Maternal food restrictions during breastfeeding
Article information
Abstract
Purpose
This study investigated self-food restriction during breastfeeding, reviewed the literature showing the effect of maternal diet on the health of breast-fed infants, and explored the validity of dietary restrictions.
Methods
Questionnaire data were collected from breastfeeding Korean mothers who visited the pediatric clinic of Cheil General Hospital & Women's Healthcare Center from July 2015 through August 2015. The survey included items assessing maternal age, number of children, maternal educational attainment, household income, degree of difficulty with self-food restriction, types of self-restricted foods, dietary customs during breastfeeding, and sources of information about breastfeeding.
Results
The questionnaire was completed by 145 mothers. More than a third (n=56, 39%) had discomfort from and usually avoided 4–5 types of food (mean, 4.92). Mothers younger than 40 years had more discomfort (odds ratio [OR], 12.762; P=0.017). Primiparas felt less discomfort than multiparas (OR, 0.436; P=0.036). Dietary practices were not influenced by maternal educational attainment or household income. The most common self-restricted foods were caffeine (n=131, 90.3%), spicy foods (n=124, 85.5%), raw foods (n=109, 75.2%), cold foods (n=100, 69%), and sikhye (traditional sweet Korean rice beverage) (n=100, 69%). Most mothers (n=122, 84.1%) avoided foods for vague reasons.
Conclusion
Most mothers restricted certain foods unnecessarily. Literature review identified no foods that mothers should absolutely avoid during breastfeeding unless the infant reacts negatively to the food.
Introduction
Exclusive breastfeeding for 6 months after birth has many benefits for the infant and mother1). Breast milk is also an important source of energy and nutrients in children aged 6 to 23 months. However, there are many obstacles that can disrupt breastfeeding, despite its merits. The major reasons for breastfeeding failure are insufficient amount of milk, return to work, maternal diseases, and baby's diseases in Korea234). Cultural tradition also affects the lactation behavior56). Without a scientific basis, popular myths about maternal diet during breastfeeding can become barriers to breastfeeding and lead to unnecessary dietary restrictions in breastfeeding mothers. Most cultures have some proscriptions during lactation7). For example, many Asian women are advised to avoid cold foods because they are not good for the mother and baby8). Hispanic women may be told not to eat pork, chili, and tomato. In Korea, mothers are cautioned to avoid spicy foods, such as Kimchi because they could cause colic, gas, diaper rashes in the breastfeeding infants. These self-restrictions differ from food insecurity owing to circumstances beyond control, such as poverty9). Lawrence and Lawrence10) explained these cultural dietary rules during breastfeeding: “Most material for nursing mothers regarding maternal diet during lactation set up complicated ‘rules’ about dietary intake that fail to consider the mother's dietary stores and normal dietary preferences and cultural patterns. Thus one barrier to breastfeeding for some women is the ‘diet rules’ they see as being too hard to follow or too restrictive.”
The maternal body prepares during pregnancy for breastfeeding not only by developing the breast, but also by storing additional nutrients and energy for breast milk production. Before and after delivery, mothers usually perceive an increase in appetite and thirst and a change in some dietary preferences. A restricted diet could reduce the quality of life of a breastfeeding mother and discourage her from continuing exclusive breastfeeding. One survey found that some mothers chose not to breastfeed for this reason and demonstrated that many women believe that the food they eat can directly affect the breast milk they produce6). In addition, mothers are often given ambivalent recommendations. For example, mothers might be encouraged to drink cow's milk in order to increase breast milk production, while others discourage cow's milk consumption in order to prevent milk allergy in breastfeeding infants.
Contrary to popular belief, if the mother has healthy eating habits, there is usually no reason to change them during breastfeeding. Although there are some nutritional guidelines for breastfeeding women11), evidence-based recommendation about food restriction during breastfeeding is still limited. In addition, there was lack of study about maternal food restriction or cultural proscriptions during breastfeeding in Korea. We sought to investigate maternal self-restricted diet practices during breastfeeding and sought any studies showing the effect of maternal diet on the health of breast-fed babies in order to explore the validity of dietary restrictions.
Materials and Methods
Questionnaire data were collected from mothers who visited pediatric outpatient clinic of Cheil General Hospital & Women's Healthcare Center from July 2015 through August 2015. Mothers were included in this study (1) who had an experience of breastfeeding (exclusive or partial breastfeeding), and (2) had neonates from 1-week- to 1-month-old age. Non-Korean mothers who could not understand Korean were excluded.
The survey included items assessing maternal age, number of children, maternal educational attainment, household income, degree of difficulty with a restricted diet, types of self-restricted foods, foods believed by mothers to be helpful for breastfeeding, recommended foods for breastfeeding, and sources of information about breastfeeding (Supplementary material 1). The degree of difficulty related to self-food restrictions was categorized as four levels according by ease of maintenance: (1) very difficult, (2) difficult, (3) bearable, and (4) easy. The measured degree of difficulty were dichotomized into discomfort (“very difficult” and “difficult”) and tolerable (“bearable” and “easy”). Food types are selected from frequently asked questions of breastfeeding mothers and previous studies1213). Self-restricted foods were classified into 14 categories: caffeine, spicy foods such as kimchi, milk products, wheat, fatty foods, cold foods, beans, nuts, fish/sea food, raw foods such as raw fish, sikhye (traditional sweet Korean rice beverage), pumpkin, specific fruits such as peaches, and specific vegetables such as cabbage. Comprehensive literature review was done to explore the association between self-restricted foods and breast milk. To compare simple proportions, chi-square tests (or Fisher exact test, when appropriate) were used. P values less than 0.05 were considered statistically significant. Logistic regression models were used to determine which factors were associated with the difficulty related to self-food restrictions. Results are reported as odds ratio (OR) and 95% confidence interval (CI). All statistical analyses were conducted using SPSS ver. 12 (SPSS Inc., Chicago, IL, USA). This study was conducted with approval by the Institutional Review Board of Cheil General Hospital & Women's Healthcare Center (approval number: CGH-IRB-2015-35).
Results
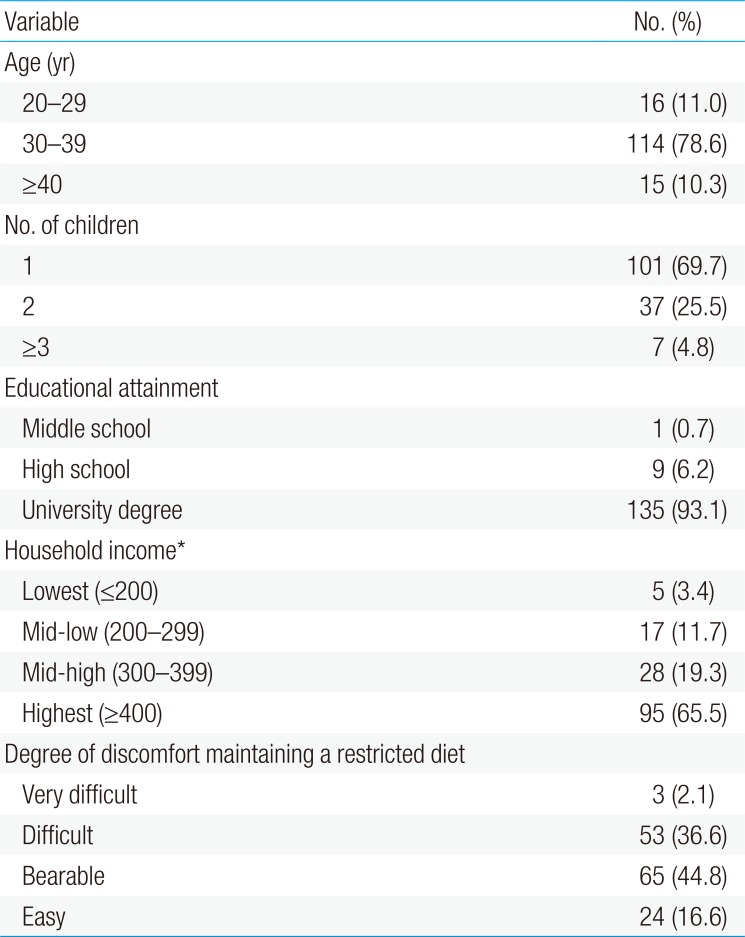
1. Characteristics of mothers
During the study period, 432 neonates visited the hospital, and 32 neonates were twin. Among 369 breastfeeding mothers, 165 mothers responded to the survey and 145 mothers were completed the questionnaire. The demographic characteristics of breastfeeding mothers are included in Table 1. Fifty-six mothers (38.6%) experienced difficulties related to self-food restrictions. All mothers avoided one or more types of food during breastfeeding and usually avoided 4–5 types of foods (mean, 4.92).
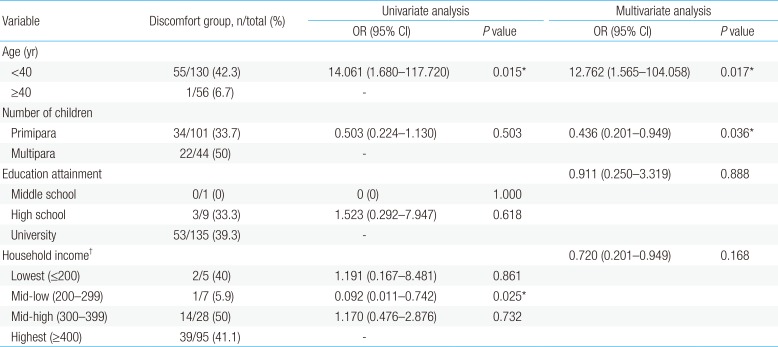
Table 2 lists the maternal risk factors associated with the discomfort with self-food restrictions during breastfeeding. Maternal age affected the discomfort. The younger mothers were, the more the discomfort increased (P=0.027). The discomfort was highest (43.8%) in 20s, followed by 42.1% in 30s and 6.7% in 40s. Mothers younger than 40 years felt more discomfort than mothers older than 40 years old (OR, 12.762; P=0.017). The experience of bringing up a child did not decrease the discomfort. Contrary to expectation, primiparas felt less discomfort than multiparas (OR, 0.436; P=0.036). The degree of difficulty varied by household income. Mothers lived in mid-low household income were the most tolerable to self-food restrictions (5.9%) but the difference was not statistically significant (P=0.168). Maternal educational attainment did not affect the discomfort (P=0.888).
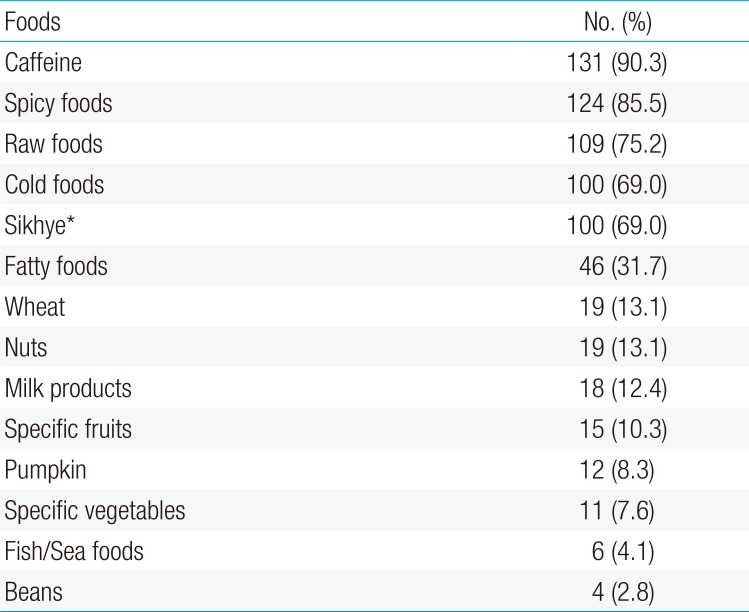
2. Types of restricted foods during breastfeeding
Commonly restricted foods were caffeine (n=131, 90.3%), spicy foods (n=124, 85.5%), raw foods (n=109, 75.2%), cold foods (n=100, 69%), and sikhye (n=100, 69%) (Table 3). The reasons given for restriction were that sikhye could decrease breast milk production (n=10); peach or kiwi could cause allergies (n=4); spicy foods could cause colic or skin rash (n=2); eating raw foods makes one susceptible to food poisoning or parasite infection (n=2); elimination of cow's milk could prevent development of milk allergy (n=1); cold foods could cause diarrhea (n=1); broccoli could cause colic and gas (n=1); pumpkin could decrease breast milk production (n=1); and fatty foods could decrease milk production because they can obstruct the mammary ducts (n=1). Most mothers (n=122, 84.1%) avoided a specific type of food without a specific reason or because of a vague concern that it could be harmful to her infant.
There was no statistically significant food type associated with the discomfort, maternal age, number of children, maternal educational attainment, nor household income. Also the discomfort was not proportional to the number of restricted foods. The number of restricted foods had no relationship with the discomfort (P=0.635).
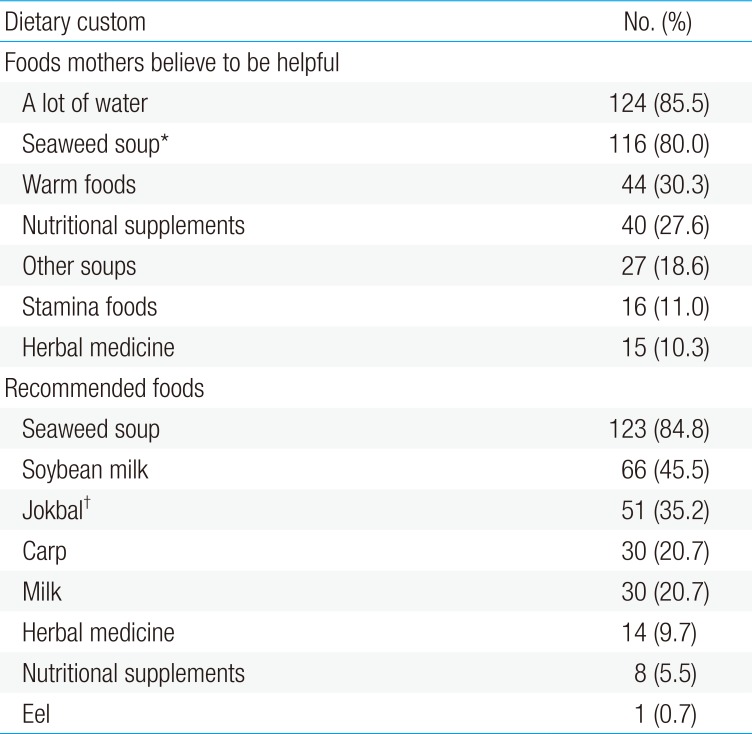
3. Dietary custom during breastfeeding
Table 4 demonstrates the cultural dietary practices around breastfeeding found in the present study. Most mothers believed that drinking a lot of water would increase breast milk yield (n=124, 85.5%). Seaweed soup, which is called “miyeokguk” in Korean (n=116, 80%), and other soups (n=27, 18.6%) were also considered helpful for breastfeeding. Other practices believed to be beneficial for breastfeeding included eating warm foods (n=44, 30.3%), nutritional supplements (n=40, 27.6%), stamina foods (n=16, 11%), and herbal medicine (n=15, 10.3%). The most commonly recommended foods for breastfeeding were seaweed soup (n=123, 84.8%); soy milk (n=66, 45.5%); jokbal, which is a Korean dish consisting of pig trotters cooked with soy sauce and spices (n=51, 35.2%); carp (n=30, 20.7%); milk (n=30, 20.7%); herbal medicine (n=14, 9.7%); nutritional supplements (n=8, 5.5%); and eel (n=1, 0.7%).
4. Information source regarding breastfeeding
Breastfeeding mothers usually received information about breastfeeding from family members (n=75, 51.7%) or friends (n=75, 51.7%). Other sources included the media (including the internet) (n=69, 47.6%), postnatal care centers (n=64, 44.1%), books (n=44, 30.3%), medical professionals (n=43, 20.7%), and postnatal caretakers (n=17, 11.7%). Medical professionals were the source of information to only a small proportion of mothers and were a less common source of information than postnatal care centers.
Discussion
More than a third of breastfeeding mothers surveyed reported the discomfort due to the self-food restriction of certain foods. Mothers younger than 40 years old age felt more discomfort about self-food restrictions. The experience of childbearing did not decrease the discomfort. Rather mothers with 2 or more children had more difficulty to sustain self-food restrictions. The most commonly restricted foods were caffeine, spicy foods, raw foods, and sikhye. Most breastfeeding mothers received information about breastfeeding from nonmedical professionals, and there was usually no scientific reason for dietary restrictions. In light of this, we reviewed previous studies and suggested the following dietary recommendations for breastfeeding.
Common sources of caffeine are coffee, tea, and soft drinks. Although caffeine is transferred to breast milk, the amount of caffeine transferred to breast milk is generally less than 1% of the amount consumed by the mother13), and modest caffeine use does not negatively affect infants14). Because no caffeine has been detected in an infant's urine with maternal consumption of up to three cups of coffee a day, it is unlikely that infants experience measurable exposure to caffeine. However, if a mother consumes more caffeine in one day than is found in 5 cups of coffee (750 mL), caffeine could begin accumulating in an infant's system, causing symptoms of caffeine stimulation12). Theobromine in chocolate is similar to caffeine, although there is much less theobromine in chocolate than there is caffeine in coffee. Typical intake of chocolate does not significantly increase the level of either theobromine or caffeine in infant15).
Many mothers are told to avoid spicy foods because these foods are thought to cause colic, gas, diarrhea, and rashes in the breastfeeding infant. However, although strong flavors such as garlic can change the smell and flavor of breast milk, this does not usually make infants fussier. Two studies have shown that the infants of mothers who eat garlic extract tend to feed for a longer time and seem to prefer a variety of flavors in breast milk, which might facilitate weaning to solid foods16). Infants rarely react to a food that mothers eat, and the few foods that have been observed to cause reactions differed among infants, so it is not reasonable to recommend that all breastfeeding mothers avoid certain foods.
In addition, it is common for mothers to be warned to avoid “gassy foods” such as cabbage, cauliflower, and broccoli. Eating such foods can cause gas in the mother's bowel; however, gas and fiber do not pass into breast milk. Similarly, acidic foods like citrus fruits, pineapple, and tomatoes do not affect breast milk, as these foods do not change the pH of maternal plasma10).
Common raw foods include raw fish (sashimi), oysters, unpasteurized milk, and Yukhoe (traditional Korean steak tartare). Any raw food can be a source of infection, and some species of fish contain a significant amount of mercury. Consumption of raw foods by nursing mothers does not pose a serious problem for breastfeeding infants, although there is the potential for the mother to suffer from food poisoning. In general, maternal food poisoning does not result in infection in infants except in rare cases of septicemia, where bacteria might reach the breast milk17). Even in severe septicemia, there is no need to discontinue breastfeeding if the mother is treated with appropriate antibiotics.
There is a common belief in many non-Western cultures that women need to maintain a warm temperature within the body and the environment during the postpartum period8). Thus, breastfeeding mothers in these cultures are advised to avoid cold foods. The temperature of breast milk is similar to body temperature and is well maintained through thermoregulation. There have been no reports of cold foods affecting the production or quality of breast milk.
Sikhye is a traditional sweet Korean rice beverage made by pouring malted water over cooked rice. The combination is then fermented for a least one day, boiled, and sometimes flavored with jujube or ginger. Traditionally, sikhye has been thought to decrease breast milk production in Korean. ‘Sikhye,’ ‘fermented rice,’ and ‘malt’ were used as key search terms; however, our extensive literature search through online medical literature including PubMed, Embase, Web of Science, and KoreaMed, which is operated by the Korean Association of Medical Journal Editors, produced no evidence on the relationship between sikhye and breast milk production. Further research is needed on whether sikhye decreases breast milk yield before recommendations can be provided to breastfeeding mothers.
The diet of breastfeeding mothers should include adequate polyunsaturated fatty acids and very low levels (i.e., <1%) of transfatty acids. The amount of fat in breast milk changes during each feeding and throughout the day. Maternal diet can affect the composition of fatty acids, but does not change the total milk fat content101318). Docosahexaenoic acid (DHA) is critically important for visual acuity and neural development. Maternal DHA intake through consumption of fish and seafood increases the level of DHA in breast milk.
In contrast to the benefits of DHA, transfatty acids in breast milk could negatively affect infant growth and development19). A high level of transfatty acids is consistently related to lower levels of DHA. The most common foods containing transfatty acids are bakery items, snacks, fast food products, and margarine. The World Health Organization recommends that transfats be limited to less than 1% of overall energy intake20).
Milk and milk products are important sources of calcium. The Korea Food and Drug Administration recommends that breastfeeding mothers consume 3 or more cups of milk or dairy products every day11). However, breastfeeding mothers do not need to drink extra milk to increase breast milk production.
While milk provides good nutrients, milk consumption is sometimes discouraged due to concerns about cow's milk protein allergy (CMPA). CMPA occurs in both exclusively and partially breast-fed infants, although the incidence of CMPA is lower in exclusively breast-fed infants than formula-fed or mixed-fed infants. Reactions to CMP by exclusively breast-fed infants are rare (0.5%), and adverse reactions are not severe21). If CMPA is suspected, diagnostic elimination of CMP should be initiated for a limited period22). When a maternal elimination diet results in considerable benefit, the mother should be advised to continue avoiding all milk and milk products22). During the elimination diet, mothers should be given sufficient calcium (i.e., 1000 mg/day). In infants who have a strong family history of allergies, exclusive breastfeeding in combination with maternal dietary restrictions may be beneficial. As noted in the Cochrane review, a maternal elimination diet of cow's milk, egg, and other antigens is helpful in some breast-fed infants with atopic eczema. However, at the present time, a maternal elimination diet during breastfeeding has not been proven to prevent any allergic disease in infants except atopic eczema23). The evidence suggesting that an elimination diet during breastfeeding decreases the development of allergies is weak, whereas the potential for maternal malnutrition is concerning. Therefore, the recommendation that all breastfeeding mothers avoid specific foods in order to protect their children from allergic diseases is an unnecessary precaution.
Fish and seafood are rich in protein and omega-3 fatty acids. Fish consumption by breastfeeding mothers has been suggested to be beneficial to infants because of the large amount of essential fatty acids, which are important in brain development. However, most fish and seafood contain mercury and other contaminants. Excessive amounts of mercury passed through breast milk may potentially harm the infant's developing nervous system. Mercury intake can be decreased by avoiding the ingestion of certain large fish (e.g., pike, swordfish, king mackerel, tilefish, and marlin). Considering the potential benefit of essential fatty acids versus the risk of mercury exposure, the American Academy of Pediatrics24) concluded that the “possible risk of excessive mercury or other contaminants is offset by the neurobehavioral benefits of adequate DHA intake.”
In this study, many mothers believed that drinking a lot of fluids was helpful in increasing breast milk production. However, fluid intake during lactation does not affect milk volume13). “Drink to thirst” is the best guide for how much liquid a breastfeeding mother should drink. It is not beneficial for the mother or her milk supply to force extra fluids. One study found that drinking 25 percent more fluid than the “drink to thirst” recommendation actually resulted in a slightly decreased milk supply25).
In conclusion, all mothers in the present study restricted at least one type of food without scientific rationale while breastfeeding and more than a third of nursing mothers experienced difficulties with diet restriction. Nursing mothers should be educated on proper diet practices while being warned about unscientific approaches to diet restriction. In recent systematic review, education and emotional support by healthcare providers could enhance breastfeeding26). We expect this study will give scientific basis for dietary recommendation to breastfeeding mothers and could promote a breastfeeding.
Acknowledgment
The authors wish to thank all the mothers who took part in this study.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
Supplementary Material
Supplementary material can be found via http://kjp.or.kr/upload/kjp-60-70-s001.pdf.
Supplement material 1
Survey questionnaire