperuricemia and MetS, abdominal obesity, and BMI z scores | |
| Kim et al. (2019) [166] | KNHANES (2009–2011) | 763 | 10–18 | BMI, WC, BP, total cholesterol, HDL-C, TG, LDL-C, FEV1, FVC | Significant association between low lung function and MetS components | |
| An et al. (2018) [129] | KNHANES (2013–2015) | 975 | 10–18 | BMI, WC, BP, total cholesterol, HDL-C, TSH, fT4 | Korean children with abdominal obesity had increased TSH and decreased fT4 levels compared with normal-weight children | |
| Cho et al. (2018) [127] | KNHANES (2007–2014) | 1,326 | 10–18 | BMI, WC, BP, total cholesterol, HDL-C, TG, LDL-C, fasting glucose | Adolescents with severe obesity have more metabolic risk factors than adolescents with less severe obesity | |
| Jin et al. (2018) [128] | KNHANES (2013–2015) | 1,104 | 10–19 | TSH, fT4, BMI, total cholesterol, HDL-C, LDL-C, serum insulin level | Subclinical hypothyroidism was common in the obese group | |
| Kim et al. (2018) [167] | KNHANES (2008–2014) | 5,742 | 10–18 | BMI, WC, BP, total cholesterol, HDL-C, TG, LDL-C, fasting glucose, serum fasting insulin | Non-HDL-C level of 120 mg/dL for males and 150 mg/dL for females is the threshold between borderline high and high risk for MetS | |
| Choi et al. (2017) [168] | KNHANES (2013–2014) | 3,057 | 10–19 | WHR, BMI, WC | No significant difference found between the diagnostic power of WHR and that of BMI/WC when screening for MetS | |
| Yoon et al. (2017) [169] | KNHANES (2007–200) | 530 | 10–19 | BMI, WC, BP, total cholesterol, HDL-C, TG, LDL-C, fasting glucose, WHR, fasting glucose, ALT, insulin | High CMRFs were significantly observed in metabolically unhealthy obese children | |
| Chung et al. (2016) [170] | KNHANES (1998–2008) | 4,068 | 10–19 | WHR, BMI, WC, fasting glucose, TG, HDL-C, BP | Significant association between WHR and CMRFs (systolic BP, HDL-C, TG) in both non-overweight and overweight subjects | |
| Yu and Song (2015) [171] | KNHANES (2007–2010) | 2,958 | 10–18 | Dietary sodium intake, WC, BMI, WC, BP, total cholesterol, HDL-C, TG, LDL-C, fasting glucose | Three clustering patterns: high BP, dyslipidemia, and glucose abnormality | |
No significant association between glucose patterns and nutrient intake except for thiamin
KNHANES, Korea National Health and Nutrition Examination Survey; NSHE, National School Health Examination; BMI, body mass index; WHR, waist–height ratio; SES, socioeconomic status; BFP, body fat percentage; BMD, bone mineral density; BMAD, bone mineral apparent density; HDL-C, highdensity lipoprotein cholesterol; 25(OH)D, 25-hydroxyvitamin D; WC, waist circumference; TG, triglycerides; LDL-C, low-density lipoprotein cholesterol; BP, blood pressure; CVR, cardiovascular risk; ALT, alanine transaminase; NAFLD, nonalcoholic fatty liver disease; MetS, metabolic syndrome; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; TSH, thyroid stimulating hormone; fT4, free thyroxine; CMRFs, cardiometabolic risk factors; TG, triglycerides; TBPF, total body percent fat.
Table 7.
| Study | Survey | No. of subjects | Age (yr) | Key variables | Main findings |
|---|---|---|---|---|---|
| Kim (2019) [172] | KNHANES (2013–2015) | 752 | 9–11 | AD, nutrient intakea) | Significant association between AD and intake of high carbohydrate, low fat, low PUFA, and low n-3 FA |
| Kang et al. (2018) [149] | KYRBS (2012) | 76,980 | 12–18 | Asthma, dietary intakeb) | Significant association between high intake of fast food and asthma |
| No association between consumption of fruits, vegetables, or milk and asthma | |||||
| Lee et al. (2017) [144] | KNHANES (2007–2012) | 2,015 | 1–3 | AD, feeding practices | No significant association between exclusive breastfeeding or duration of breastfeeding and incidence of AD |
| Kim et al. (2017) [148] | KYRBS (2014) | 72,060 | 12–18 | Allergic diseases (AD, asthma, AR), dietary intake | Significant associations between frequent consumption of fast food, snacks, sweetened beverages, vegetables, or fruits and allergic diseases |
| Kim et al. (2016) [173] | KNHANES (2010–2012) | 3,040 | 4–13 | Allergic diseases (AD, asthma, AR), nutrient intake | No significant findings between AD and nutrient intake |
| Significant association between asthma and high intake of vitamin A | |||||
| Significant association between AR and high fat, protein, thiamine, and niacin intake and, low-carbohydrate intake |






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


