Association between polycystic ovary syndrome and risk of attention-deficit/hyperactivity disorder in offspring: a meta-analysis
Article information
Abstract
Background
There is evidence of a relationship between prenatal excess androgen exposure and central nervous developmental problems and attention-deficit/hyperactivity disorder (ADHD) in the offspring of mothers with polycystic ovary syndrome (PCOS).
Purpose
Here we aimed to use a meta-analysis to investigate whether the offspring of mothers with PCOS are at an increased chance of developing ADHD.
Methods
Three main English databases were searched for articles published through December 2020. The NewcastleOttawa Scale was used to assess study quality. Study heterogeneity was determined using I2 statistics and publication bias was assessed using Begg and Egger tests. The results are presented as odds ratio (OR) and relative ratio (RR) estimates with 95% confidence intervals (CIs) using a random-effects model.
Results
Six articles (3 cohort and 3 case-control studies; 401,413 total ADHD cases) met the study criteria. Maternal PCOS was associated with an increased risk of ADHD in the offspring based on OR and RR (OR, 1.42; 95% CI, 1.27–1.57) and (RR, 1.43; 95% CI, 1.35–1.51), respectively. There was no heterogeneity among the included articles based on OR (I2=0.0%, P=0.588) and RR (I2=0.0%, P=0.878).
Conclusion
Our study showed that maternal PCOS is a risk factor for ADHD. Therefore, screening their offspring for ADHD should be considered part of the comprehensive clinical care of women with PCOS.
Key message
Question: Have polycystic ovary syndrome (PCOS) increased risk of having an offspring with attention-deficit/hyperactivity disorder (ADHD)?
Finding: Six articles (3 cohort and 3 case-control studies; 401,413 total ADHD cases) met the study criteria. Maternal PCOS was associated with an increased risk of ADHD in the offspring based on odds ratio (OR) and relative ratio (RR) (OR, 1.42; 95% confidence interval [CI], 1.27–1.57) and (RR, 1.43; 95% CI, 1.35–1.51), respectively.
Meaning: Our study showed that maternal PCOS is a risk factor for ADHD.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a childhood mood disorders though some symptoms often continue to adulthood [1]. It is characterized by pervasive symptoms of attention-deficit/hyperactivity according to Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) [2]. ADHD categorized in 3 types inattentive, hyperactive-impulsive, or both inattention and hyperactive-impulsive symptoms [3]. The prevalence of ADHD is varied in worldwide. According to the meta-analysis overall prevalence of ADHD was 7.2% [4]. The etiology of ADHD is not fully understood but many environmental, genetic, and environment-gene interactions factors can lead to the development of ADHD [5]. In terms of frequency, ADHD is more common in boys than girls [6]. These observations suggest that early intrauterine exposure of the fetus to a high level of androgen and sex hormone are probably associated with hyperactivity by affecting brain development [7].
One of the sources of excess androgen exposure of mother is polycystic ovary syndrome (PCOS). Other common finding in women with PCOS are chorionic anovulation, subinfertility, and metabolic syndrome [8]. According to a prospective cohort study, the risk of failing the Ages and Stages Questionnaire among children who born to women reported PCOS treatment was more than the offspring of women who reported receiving no treatment for PCOS [9]. The association between maternal PCOS with ADHD, autism spectrum disorders (ASDs), and ADHD comorbid with ASD have been reported in some studies may suggest evidence on offspring behavioral and developmental disorders [10,11]. The evidence of meta-analyses emphasizes that the odds of ASD in the offspring women with PCOS have increased 1.66 times [12] but the association between polycystic ovary syndrome and the risk of ADHD among their offspring has not been systematically reviewed. Therefore, we conducted the first review and meta-analysis to assess whether women with PCOS have increased risk of having an offspring with ADHD.
Methods
The aim of this review was to determine whether a mother with PCOS has increased chance of ADHD in her offspring. The review is reported based on the PRISMA checklist [13].
1. Search strategy and data sources
The English electronic databases included the Web of Science, PubMed, and Scopus were systematically searched for studies published to December 2020 with restricted English language using the following search strategies in accordance with the MeSH browser keywords and free-text words: [((((("polycystic ovary syndrome"[Title/Abstract]) OR ("Stein-Leventhal Syndrome"[Title/Abstract])) OR ("Sclerocystic Ovary"[Title/Abstract])) OR ("Ovarian Syndrome"[Title/Abstract])) OR ("Polycystic Ovary Syndrome 1"[Title/Abstract]) AND ((((("Attention Deficit Hyperactivity Disorders"[Title/Abstract]) OR ("Hyperkinetic Syndrome"[Title/Abstract])) OR (ADDH*[Title/Abstract])) OR (ADDH[Title/Abstract])) OR ("Minimal Brain Dysfunction" [Title/Abstract])) OR ("Attention Deficit Disorders"[Title/Abstract]) AND "Case-control study "[Title/Abstract]) AND "Cohort study" [Title/Abstract])]. In addition, the list reference of selected articles was checked and contacted the authors if required to obtain full texts of study.
2. Inclusion criteria and exclusion criteria
All case-control and cohort (both prospective and retrospective) studies that provided data on the rate of ADDH among the offspring of women with PCOS were included the review.
The PCOS criteria in mother are defined by Rotterdam, National Institute of Health and the accepted clinical criteria International Classification of Diseases (ICD)-8, ICD-9/ICD-10, and self-reported. Rotterdam criteria are defined by 2 of the following 3 features: (1) oligo or anovulation, (2) clinical and/or biochemical signs of hyperandrogenism, or (3) polycystic ovaries [14]. The ADHD criteria are defined by the accepted clinical criteria DSM-IV, ICD-9, and ICD-10. ADHD criteria are defined 5 or more symptoms of inattention and/or ≥5 symptoms of hyperactivity/impulsivity must have persisted for ≥6 months to a degree that is inconsistent with the developmental level and negatively impacts social and academic/occupational activities [15].
All experimental in vivo/in vitro study, cross-sectional, review, and case report/series studies were excluded.
3. Study selection
Two authors (EJ and AM) independently searched, and screened duplicates, the titles, and abstracts the studies. The information of full texts extracted using a structured form included author name, year, design, sample size, estimate, adjustment, maternal age rang (year)/mean, ADHD criteria, and study quality. Disagreements of the extractors were resolved by discussion with a third person.
The Newcastle-Ottawa Scale (NOS) for cohort and case-control studies have been used to the evaluation of quality in individual studies [16]. The NOS includes 8 items. Each item gets a score when it will be appropriate criteria. Therefore, a maximum score considered high quality.
4. Synthesis of results
STATA 16 (StataCorp LP., College Station, TX, USA) was used for analyses. The heterogeneity of the studies was assessed using I2. The I2 equal or lower than 50% considered adequate heterogeneity. In this study, random effect model was applied due to true effect size. We presented results using odds ratio (OR) and relative ratio (RR) estimates with its 95% confidence intervals (CI) using a random-effects model. Publication bias was assessed using the funnel plot and Egger and Begg tests [17].
Results
1. Description of studies
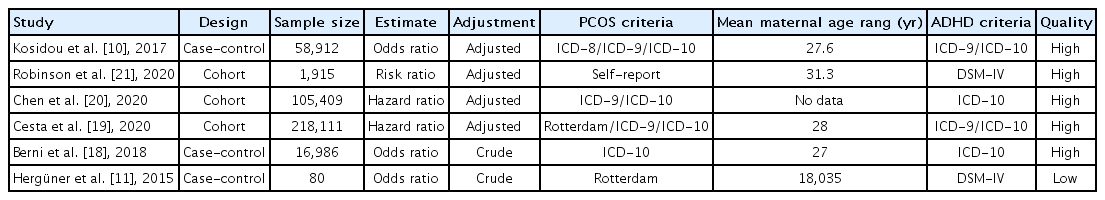
We identified 236 articles by search in 3 major databases and other sources. Among these, 69 duplicate articles and 155 unrelated articles were removed. Then, 12 articles were remained for review of the full paper. After review, 6 articles were excluded due to 5 review articles and 1 article with similar data to another article. In total, 6 articles (3 cohort studies and 3 case-control studies) were included in the present meta-analysis [10,11,18-21]. Fig. 1 presents the process of the included articles.
Preterm labor, maternal and paternal age, birth order, household income, mother's country of birth, small for gestational age, and preeclampsia were the confounding variables of the association between PCOS and the risk of ADHD among offspring.
2. Main analysis
Fig. 2 presents the association between PCOS and the risk of ADHD among the included studies. The pool estimates of the present meta-analysis reported that PCO in maternal was associated with the risk of ADHD among offspring based on OR and RR (OR, 1.42; 95% CI, 1.27–1.57) and (RR, 1.43; 95% CI, 1.35–1.51), respectively. There was not heterogeneity among included articles based on OR (I2=0.0%, P=0.588) and RR (I2=0.0%, P=0.878).
Forest plot of the association between polycystic ovary syndrome and the risk of attention-deficit/hyperactivity disorder. OR, odds ratio; RR, relative ratio.
The publication bias did not find among studies based on Begg and Egger tests. The P values for Egger and Begg tests were P=0.133 and P=0.188, respectively.
3. Quality of the studies
The quality of the studies based on the NOS Scale was presented in Table 1. The quality of the studies in the present meta-analysis was categorized into 5 studies with high quality and 1 study with low quality. Fig. 3 shows review authors' judgments about each risk of bias item for each included study.
Discussion
To our knowledge, this is the first systematic review to assess the risk of ADHD in the children of women with PCOS compared to control group. Overall, based on the available evidence, the meta-analysis showed that the PCOS in maternal was associated with increasing the risk of ADHD among her offspring. There was between-study homogeneity in the present meta-analysis.
However, in a meta-analysis of 10 studies has been reported evidence that chance of having ASD significantly increased in offspring of women with PCOS [12]. Although, brain structure of ADHD and ASD have distinct neural features in gray and white matter structures, the majority of ASD symptoms commonly cooccur with ADHD symptoms but the minority of individuals with ADHD demonstrates ASD symptoms [22].
PCOS may expose the developing fetus to excess androgens because women with PCOS increase circulating androgen levels during pregnancy and have more placental androgen capacity. Brain development is influenced significantly by exposure to androgens during early gestation [23]. Prenatal androgen exposure may increase the risk of ASD and ADHD by affecting dendritic morphology, nerve density, abnormal synapse function, and morphology. Also, PCOS in mother is associated with more circulating androgens and inflammatory cytokines, which may affect fetal brain development [24].
Robinson et al. [21] showed that one-third of women with PCOS had hirsutism. The hirsutism in maternal was association with ADHD among offspring, conduct disorder, peer relationship problems, prosocial problems, and emotional symptoms.
Some reasonable mechanism underlying the potential association between maternal PCOS and ADHD. Poor pregnancy outcome has been reported in women with PCOS such as abortion, preeclampsia, gestational diabetes mellitus (GDM), small/large for gestational age infants, cesarean delivery, and preterm delivery [25]. It is known that the risk of ADHD increases among offspring whose mothers had obesity, preeclampsia and GDM [26-28]. Obesity, infertility, and the use of fertility treatment more experienced by women with PCOS might be influenced offspring [29,30]. Women with PCOS are known to have a higher risk of developing depression and adult ADHD. This risk, in turn, might cause an increase in psychiatric morbidity in their children [18].
Our study has some limitations. Although, most of the studies in present meta-analysis were adjusted for some risk factors of ADHD. However, 2 studies reported crude form for ADHD. In addition, there was limit studies about the association between of PCOS and the risk of ADHD that has been done so far. Therefore, these limitations may increase the possibility of bias that should be determined when interpreting these findings. However, our study with 401,413 participants showed that PCOS is a risk factor for ADHD among offspring.
Our study showed that maternal PCOS is a risk factor for ADHD. Therefore, Screening for ADHD among children of these women should be considered as part of the comprehensive clinical care for women with PCOS.
Notes
Conflicts of interest
The authors have no conflict of interest to declare.
Acknowledgements
This study was funded by Hamadan University of Medical Sciences with code 9911218343.
We thank from Hamadan University of Medical Sciences for their support.