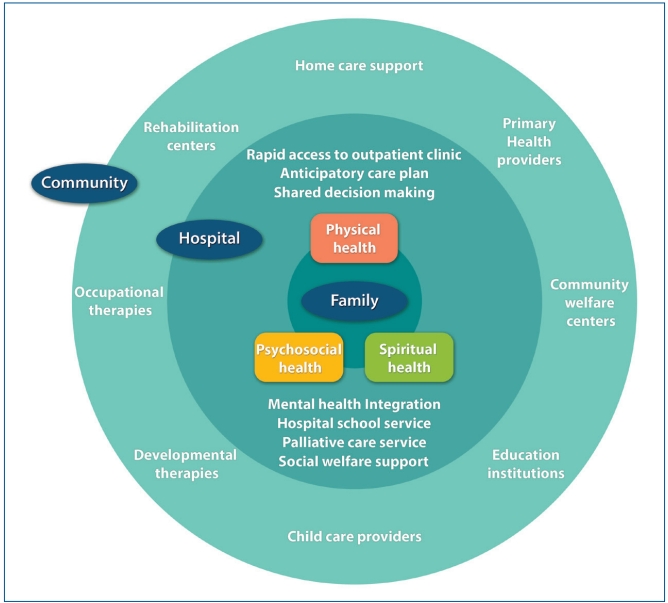
Graphical abstract. The concept of integrative care for children with medical complexity
With medical advancements, the survival rates of pediatric diseases have increased. However, many children still suffer from life-threatening conditions such as cancer, cardiac disease, congenital malformation, neuromuscular disease, and genetic conditions. More than 1,300 children with these conditions die each year, and 130,000 children in the Republic of Korea are currently living with medical complexity [1].
Children with medical complexity (CMC) have uncertain prognoses and require intensive treatment and long-term care, which greatly affect the physical, mental, and social suffering of them and their families. Nevertheless, current healthcare systems in Korea are not well-designed for CMC, which results in fragmented, uncoordinated, and emergency-driven care. Children and families have inadequate caregiving support and must navigate the complex care process themselves while meeting with dozens of healthcare professionals in the hospital and community settings [2].
Integrative care is a fundamental concept of high-quality healthcare for CMC and their families. The core components of integrative care for CMC are follows: (1) an anticipatory care plan is developed by the healthcare team so that acute nonsevere problems can be managed urgently in the outpatient setting; (2) decision-making is supported and coordinated among patients, their families, and multiple healthcare professionals; and (3) an interdisciplinary team comprehensively addresses the patients and families’ physical, psychosocial, and spiritual needs [3-5].
Since CMC often experience medical problems that may lead to a serious decline in their health, it is important that they have rapid access to an outpatient clinic that can address their needs in person or on the phone. Since many CMC have chronic conditions that affect multiple organ systems and rely on a number of specialists, care coordination among the members of the child’s healthcare team is critical for care planning decisions to ensure that appropriate care plans are designed and executed. Key aspects of coordination include a designated staff person who acts as a care coordinator for CMC and the families and approaches the child comprehensively; that is, the provider systematically assesses each problem and need in the context of the child’s overall health and well-being. A randomized controlled trial of “enhanced” primary care for CMC with collocation of specialty and comprehensive services found a significant decrease in the incidence of serious illnesses, number of emergency department visits and inpatient admissions, and medical expense [4].
Patient- and family-centered decision-making is also very important when integrative care is provided for CMC. Patient- and family-centered decision-making is a process in which healthcare provider, patients, and families work together to make decisions regarding evaluations, treatments, and care plans based on clinical evidence that balances risks and expected outcomes with family preferences and values. Through this process, families can maintain control during the illness trajectories and healthcare providers can tailor the care or treatment to the needs of the individual.
Addressing psychosocial factors that impact wellness and resilience for children and their families is also an essential component of the integrative care concept [5]. CMC and their families may encounter several internal (i.e., emotional and behavioral) and external (i.e., interpersonal, financial, housing, and educational) psychosocial factors that can affect their health and wellness. Integrative care team members can promote protective psychosocial factors and ameliorate risk factors as part of coordinated comprehensive chronic care. Care coordinators can assist with identifying and strengthening protective family and peer relationships to help support and monitor strategies and interventions with child care providers, schools, home health agencies, social service workers, and mental health providers. Mental health integration is a fruitful approach and model for delivering comprehensive care for children with serious illnesses and their families. Practices with on-staff mental health providers or real-time access to mental health support have enhanced systematic assessments of psychosocial health care needs and timely access to mental health services for children and their families.
CMC often require community-based services to optimize their health, functioning, and well-being. Examples of community-based services include home and school nursing, personal care attendants, equipment vendors, and occupational, physical, and speech therapies. It is also important that hospitals, schools, and day care centers in the community cooperate so that children can maintain academic achievement and good relationships with their peer groups. The arrangement between hospitals and community-based services may be especially important as CMC return home after a long-term inpatient stay.
Since fee-for-service payment is incurred by separate medical services, an integrative care model is poorly reimbursed since much of the care is not delivered during face-to-face encounters and counting the number of services is difficult. To provide highquality care to CMC and their family members, it is necessary to change the medical system, along with training medical staff consisting of an interdisciplinary team.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


