Introduction
Development of renal replacement therapies such as hemodialysis (HD), peritoneal dialysis (PD) and renal transplantation in children with end-stage renal disease (ESRD) has resulted in improved long-term survival1). However, ESRD influences virtually every organ system and thus, has a major impact not only on morbidity and mortality but also on the quality of life (QoL) of children with ESRD2).
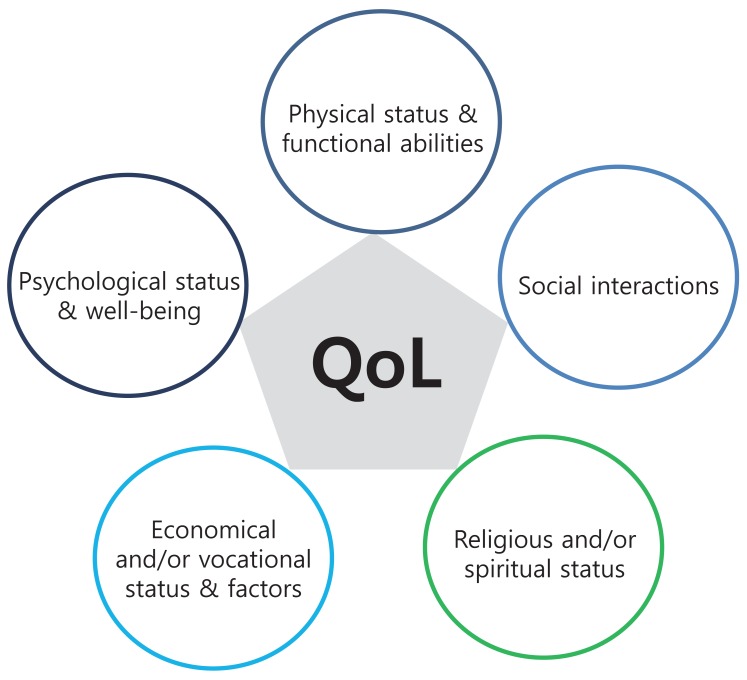
In general, QoL can be defined as a patient's sense of well-being and functional outcome within several life domains including physical, psychological status, and social interaction3). QoL should not be confused with the concept of standard of living, which is based primarily on income. Based on previous studies of QoL, Spilker4) concluded that QoL is a multifaceted/multidimensional phenomenon and there are next five domains in a conceptual definition of QoL: 1) physical status and functional abilities, 2) psychological status and well-being, 3) social interaction, 4) economic and/or vocational status, and 5) religious and/or spiritual status5) (Fig. 1).
Actually, we, pediatric nephrologists, should confront a lot of medical problems in children with ESRD. These problems consist of general symptoms such as fatigue and malaise, hematologic problems such as anemia and dysfunction of platelet, gastrointestinal problems such as anorexia, nausea and vomiting, electrolyte imbalances such as hyperkalemia, metabolic acidosis, hyponatremia, hyperuricemia and hyperphosphatemia, genitourinary problems, nerve system, endocrine, musculoskeletal, cardiovascular, and dermal problems, etc. Except for these medical problems, however, there are additional problems that we must resolve in children including the change of body image, too many medicines, side effects, psychiatric problems, growth, and development. If we don't have concern about these issues, normal growth and development in these children cannot be accomplished. Kurtin et al.6) suggested that the definition of success in the care of pediatric ESRD patients should not be limited to mortality rates, but must include the degree to which these children are allowed to grow, develop, and behave in the same manner as their healthy peers.
The goal of this review was to help the understanding of clinical usefulness of assessment of QoL in children and adolescents with ESRD.
QoL in adults with ESRD
The QoL of adults with ESRD has been evaluated more comprehensively than in children. In 1985 Evans et al.7) evaluated the QoL of 859 patients undergoing dialysis or transplantation. They concluded that transplantation can give better QoL than dialysis because QoL of transplant recipients compared well with that of the general population, whereas patients with dialysis did not work at the similar level as people in the general population. In the CHOICE Health Experience Questionnaire (CHEQ) study, the difference of QoL according to dialysis modality in adults with ESRD was evaluated by 36-Item Short-Form Survey (SF-36) and it was reported that PD can give better QoL than HD in various domains including physical functioning, bodily pain and emotional functioning8). In 2002, Kidney Disease Outcomes Quality Initiative (K/DOQI) reported that impairment in functioning and well-being are associated with worse outcomes in chronic kidney disease (CKD) and compared with healthy population, dialysis patients tend to have more dysfunctions and limitations of behavior due to more bodily pain, poorer vitality, and poorer general health9). So, K/DOQI Clinical Practice Guidelines for CKD recommended that patients with glomerular filtration rate (GFR) <60 mL/min/1.73 m2 should undergo regular assessment for impairment of functioning and well-being9). In Korea, Park et al.10) suggested that lower residual renal function is a risk factor for depression and impaired QoL in Korean PD patients.
Pediatric QoL tools
Up to the present, several pediatric QoL tools have been developed such as these lists; Child Health Questionnaire (CHQ), Child Health and Illness Profile-Adolescent Edition (CHIP-AE), Dartmouth Primary Care Cooperative Functional Health Assessment Charts (COOP), Functional Status II (R), Pediatric Quality of Life Inventory (PedsQL) and The Vineland Adaptive Behavior Scale (VINELAND).
The CHQ consists of 12 domains of health status (physical functioning, limitations in schoolwork and activities with friends, general health, bodily pain, discomfort, limitations in family activities, emotional/time impact on the parent, impact of emotional or behavior problems on school work and other daily activities, self-esteem, mental health, behavior, family cohesion and change in health) and is suitable for children aged 10 to 19 tears11). The CHIP-AE is 6 domain/153 item self-report instrument (discomfort, satisfaction, disorder, achievements, resilience and risk) and sensitive to age, gender and socioeconomic influences12,13). The COOP chart system has 6 domains of health status including physical fitness, emotional feeling, school work, social support, family communication, and health habits14). The VINELAND is suitable for evaluating both handicapped and nonhandicapped persons from birth to age 19 years unlike the other QoL instruments15). PedsQL 4.0 Generic Core Scale created by Varni et al.16) is a 23-item generic health status instrument that assesses five domains of health including Physical, Emotional, Psychosocial, Social and School functioning in children and adolescents ages 2 to 18 years.
Although these modules have internal reliability and clinical validity and can be completed easily by children and their parents, they have some limitations because they were not disease-specific module. After then, Varni et al.17-20) have developed disease-specific modules to assess QoL in children with chronic diseases such as ESRD, asthma, cancer, and rheumatoid arthritis.
The 34-item PedsQL 3.0 ESRD Module developed in 2002 includes 7 scales: 1) general fatigue (4 items), 2) about my kidney disease (5 items), 3) treatment problems (4 items), 4) family and peer interaction (3 items), 5) worry (10 items), 6) perceived physical appearance (3 items), and 7) communication (5 items). This module consists of 4 age categories of 2-4, 5-7, 8-12, and 13-18 years. The scales are composed of both the child-self report and parent-proxy report formats for children aged 5 to 18 years and a parent-proxy report format for children aged 2 to 4 years. Items are reverse-scored and linearly transformed to a 0-100 scale (0=100, 1=75, 2=50, 3=25, 4=0). Higher scores indicate better health-related QoL. In our previous study, we translated the original English version of the PedsQL 3.0 ESRD into new Korean version based on the guideline of linguistic validation provided by the original developer (Mapi Research Trust, Lyon, France; on behalf of Dr. James W. Varni, copyright owner in the PedsQL)21) (Suppl. 1).
Studies of QoL in children with ESRD
Unfortunately, there are few studies of QoL in children with ESRD because first, it is very difficult to obtain suitable questions for children and second, proxy assessment is always needed. Initially, there are several limited studies of qualitative status in children with ESRD instead of typical QoL. Morton et al.22) reported that living with parents, lack of experience of close relationship, lack of educational qualifications and unemployment were more common in young adults with ESRD. In other study, 30% of adolescents with ESRD were neither enrolled in an educational program nor were employed23).
Recently, there have been several attempts to quantitate in systematically analyzable terms, the net outcome of a disease and its treatment on the patient's perception of his/her ability to live a useful and fulfilling life during childhood. In 1994, Kurtin et al.6) created parent-completed questionnaire validated in the Children's Health and Quality of Life Project and suggested that less compliant adolescents consistently reported more pain and poorer general and mental health than more compliant adolescents, as well as lower family involvement. It was also reported that QoL scores of children with ESRD were considerably lower than healthy controls24). In addition, Marciano et al.25) suggested that children with CKD showed a higher proportion of behavioral and emotional disorders and there was a negative correlation between the presence of behavior and emotional disorders and QoL score.
There have been several studies of difference of QoL between treatment modalities such as dialysis and transplantation in children with ESRD. According to study of QoL in children with ESRD using CHIP-AE, transplantation can produce improved physical activity, better work performance, more satisfaction, and less discomfort compared with dialysis26). In other study using PedsQL module, transplant patients reported better physical and psychosocial health than dialysis patients24). In addition, pediatric kidney transplant recipients also reported a higher QoL score than other published studies of chronic illness cohorts27).
Some studies have been reported the difference of QoL between child-self and parent-proxy reports. McKenna et al.28) reported that caregivers score their children lower in almost all categories than the child-self reports. On the other hand, Goldstein et al.29) reported that although parent-proxy reports show a positive impact from renal transplantation on the majority of QoL domains compared with dialysis, child-self reports show nonsignificant differences in favor of renal transplantation. Therefore, Buyan et al.30) concluded that parent-proxy scores on the QoL were not equivalent to child-self scores and that evaluating both children's and parents' perspectives were important.
Comorbidities including cardiovascular, gastrointestinal, endocrinologic, hematologic and neurologic disorders can be also one of the significant factors to decide the QoL in children with ESRD. Especially, hypertension, diabetes, and cardiovascular disorders have been regarded as the leading comorbidities in developing countries31). Khan32) classified patients into high, medium and low risk groups according to comorbidity and age and reported the significant difference of patients' perception of health score among the 3 risk groups.
In 2012, we published a cross-sectional study of the Korean translations of the PedsQL ESRD module comparing child-self reported and parent-proxy reported HRQoL of children with ESRD based on a national-wide pediatric ESRD registry, the so called 'The Korea Pediatric CKD registry'21). Participants included children aged 2 to 18 years who received maintenance dialysis treatment or renal transplant care for at least 6 months and their parents. Total 92 pediatric patients (11 HD, 44 PD, and 37 transplant) were enrolled. We reported that patients with PD had better QoL than HD in several domains (including Treatment problems in the child-self reports, About my kidney disease and Worry in the parent-proxy reports) and transplant patients had better HRQoL than dialysis patients in one domain of the child-self report (Treatment problems) and in two domains of the parent-proxy reports (About my kidney disease and Worry). However, there were no significant differences in the total QoL scores of the child-self reports between the PD and transplant patients.
Conclusions
Compared with adults, studies of QoL in children with ESRD have been not popular yet. However, we should consider that assessment of QoL can be essential to achieve normal growth and development in children with chronic diseases including ESRD. In addition, although various assessment tools for children have been recently developed, the optimized QoL instrument in our country should be developed to overcome the language problems and cultural gap. A larger, longitudinal prospective study is needed in the future.



 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


