Materials and methods
1. Subjects and methods
Patients with CHD who underwent percutaneous stent implantation between March 2012 and August 2016 in the Department of Pediatric Cardiology at Sejong General Hospital were enrolled in this study. A total of 75 patients with 81 vascular lesions underwent implantation of vascular stents; the sites of the lesions were as follows: (1) PAS group, 56 lesions in 51 patients; (2) CoA group, 5 lesions in 5 patients; (3) Fontan group, 13 lesions in 12 patients; (4) ductal stent group, 3 lesions in 3 patients; and (5) other CHD group, 4 lesions in 4 patients.
Patients' medical records were retrospectively reviewed for demographic data.
To evaluate the effectiveness and safety of catheterization, all catheterization data were obtained before and after stent implantation. The following parameters were recorded: minimum lumen diameter (MLD), systolic pressure gradient (PG) in the stenotic pulmonary artery and right ventricular to aortic pressure ratio in the PAS group; MLD and systolic PG at the narrowest portion of the aorta in the CoA group; mean PG in the Fontan group; and MLD and arterial oxygen saturation in the ductal stent group. All of patients in our study had a full preprocedural evaluation, including laboratory tests, chest radiography, electrocardiogram, echocardiography, and computed tomography angiography. Stent implantation was performed with the following indication in our study: in PAS group, PG on stenosis >20 mmHg, perfusion difference in lung perfusion scan (LPS) >2:1, or right ventricular to aortic pressure ratio >0.6; in CoA group, PG >15 mmHg; in Fontan group, mean PG >2 mmHg or LPS >2:1; in ductal stent group, although balloon valvuloplasty for pulmonary atresia with intact ventricular septum was performed, SaO2 <80% after weaning of prostaglandin E1. The indication for reintervention is the same as above, but also includes serial redilation cases. We collected the time from stent implantation to the next reintervention for patients requiring reintervention. For evaluating the effectiveness after stent implantation in each group, LPS, computed tomography angiography, and echocardiography were done before and after the procedure. We also collected data concerning complications of the stent implantation.
We used various types of stent, including Omnilink (Abbott, Abbott Park, IL, USA), Express (Boston Scientific, Marlborough, MA, USA), and medium sized Genesis stents (Johnson and Johnson, New Brunswick, NJ, USA), which can be expanded to a maximum of 12 mm in diameter. In some cases, balloon angioplasty was performed first to make it easier to introduce the stent. We tried using cut Palmaz 4014 or 5014 stents (Johnson and Johnson) in the pulmonary position in several cases, but this approach was abandoned because balloon perforation occurred frequently.
This study was reviewed and approved by the Institutional Review Board of Sejong General Hospital (approval number: 1741).
2. Statistical analysis
Data are expressed as mean±standard deviation for continuous data or as numbers for categorical data. The acute outcomes of stent implantation were analyzed using the paired t test. The SPSS software package (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. A P value <0.05 and a confidence interval of 95% were considered statistically significant.
Discussion
The aim of this study was to analyze the short-term outcomes of stent implantation in different groups of patients with CHD in order to assess the efficacy and safety of the method, and also to describe the midterm outcomes of stent implantation in a single institution over a 4-year period. As in previously published reports, our results from patients with CHD occur immediately after stent implantation and at follow-up in our hospital were generally excellent.
Stents have contributed greatly to the development of interventional catheterization for CHD, especially PAS. Stent implantation can be considered universally superior to balloon angioplasty in the aspect of recoil. In PAS patients, elevated right ventricular pressure is associated with right ventricular failure, arrhythmias and sudden cardiac death. Aggressive management is required to improve the patient's hemodynamics.
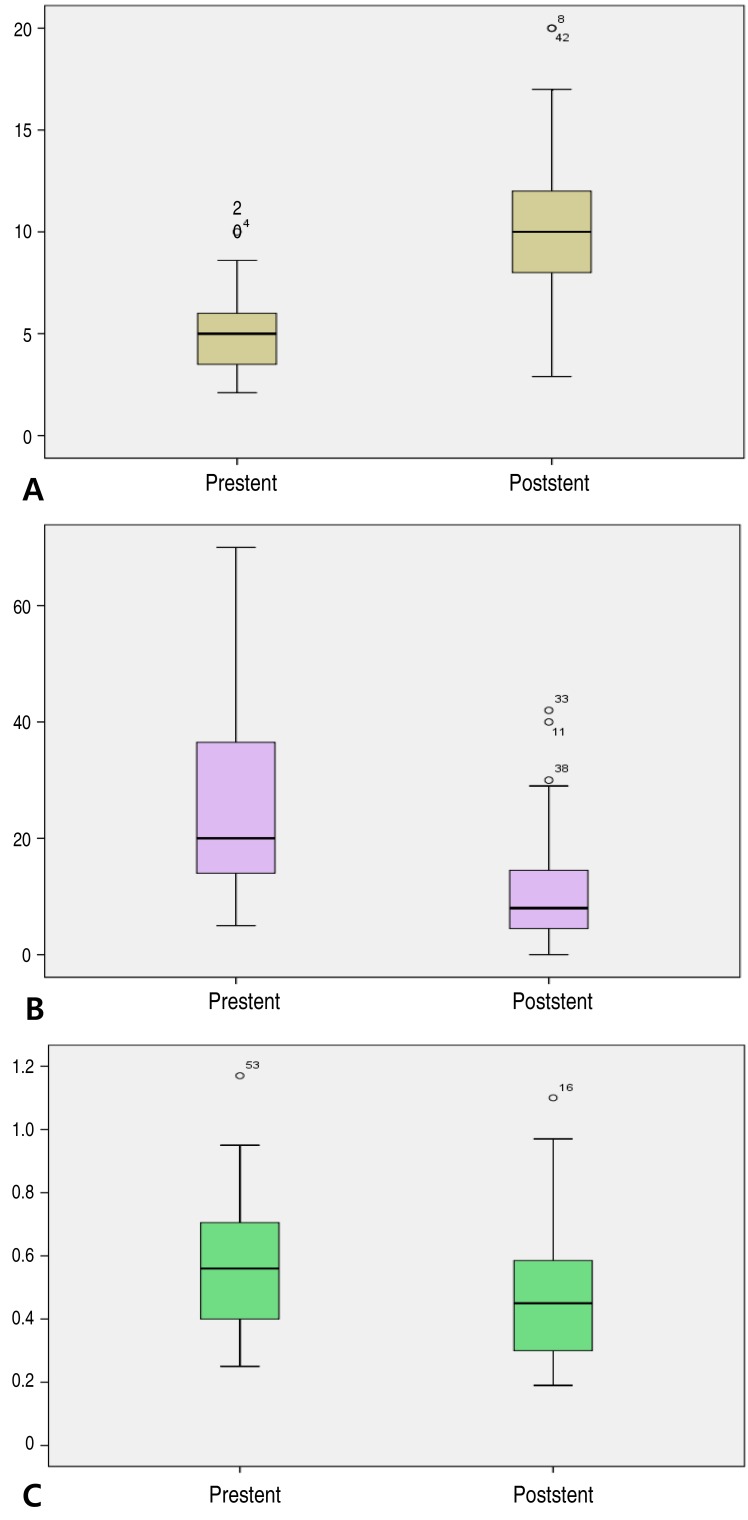
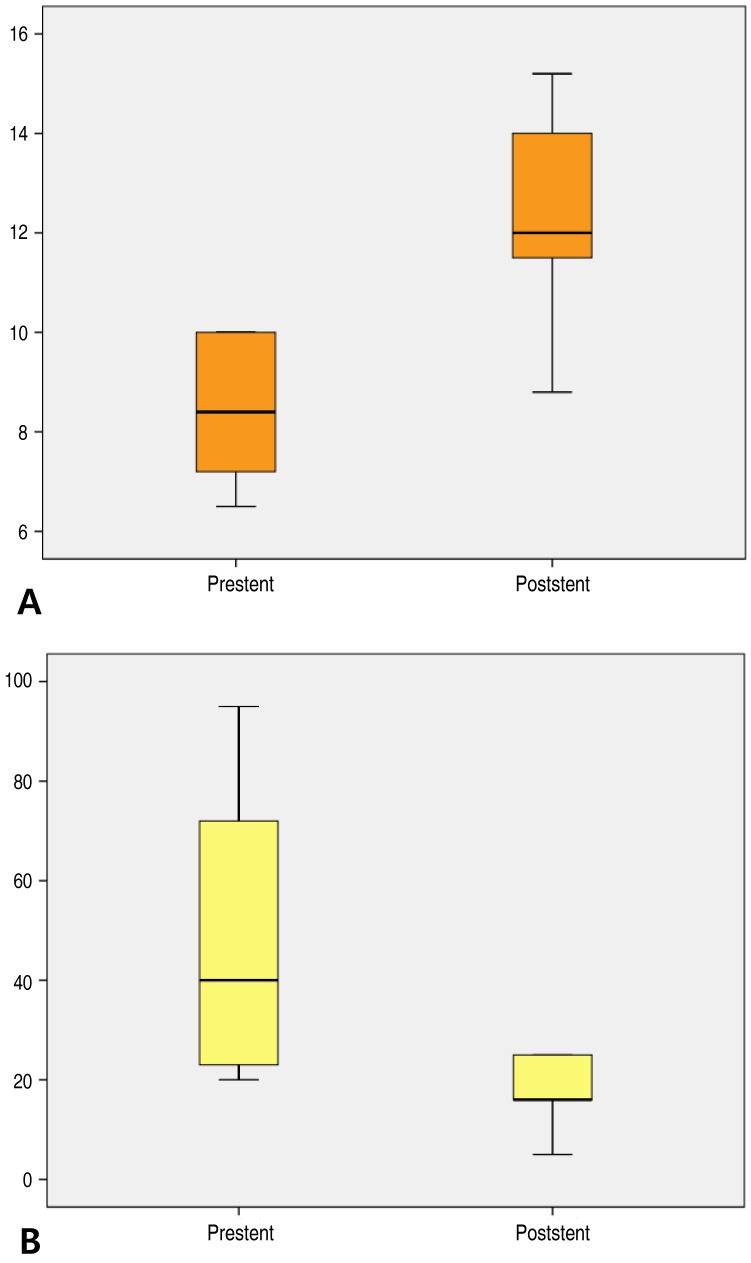
1,3) Therefore, the treatment of PAS is critical for these patients. In our study, PAS was the most common lesion over all stent implantations for CHD. We evaluated the effect of stent implantation on PAS in terms of the increase in the MLD of the stenotic lesions, the decrease in systolic PG, and the decrease in right ventricular to aortic pressure ratio; our stent implantation procedures yielded statistically significant successful outcomes for all 3 parameters. These results are consistent with studies by other investigators.
2,3,6,7,8,9,10) However, the right ventricular to aortic pressure ratio of some patients did not decrease significantly after the procedure, probably because of residual distal PAS.
Percutaneous stent implantation can be used to reduce the blood PG and to relieve symptoms associated with native CoA or residual coarctation after surgical intervention. According to previous data, stent implantation is similarly as effective as surgical repair with respect to acute and intermediate-term follow-up outcomes.
11) In our study, stent implantation showed good efficacy with an acceptable midterm outcome in all patients, except for 1 patient with abdominal aorta stenosis who was suspicion of Takayasu's arteritis, and underwent balloon angioplasty for restenosis 14 months after stent implantation. In a recent report, self-expandable stents demonstrated good results for native and recurrent CoA.
12) Two patients of our cases underwent stent implantation using self-expandable stent (Hercules). One patient had a excellent outcome, while the other patient received redilation after 14 months of stenting. Although the exact mechanism is unknown, restenosis of this patient is thought to be caused by chronic inflammation of vessels due to Takayasu's arteritis.
In Fontan patients, stent is used to increase mean diameter and reduce PG in patients with cavopulmonary pathway obstruction.
13) In our study, the most patients received stent implantation in branch pulmonary artery and 2 patients received stent in Fontan conduit and right SVC each other, and all patient experienced the significant decreased Fontan pathway pressure after stent insertion and improved hemodynamics. Some of them showed significant PG on LPA (PG>2 mmHg), but relatively good sized diameter superoinferiorly in anteroposterior projection. However, computed tomography showed significant stenosis on LPA anteroposteriorly, therefore, we implanted stent on LPA. Three-dimensional rotational angiography is beneficial for the diagnosis and interventional procedure in this situation. One of our patients with hypoplastic left heart syndrome in Fontan group had stent implantation on LPA, followed by stenting on descending aorta because LPA stent compressed descending aorta. Tiny hole developed between 2 stents, but was not significant hemodynamically.
Stent implantation in a patent ductus arteriosus is an alternative to surgical palliation in neonatal patients with ductal-dependent pulmonary circulation.
14,15) Optimal diameter of stented ductus was not established, and one of our patients showed significant pulmonary overflow after 5-mm stent, and needed a transcatheter closure of stented ductus with an Amplatzer vascular plug II (St. Jude Medical, St. Paul, NN, USA) in a month after confirming adequate right ventricle as a pulmonary pump. We supposed a 4-mm stent would be an optimal size for ductal stenting in PA IVS.
PVS is rare, presenting either as primary PVS or secondary PVS after TAPVR repair surgery. In many cases, PVS is progressive in nature and can result in secondary pulmonary hypertension and RV failure. Since PVS is a challenging lesion to treat whether it occurred congenitally or postoperatively. Restenosis rate and overall mortality is still high. In our study, 2 patients underwent stent implantation for recurrent PVS despite serial balloon angioplasty or reoperation. Their immediate outcomes were good, however, they needed further intervention for PVS. And one of them died 8 days after stenting. This patient with congenital PVS was repaired surgically in neonate, and PVS developed, which recurred despite one more surgery and several times of balloon dilatation. Therefore, stent implantation was performed finally, but the patient died because of pulmonary edema and sepsis.
Stenting of the systemic ventricular outflow tract can be a potential therapeutic option in rare patients with CHD who developed significant ventricular hypertension or severe ventricular dysfunction due to outflow obstruction.
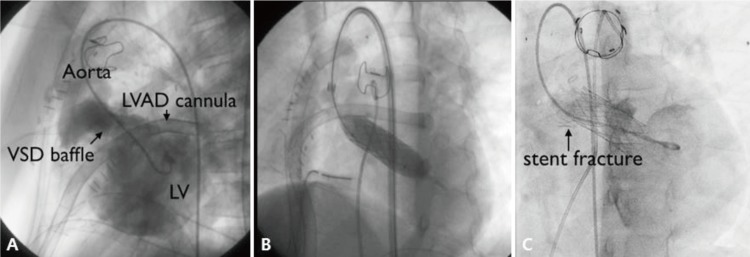
16) In our study, 1 patient with PA, DORV and remote VSD received LVOT stent implantation for LVOT stenosis after corrective surgery. Before stenting, this patient showed severe LV dysfunction and low cardiac output, requiring left ventricular assisted device support (LVAD). However, after relieving LVOT obstruction with LVOT stenting (Palmaz 4014 stent), PG of LVOT was decreased 45 mmHg to 7 mmHg significantly and improved LV function. It could be possible to wean LVAD the next day (
Fig. 4). Stent fracture was observed on the distal portion twelve months after stenting, but the PG on cardiac catheterization was insignificant (<20 mmHg). Follow-up echocardiogram in 4 years also showed no significant PG on LVOT stent.
Several complications related to stent implantation have been reported in other studies: stent migration during deployment, slippage of stent from balloon, late stent migration, stent fracture, embolism, lung congestion, gastrointestinal bleeding, paralysis of the brachial plexus, perforation of the pulmonary artery, and hemoptysis. In some previously reported multicenter studies, up to 23.1% of patients experienced an adverse event, 2.8% of patients required surgical treatment, and 10% experienced a high severity event.
2,3,6,7,8,9) In our study, complication rate was 6.6%, which is lower or similar to other institutes. And unlike other studies, there were no severe complications such as massive bleeding, bacteremia, or death related to procedure. Although stent migration occurred in 3 patients, repositioning was successful in all. In our cohort, overall survival rate was 98.6% (74 of 75). There was no death apparently associated with the stents or procedures in our study.
In many studies including our study, efficacy and safety of the stent is amply demonstrated. However, mid and long-term outcomes are not sufficiently completed. Although stents make up for shortcoming of balloon angioplasty in aspect of recoil, in-stent stenosis is also outstanding issue to resolve. In the studies of Tomita et al.
2) and Ing et al.
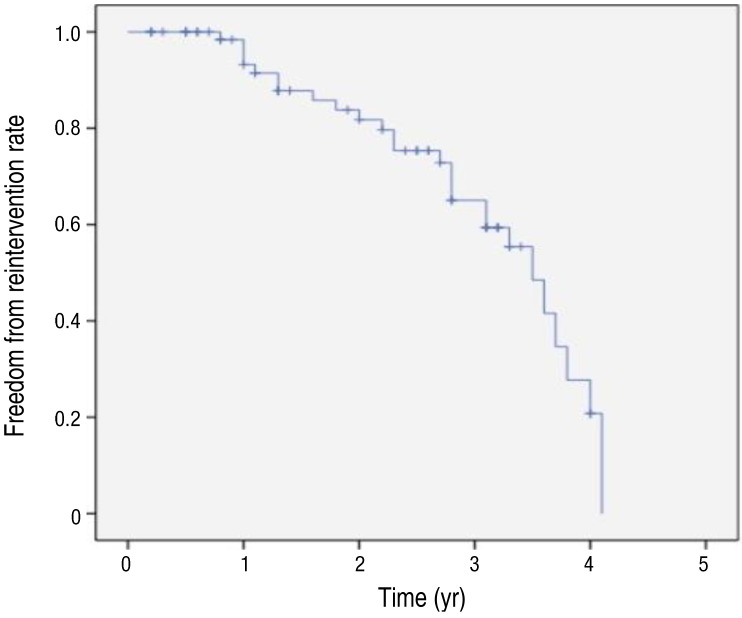
17), redilation rates were 42.3% (108 of 255) and 58.9% (43 of 73), respectively. In our study, 30.6% of patients (23 of 75) needed redilation after stent implantation. Especially, in case of early age intervention, as the younger patients grow, further dilation of the stent will be required to compensate for their somatic growth or because of in-stent restenosis.
1,2,17) According to recent study, stents with a larger diameter appear to remain patent longer than small stents, allowing a long interval free from reintervention.
2) However, deployment of an oversized stent may be potentially harmful to the vessel in small child. So in some cases, repetitive in-stent redilation can be an effective method after small stent insertion. In our study, serial redilation after stent implantation was the most common reason for reintervention, and only in 3 cases, there were stent-in-stent procedures due to intimal growth. However, our study differs from other studies in the following point. In our study, there were many cases of planned serial redilation for reduce the risk of vessel rupture. These results would influence the value of freedom from reintervention of total patients in our study (
Fig. 3). And to overcome the problem of restenosis, it will be necessary to carry out close long-term follow-up and to determine the mechanism of restenosis.
The Palmaz stent is still the most commonly used for lesions of great vessels, such as pulmonary arteries, aorta, and systemic veins.
2,8,17) In our study, the Omnilink (premounted stent) was the most commonly used, followed by the Express (premounted stent). This differs slightly from previous studies, because, unlike other countries, the types of stent that can be used for treatment in Korea are limited. Stents with maximum expanded diameter >15 mm were not available in Korea, apart from the Palmaz 4014 or 5014 stent, which was used for CoA but was too long for pulmonary artery deployment. We tried using cut Palmaz 4014 or 5014 stents in the pulmonary position in several cases, but this approach was abandoned because balloon perforation occurred frequently.
New stents have been developed and have emerged with promising results. In practice, many of the types of stent used currently in children are used “off-label,” because they have not been approved for vascular lesions in children.
This study had several limitations. First, it included only a relatively small cohort and it was retrospective in design. Second, since the procedures were performed by more than 2 operators, it is possible that the postprocedural follow-up was nonuniform. Third, there is a lack of analysis for related factors or mechanism about in-stent restenosis. Furthermore, at present, several stents, such as the P308E (Cordis, Miami, FL, USA), Genesis XD (Cordis Corp., Bridgewater, NJ, USA), or Valeo (Bard Peripheral Vascular, Tempe, AZ, USA), are not available in Korea. The limited supply of stents remains a challenge to be overcome in order to achieve more successful outcomes of stent implantation.
The results of our study showed that stent implantation is not only an effective and safe therapeutic modality for the treatment of vascular stenosis, but also an essential strategy in patients with CHD. However, we have no long-term results from this procedure; accordingly, the follow-up will continue so that we can detect and manage any unexpected long-term complications that may occur.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


