Factors associated with thiamin deficiency in pediatric patients with heart disease and receiving diuretics: a single-center study
Article information
Abstract
Background
Thiamin deficiency (TD) manifesting clinically as wet beriberi can significantly impair a patient's cardiac function. Children with heart disease who are receiving diuretic treatment may be at increased risk for severe clinical manifestations of TD.
Purpose
This study aimed to determine the prevalence of TD and evaluate the association between various factors with thiamin status in pediatric patients with heart disease undergoing diuretic treatment.
Methods
Children with heart disease aged 1 month to 15 years who exhibited increased pulmonary blood flow or congestive heart failure (CHF) and had been taking diuretics for at least 1 month were recruited. Data regarding their heart condition, treatment, dietary intake, anthropometry, and symptoms and signs of TD were collected. An erythrocyte transketolase activity assay after the addition of exogenous thiamin pyrophosphate was used to assess thiamin status. Left ventricular ejection fraction and N-terminal pro-brain natriuretic peptide levels were indicators of cardiac function and laboratory evidence of CHF, respectively.
Results
A total of 68 participants were recruited, of whom 10 (15%) had TD. TD was not associated with a CHF exacerbation. An adequate dietary thiamin intake was associated with a better thiamin status (β=-0.37, P=0.003), while increasing age was linked to a poorer thiamin status (β=+0.40, P=0.001).
Conclusion
TD was present in 15% of pediatric patients with heart disease who were receiving diuretic treatment. An adequate dietary thiamin intake appeared to have a protective effect against TD, while increasing age was associated with a poorer thiamin status.
Key message
Question: Are pediatric patients with heart disease who are receiving diuretics at risk of thiamin deficiency (TD)?
Finding: Fifteen percent of the patients had TD. TD was associated with inadequate dietary thiamin intake and increasing age.
Meaning: The thiamin pyrophosphate effect should be assessed in those with high risk of TD. Dietary counseling should be emphasized to ensure adequate dietary thiamin intake.
Graphical abstract
Introduction
Thiamin is a water-soluble vitamin that participates in several oxidative decarboxylation reactions involved in glucose metabolism, the pentose phosphate pathway, and the citric acid cycle [1,2]. Inadequate dietary thiamin intake, impaired intestinal thiamin absorption, or increased thiamin loss can lead to thiamin deficiency (TD). TD can present as dry beriberi or wet beriberi. Dry beriberi primarily affects the neurological system, while wet beriberi primarily affects the cardiovascular system. Clinical manifestations of wet beriberi include arrhythmia, lactic acidosis, respiratory distress, and congestive heart failure (CHF) [2,3].
Thiamin is abundantly found in meats, whole grains, legumes, sunflower seeds, and vegetables, and consuming these foods is encouraged to meet the daily thiamin requirement. However, antithiamin factors present in certain foods can inhibit intestinal thiamin absorption. These include heat-labile thiaminases found in raw fish and shellfish, as well as heat-stable thiamin antagonist associated with tannic and caffeic acids [3]. The human body has a limited capacity to store thiamin, and excess thiamin is excreted via urine [2,4]. Diuretics can increase urinary thiamin loss in humans and animals, as demonstrated in studies by Rieck et al. [5] and Lubetsky et al. [6], respectively.
Adult patients with CHF who are on chronic diuretic therapy are at risk of TD [7]. Lymphatic congestion, which can occur as a complication of CHF, may further impair intestinal thiamin absorption [2]. Given that wet beriberi affects the cardiovascular system, there are specific concerns about TD in patients with heart disease, as it may exacerbate their pre-existing cardiac condition.
The prevalence of TD in adult patients with CHF varies from 3% to 91% [7]. However, the prevalence of TD in pediatric patients with CHF has not been thoroughly investigated. A small study by Shamir et al. [8] found that 1 in 12 children (8.3%) with ventricular septal defect (VSD) who underwent furosemide treatment had TD before surgery and 3 in 12 children (25%) had TD 5 days after surgery.
The primary objective of this study was to determine the proportion of TD in pediatric patients with heart disease undergoing diuretic treatment. The secondary objective was to evaluate the factors associated with thiamin status in this group of patients.
Methods
1. Participants and ethical approval
This cross-sectional study was conducted at Siriraj Hospital, Bangkok, Thailand, from December 2019 to April 2024. Children with heart disease aged 1 month to 15 years were recruited from outpatient and inpatient settings if they had increased pulmonary blood flow or CHF and had received diuretics for at least 1 month.
The exclusion criteria included the current use of thiamin or other thiamin-containing vitamins; hemodialysis or peritoneal dialysis; red blood cell disease such as thalassemia, abnormal hemoglobin (Hb) types, and G-6-PD deficiency; conditions with a risk of intestinal malabsorption of thiamin, such as bariatric surgery and small intestinal resection; chronic lung disease; probiotic supplementation with thiamin-producing bacterial strains; heart failure treated with inotropic drugs; and severe anemia with Hb of less than 7 g/dL. The flow chart of participant recruitment was as portrayed in Supplementary Fig. 1.
The study protocol and informed consent were approved by the Siriraj Institutional Review Board of the Faculty of Medicine Siriraj Hospital, Mahidol University (certificate of approval number: Si 364/2019). Written informed assent was obtained from participants aged 7 years or older, and the parents of all participants provided written informed consent.
2. Sample size calculation
In the study by Shamir et al. [8], 8.3% of pediatric VSD patients on diuretics had TD preoperatively and 25% had TD 5 days postoperatively. Based on these findings, we predicted that the prevalence of TD in pediatric patients with heart disease receiving diuretics would be 20%. To determine the proportion of TD in this population with a power of 90% and an alpha error of 0.05, a sample size of 62 participants was required.
3. Participant characteristics and dietary data
After obtaining written informed consent and assent, information on heart disease, diuretic use, as well as frequency and quantity of intake of foods containing antithiamin factors was collected from the participants and their medical records. Anthropometry and signs of TD, such as CHF, aphonic cry, peripheral neuropathy, and absent tendon reflexes, were assessed by 2 pediatric investigators. From the anthropometric data, weight-for-height z score, body mass index (BMI)-for-age z score and height-for-age z score were calculated using WHO Anthro and WHO AnthroPlus software, based on the 2006 WHO Child Growth Standards [9] and the 2007 WHO Growth Reference for 5-19 years of age [10], respectively. Wasting was defined as a weight-for-height z score of <-2 for children 5 years of age or younger, and thinness was defined as a BMI-for-age z score of <-2 for children older than 5 years of age. Stunting was defined as a height-for-age z score of <-2 for children of all ages [11].
To obtain information on daily dietary thiamin intake, participants were asked to complete a 5-day prospective food record. A certified dietitian provided instructions on how to accurately document their food intake. At the end of the procedure, the dietitian verified the accuracy of the food records while blinded to the physical examination findings and the results of the erythrocyte transketolase activity (ETKA) assay. The energy and nutrients data were then analyzed using INMUCAL-Nutrients V.4.0 computer software, based on the Thai food database (Institute of Nutrition, Mahidol University, Thailand). Daily dietary thiamin intake was compared to the recommendations of the Thai dietary reference intake (DRI) [12]. Adequate dietary thiamin intake was defined as meeting or exceeding the age- and sex-specific DRI requirements.
4. Erythrocyte transketolase assay
The thiamin status was assessed by measuring ETKA after the addition of exogenous thiamin pyrophosphate, commonly referred to as the thiamin pyrophosphate effect (TPPE) [13]. The detailed method of the TPPE measurement was described in a previous study by Densupsoontorn et al. [14] The TPPE results were determined using the following formula:
TD was defined as a TPPE of 15% to 24.9%, while severe TD was defined as a TPPE of 25% or greater. The investigators who analyzed the TPPE values were blinded to the findings of the physical examination and dietary data.
5. Cardiac function
The cardiac function of the participants was assessed using left ventricular ejection fraction (LVEF) from echocardiography, with an LVEF of ≥55% indicating normal left ventricular function. The N-terminal pro-brain natriuretic peptide (NT-pro-BNP) was selected as the laboratory assessment for CHF, where an NT-pro-BNP level above the age-specific 95th percentile was considered abnormal.
6. Statistical analysis
Continuous data with a normal distribution were expressed as mean±standard deviation, while those without a normal distribution were expressed as medians (interquartile range [IQR]). Categorical data were presented as counts and percentages. The proportion of TD in pediatric patients with heart disease undergoing diuretic treatment was expressed as a percentage. The association between 2 categorical data was analyzed using a chi-square test. The Mann-Whitney U test was used to compare the ages of participants who consumed and did not consume thiamin-fortified milk/formula, as the data were not normally distributed. The associations between the various factors and the TPPE values were determined by linear regression analyses. Initially, a simple linear regression of TPPE values on various factors, which included age, BMI-for-age z score, height-for-age z score, dosages and durations of furosemide and spironolactone, adequate dietary thiamin intake, number of food groups containing antithiamin factors consumed, intake of thiamin-fortified milk/formula, and postoperative status, was performed. Subsequently, factors with a P value <0.2 were selected for inclusion in multiple linear regression analysis, which was executed via a stepwise procedure. Multicollinearity among independent variables was assessed, with a collinearity tolerance threshold of less than 0.1 and a variance inflation factor of greater than 10. The analyses were performed using IBM SPSS Statistics software (ver. 26.0 and 29.0, IBM Corp., USA), with the significance level set at the P value <0.05.
Results
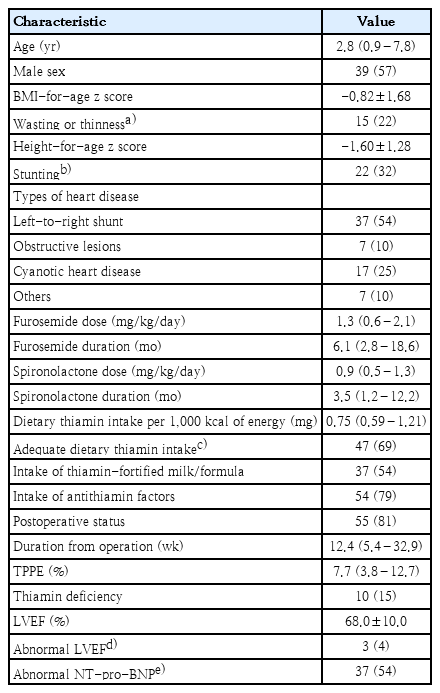
The characteristics of the 68 participants are presented in Table 1. The median (IQR) age of the participants was 2.8 (0.9–7.8) years. More than half of the participants (54%) had a left-to-right shunt heart defect. Most of the participants (63 of 68) received both furosemide and spironolactone, while only 5 participants received furosemide alone. Ten out of 68 participants (15%) had TD, as indicated by a TPPE of 15% or greater. Only 2 patients had TPPE of 25% or greater, suggesting severe TD. However, TD was not significantly associated with abnormally low LVEF (P=0.301) or abnormally high NT-pro-BNP (P=0.322). Furthermore, TD was not associated with aggravation of CHF (P=0.335). Other symptoms suggestive of TD, such as aphonic cry, peripheral neuropathy, and absent tendon reflex, were not present in any of the participants.
Forty-seven of the 68 participants (69%) had adequate dietary thiamin intake according to the Thai DRI [12]. Fifty-four percent of the participants consumed thiamin-fortified milk/formula. Participants who consumed thiamin-fortified milk/formula were younger compared to those who did not, with median (IQR) ages of 1.9 (0.7–5.3) years versus 7.7 (3.3–11.9) years, respectively (P=0.002). Furthermore, 79% of the participants consumed foods with antithiamin factors, including raw fish and shellfish, tea and coffee beverages, and certain vegetables.
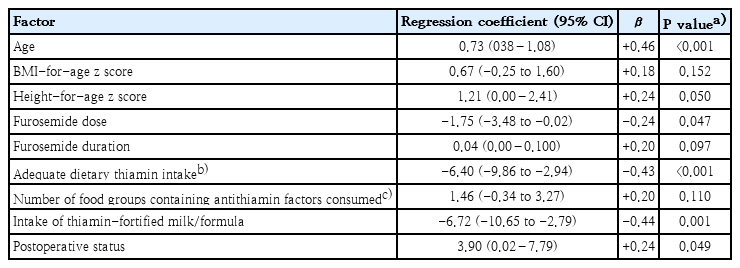
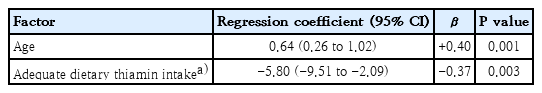
The simple linear regression analysis of the association between TPPE and various factors is presented in Table 2. Factors with a P value <0.2 in simple linear regression, which included age, BMI-for-age z score, height-for-age z score, dosage and duration of furosemide, adequate dietary thiamin intake, intake of thiamin-fortified milk/formula, number of food groups containing antithiamin factors consumed, and postoperative status, were considered potential factors and were selected for inclusion in the multiple linear regression analysis. Ultimately, age (β=+0.40, P=0.001) and adequate dietary thiamin intake (β=-0.37, P=0.003) were found to have significant independent associations with TPPE values, as presented in Table 3.
Discussion
Fifteen percent of pediatric patients with heart disease undergoing diuretic treatment had TD. However, none of the thiamin-deficient participants exhibited overt TD symptoms or exacerbation of CHF. While adequate dietary thiamin intake was associated with a better thiamin status, as indicated by lower TPPE values, it was found that increasing age was associated with a poorer thiamin status.
To date, no studies have determined the prevalence of TD in pediatric patients with heart disease undergoing diuretic treatment. Shamir et al. [8] found that among 12 patients with VSD receiving furosemide, 8.3% had TD before surgery and 25% had TD 5 days after surgery, using a TPPE cutoff of ≥12%. In contrast, our study defined TD at TPPE ≥15%.
Some references stated that a TPPE of 15% to 24.9% indicated marginal deficiency, whilst a TPPE of ≥25% indicated TD [15,16]. As described in the results section, 10 out of 68 participants had TPPE ≥15%, but only 2 of them had TPPE ≥25%. This suggests that our participants may have subclinical TD. Consequently, clinical signs of severe TD, such as aphonic cry, peripheral neuropathy, and absent tendon reflex, were not observed in any of the participants.
Several factors may influence the clinical severity of CHF, including the underlying heart disease, dosage of diuretics, fluid and salt intake, and thiamin status. Our study showed that TPPE values did not correlate with LVEF and NT-pro-BNP levels, which may explain why TD was not associated with the aggravation of CHF in our participants. The worsening of CHF in our participants may have been influenced by other factors, as noted above.
The correlation of beriberi and laboratory thiamin status has never been studied. Additionally, laboratory assessments of thiamin status are not routinely available in many hospitals. There have been several trials on thiamin supplementation in adults with CHF. Two trials found that oral thiamin supplementation led to a significant improvement in LVEF [17,18]; however, neither study evaluated the clinical manifestations of CHF. In 2007, Smithline [19] conducted a study in adults with acute decompensated heart failure, randomly assigning participants to receive either 100 mg of intravenous thiamin or normal saline within 30 minutes of arrival at the emergency department. No significant differences in hospital admission rates, total in-hospital length of stay, and changes in dyspnea severity within 4 hours of enrollment were observed between the thiamin group and control group. Subsequently, in 2019, Smithline et al. [20] performed a randomized controlled trial in adults with CHF with diagnosis of acute heart failure. Patients were randomized to receive either 100 mg of intravenous thiamin daily for 2 days or placebo. Similarly, no significant improvements in dyspnea severity and NT-pro-BNP levels were observed between thiamin group compared to placebo group. From the literature review, better thiamin status may improve LVEF in adult patients but not appear to affect the clinical manifestations of CHF. Furthermore, none of the cited studies investigated the neurological symptoms associated with TD.
Both our study and the study of Shamir et al. [8] reported that markers of malnutrition and furosemide dosage were not associated with TD. Notably, 75% of the patients with TD in the study of Shamir et al. [8] had adequate dietary thiamin intake, which contradicts our findings, as we observed that adequate dietary thiamin intake was associated with better thiamin status.
In adults with CHF receiving diuretic treatment, the prevalence of TD has been reported to range from 3% to 91%. Specifically, prevalence in ambulatory settings ranged from 3% to 27%, while in a hospital setting it varies from 5% to 91% [7]. Moreover, the prevalence of TD, defined by a TPPE of 15% or greater, was significantly higher in CHF patients compared to non-CHF control subjects (odds ratio, 2.43; 95% confidence interval, 1.31−4.54; I2=85%; P=0.0002) [7]. Diuretic use has been associated with increased urinary thiamin loss [5,6], and Zenuk et al. [21] found that adult CHF patients receiving at least 80 mg/day of furosemide had more severe TD than those taking lower doses. However, similar to our present study, Hanninen et al. [22] observed no significant association between TD and the use of furosemide, the dose of furosemide, or the use of multiple diuretics in adult CHF patients. Interestingly, urine thiamin excretion was negatively correlated with TD. A possible explanation is that multiple factors may influence urine thiamin excretion. In addition to diuretic use [5,6], urine thiamin excretion is positively associated with dietary thiamin intake and blood thiamin levels [23-25].
Regarding the prevalence of TD in Thailand, Khampitak et al. [26] found that the prevalence of TD in rural Thai children ranged from 16.8% to 25.4%. In particular, 45.3% of the participants had parasitic infections, but the prevalence of TD did not improve after parasitic treatment. However, data on dietary thiamin intake and the intake of antithiamin factors were not available; therefore, the cause of TD in the study by Khampitak et al. [26] could not be determined. Additionally, it was difficult to compare the results from the study by Khampitak et al. [26] with the findings of this study because the subjects in the 2 studies were from different environmental settings, and the period of investigation were about 15 years apart.
In our study, it is fortunate that none of the patients with TD experienced worsening of CHF or other symptoms related to TD. However, the relatively high proportion of TD in pediatric patients with heart disease undergoing diuretic treatment underscores the importance of TPPE assessment in this population, especially those who have inadequate dietary thiamin intake to detect subclinical TD and allow timely treatment. Furthermore, the clinical implications should emphasize dietary counseling to ensure adequate dietary thiamin intake, with particular consideration given to incorporating thiamin-fortified milk or formula into the dietary plan.
A notable strength of this study is that it is the first to investigate the proportion of TD in a relatively large cohort of pediatric patients with heart disease undergoing diuretic treatment, whereas a previous study had a much smaller sample size of only 12 participants. Additionally, various factors that may contribute to the development of TD were considered in the analysis, including malnutrition status, dietary data, and diuretic use. The TPPE values in this study provided objective data that could not be biased. Furthermore, dietary data did not depend on the recall of participants. We also minimized bias by ensuring that data collectors were blinded.
The limitation of this study included the difficulty of evaluating neurological symptoms and signs of TD in young children, such as numbness or some abnormal sensory test. Furthermore, based on available data, it could not be determined whether this group of patients has a higher risk of TD compared to healthy children or those who do not receive diuretics. Therefore, future research should investigate the prevalence of TD and associated factors among healthy children.
In conclusion, TD was present in 15% of pediatric patients with heart disease undergoing diuretic treatment. Adequate dietary thiamin intake appeared to have a protective effect against TD, as indicated by lower TPPE values, while increasing age was associated with a poorer thiamin status. Assessment for ETKA assay in patients with inadequate dietary thiamin intake may help identify subclinical TD, allowing for timely treatment to prevent severe clinical manifestations.
Supplementary materials
Supplementary Fig. 1 is available at https://doi.org/10.3345/cep.2024.01893.
Research flow chart. FFQ, food frequency questionnaire; NT-pro-BNP, N-terminal pro-brain natriuretic peptide; TD, thiamin deficiency; TPPE, thiamin pyrophosphate effect.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study was supported by the Siriraj Research Development Fund [Grant number (IO) R016233026] and The Royal College of Pediatricians of Thailand.
Acknowledgments
The authors gratefully acknowledge all participants and caregivers for their contributions to this study, as well as Asst. Prof. Dr. Chulaluk Komoltri of the Department of Clinical Epidemiology, Faculty of Medicine Siriraj Hospital, for her assistance with the statistical analyzes.
Author Contribution
Conceptualization: PL, RS, CV, PS, CS, ND; Investigation: RS, KC, SJ, SK, HR, PP, SL; Data curation: PL, RS, AP; Formal analysis: PL, PS; Funding acquisition: ND; Methodology: PL, RS, CV, PS, CS, ND; Project administration: RS, ND; Visualization: PL; Writing-original draft: PL; Writing - review & editing: PS, ND