A comparison of the efficacy of amoxicillin and nasal irrigation in treatment of acute sinusitis in children
Article information
Abstract
Purpose
The efficacy of antibiotic therapy for acute sinusitis is controversial. This study aimed to compare the efficacies of amoxicillin with nasal irrigation and nasal irrigation alone for acute sinusitis in children.
Methods
This randomized, double-blind, controlled study included 80 children aged 4-15 years with a clinical presentation of acute sinusitis. Patients were randomly assigned to receive either amoxicillin (80 mg/kg/day) in 3 divided doses orally for 14 days with saline nasal irrigation (for 5 days) and 0.25% phenylephrine (for 2 days) or the same treatment without amoxicillin. Clinical improvements in their initial symptoms were assessed on days 3, 14, 21, and 28.
Results
On day 3, patients in the amoxicillin with nasal irrigation group showed significant clinical improvement (P=0.001), but there was no significant difference in the degree of improvement between the amoxicillin with nasal irrigation and nasal irrigation alone groups during follow-up (P>0.05). In addition, no significant differences were seen in age, sex, and degree of improvement between groups (P>0.05).
Conclusion
High-dose amoxicillin with saline nasal irrigation relieved acute sinusitis symptoms faster and more often than saline nasal irrigation alone. However, antibiotic treatment for acute sinusitis confers only a small therapeutic benefit over nasal irrigation.
Introduction
Sinusitis is a common condition in children. Children have average six to eight colds per year with 0.5%-5% developing acute sinus infection1). Sinusitis is a leading reason for outpatient antibiotic use2). In the United States (US), sinusitis affects about 1% of children each year and accounts for more than 1.8 billion US dollar in direct health care expenditures and 20 million prescriptions for antibiotics per year3). Under diagnosis or delayed treatment of acute rhinosinusitis may lead to chronic rhinosinusitis or many complications such as intracranial extension of infection, thrombophlebitis, osteomyelitis or orbital complications4).
The diagnosis of sinusitis should be made based on clinical criteria and imaging is not routinely indicated5). The clinical symptoms of acute rhinosinusitis are nasal blockage or congestion, nasal discharge or postnasal drip (often mucopurulent), facial pain, headache, and reduction or loss of smell6).
Acute sinusitis is common and usually treated with antibiotics in spite of the lack of evidence for the effectiveness of antibiotic therapy and the increasing number of resistant strains. Falagas et al.7), did a meta-analysis of randomized controlled trials (RCTs) to assess the therapeutic role of antibiotics for acute sinusitis compared with placebo. They concluded that the use of antibiotics for acute sinusitis deals with a small therapeutic benefit over placebo.
Canadian clinical practice guidelines for acute and chronic rhinosinusitis recommended that antibiotics may be prescribed for acute bacterial rinosinusitis (ABRS) to improve rates of resolution at 14 days and should be considered where either quality of life or productivity present as issues, or in individuals with severe sinusitis or comorbidities. When antibiotic therapy is selected, amoxicillin is the first-line recommendation in treatment of ABRS. In addition, adjunct therapy should be prescribed in individuals with ABRS. Saline irrigation as an adjunct therapy may provide symptom relief. Saline therapy, either as a spray or high-volume irrigation, has seen widespread use as adjunct treatment despite a limited evidence base8).
Nasal irrigation has been used as an adjunctive therapy of sinonasal disease including acute or chronic sinusitis and allergic rhinitis. Some published articles reported it also improves clinical sinus symptoms9). This method is an inexpensive and patient-controlled therapy that flushes the nasal cavity with saline solution, facilitating washing of the structures within. Benefits from nasal irrigation may occur from removal of nasal discharge and crusts, and mucus thinning10).
High-dose amoxicillin, amoxicillin/clavulanate, or other β-lactam antibiotics should be considered for children at high risk for carrying resistant organisms11) and high-dose amoxicillin is preferred over standard-dose amoxicillin primarily to cover penicillin resistant Streptococcus pneumoniae12). Regarding to Khoshdel et al.13) study, S. pneumonia and its resistance to penicillin was 28.9% in present study area, therefore, high dose amoxicillin was used in this study.
On the other hand, clinical practice guideline for acute bacterial rhinosinusitis in children and adults claims that "there is a net clinical benefit of intranasal physiologic or hypertonic saline irrigation as an adjunct to antimicrobial therapy in both adults and children with acute sinusitis, but the optimal concentration, volume, frequency, and most appropriate technique for nasal saline irrigation remain to be determined"12), so, this study was done with the aim of comparison the effectiveness of high dose amoxicillin with nasal irrigation in management of acute sinusitis in children.
Materials and methods
This study was conducted at the department of pediatrics, Shahrekord Medical University of Sciences, Shahrekord, Iran, between April 2012 and August 2012.
Ethics Board of the Shahrekord Medical University of Sciences made approval for the study protocol. Written informed consent was obtained from the parents of children before entering to the study. Antibiotics should not be prescribed for mild to moderate sinusitis within the first week of the illness14), although in present study, the patients with no clinical improvement during follow up period, treatment incompliance, or relapse of symptoms were excluded and the pediatrician prescribed antibiotic or changed their previous antibiotic regimen. In addition, the patients with severe symptoms or complicated sinusitis did not included in study, therefore, there was not any ethical prohibition.
Sample size was calculated by PS2 (Power and Sample Size Calculation) 35 patients, but 100 children between the age 4 to 15 years with a clinical presentation of acute sinusitis were participated in this study. A pediatrician visited all patients and carried out sinusitis diagnosis.
A number was given to each patient, then according to their odd or even numbers, they were randomly assigned in two groups; intervention group (n=50) with odd numbers received amoxicillin (80 mg/kg/day) in three divided doses by mouth for 14 days with nasal 0.9% saline irrigation (for five days) and nasal 0.25% phenylepherin (for two days). Patients in nasal irrigation group (n=50) with even numbers received nasal 0.9% saline irrigation (for five days) and nasal 0.25% phenylepherin (for two days). The patients were followed-up for relapse at days 21 and 28 by the same pediatrician.
The study variables were age, sex, history of recent common cold, postnasal discharge, cough, headache, parent education levels.
The inclusion criteria for this study were a history of recent upper respiratory infection, postnasal discharge and/or nasal congestion for more than 10 days and less than 30 days. Patients with severe symptoms (fever≥39 centigrade with purulent nasal discharge at least for 3 days), chronic sinusitis, history of any nasal or adenoid surgery and those with probable complications (e.g., per orbital swelling), cystic fibrosis and history of allergy to amoxicillin, IgA deficiency, gasteroesophagial reflux, and palat defect were excluded.
The Centers for Disease Control and Prevention (CDC) recommends reserving the diagnosis of acute bacterial rhinosinusitis for patients with symptoms lasting at least 7 days, purulent nasal secretion and one of the symptoms maxillary pain, tenderness in the face (especially unilateral) and tenderness of the teeth (especially unilateral)15).
The return of respiratory symptom while still carrying out treatment considered as relapse16). In general, patients with acute bacterial rhinosinusitis begin to respond clinically after 3 to 5 days following initiation appropriate antibiotic therapy. If sign and symptoms worsen despite 72 hours of antibiotic treatment, the possible treatment failure should be considered16).
A pediatrician visited patients at days 0, 3, 14, 21, and 28. In each visit, patients were physically examined and asked (patients or their parents) about treatment compliance, symptoms relapse, side effects, and change in school functioning, absence from school and treatment satisfaction. In a checklist pediatrician recorded the patient's respiratory condition, if a particular symptom was present initially, a score of 1 was assigned; and if it was absent. In this study, cure was defined as complete absence of sinusitis respiratory signs and symptoms such as cough, and nasal discharge or congestion according to pediatrician diagnosis17).
1. Nasal irrigation
On study entry, children in the nasal irrigation group and their parents were instructed about usage of nasal irrigation with saline normal 0.9% and nasal phenylepherin 0.25%. Saline nasal irrigation was administered using a disposable syringe filled about with 15-20 mL of NS 0.9% for each nostril and 1-3 times a day for five days. The saline normal solution were irrigated fast upward in a sitting or standing position, with the head pulled back to allow the secretions to flow down ward from the nose without the patient breathing them in9). Nasal phenylepherin 0.25% was used 2-3 times for two days.
2. Statistical analysis
The data analysis was made using PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA). All collected data were expressed as a mean and standard deviation. The Independent-samples t test and one-way analysis of variance was chosen to compare the improve rate of symptoms between the two groups. Fisher exact test was chosen to determine the relationship between ages and cure rate in each groups. P value less than 0.05 was considered as significant.
Results
In each study group, ten patients were dropped during study, therefore, eighty children (40 in each group) with average age of 7.6±2.86 years old (range, 4-14 years old) were participated in this study (Fig. 1).
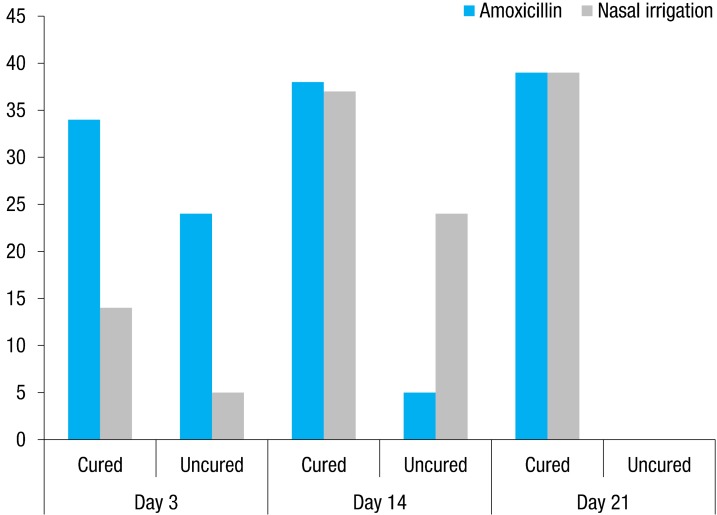
The clinical improvement according to initial symptoms in study groups. At the day 3, there was significant difference between two groups in cure process (P<0.001).
There was no significant difference in baseline demographic and health characteristics such as age and sex among the patients of the two groups (P>0.05) (Table 1).
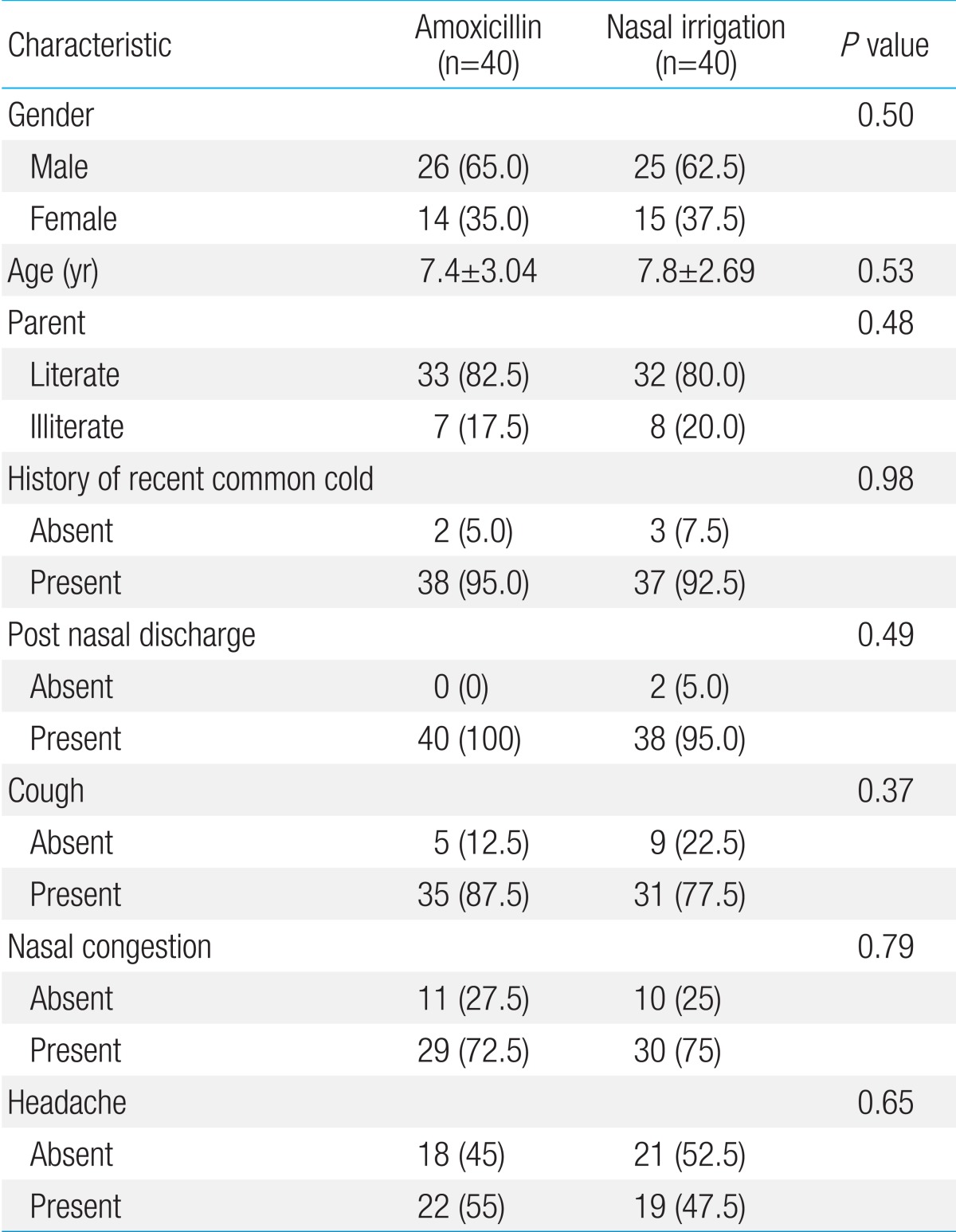
Demographic characteristic and sign and symptoms of acute sinusitis at the beginning of study in two study groups
Findings of study did not show any significant relationship between sex and cure rate in each groups of study at days 3, 14, 21, and 28 (P>0.05). In addition, there were no significant relationship between age and cure rate in each groups of study at days 14, 21, and 28 (P>0.05), but at day 3 in intervention group, older children had better condition (P<0.05). Furthermore, findings of study showed no significant relationship between treatment efficacy and history of common cold in study groups in days 3, 14, 21, and 28 (P>0.05).
Clinical cure in patients was examined according to their initial respiratory symptoms. On the third day of treatment, 34 of children (85%) in amoxicillin group were cured compared with 15 of the children (37.5%) in the nasal irrigation group. On the 14th day of treatment, 39 of children (97.5%) in amoxicillin group were cured compared with 38 of children (95%) receiving nasal irrigation. All patients were cured completely at days 21 and 28 and did not have any relapse. Only at the day 3, there was significant difference between two groups and patients in amoxicillin group had better condition and their symptoms were subsided (P<0.001), but in other days of follow-up there were no significant difference in cure process in two groups (P>0.05). Therefore, the children receiving high dose amoxicillin with saline nasal irrigation recovered more quickly and more often than those receiving saline nasal irrigation alone (Fig. 1).
Discussion
Despite of the common usage of antibiotic in treatment of acute sinusitis in children, efficacy of this treatment is controversies18).
The necessity and the choice of antimicrobial therapy in children acute sinusitis remains controversial. However, the long-term effects of antimicrobial use on resistance patterns at the population level remain unmeasured and need to be considered in the revised guidelines. There are still limited data to guide the diagnosis and management of ABS in children. Diagnostic and treatment guidelines focusing on severity of illness at the time of presentation have the potential to identify those children most likely to benefit from antimicrobial therapy and at the same time minimize unnecessary use of antibiotics"19).
The result of present study showed that the clinical improvement in patients who received amoxicillin was more rapid than nasal irrigation group, but follow-up showed no significant difference in cure rate in two groups. All patients were cured completely at days 21 and 28 and did not have any relapse. In addition, we did not show any side effects in two groups of study.
Evidence to support antibiotic treatment for acute rhinosinusitis is limited, but antibiotics are commonly used. Garbutt et al.20), did a randomized, placebo-controlled trial study to determine the incremental effect of amoxicillin treatment over symptomatic treatments for adults with clinically diagnosed acute rhinosinusitis in Missouri. Ten day course of either amoxicillin or placebo administered in three doses per day. All patients received a 5- to 7-day supply of symptomatic treatments for pain, fever, cough, and nasal congestion to use as needed. The findings of study showed no statistically significant difference in reported symptom improvement at day 3 or at day 10, whereas at day 7 more participants treated with amoxicillin reported symptom improvement.
Acute sinusitis is common and usually treated with antibiotics in spite of the lack of evidence for the effectiveness of antibiotic therapy and the increasing number of resistant strains. Falagas et al.7), did a meta-analysis of RCTs to assess the therapeutic role of antibiotics for acute sinusitis compared with placebo. Seventeen double-blind RCTs were included (three involving children). Compared with placebo, antibiotics treatment were associated with a higher rate of cure or improvement, but also with more adverse events. The rate of symptom resolution was more rapid with antibiotics in most RCTs. Falagas et al.7) concluded that the use of antibiotics for acute sinusitis deals with a small therapeutic benefit over placebo.
Guarch Ibanez et al.21), reviewed the randomized clinical trials in children with sinusitis comparing antibiotics versus placebo. Similar to findings of the present study, result of the review showed that in children with acute sinusitis, antibacterial agents did not appear benefit in terms of cure and improvement, assessed at 10 to 14 days of follow up. Similarly, the percentage of relapse was not lower among children who received antibiotics and antibiotics were associated more frequently with adverse effects.
Wang et al.9), evaluated the effectiveness of normal saline nasal irrigation in the management of acute sinusitis in children in a randomized, prospective placebo-controlled study. They evidenced that normal saline nasal irrigation decreases acute sinusitis symptoms. Nasal irrigation is an effective adjunctive treatment for pediatric acute sinusitis. Normal saline nasal irrigation in atopic children also improves allergic-related symptoms.
Nasal irrigation is an inexpensive, patient-controlled therapy that flushes the nasal cavity with saline solution, facilitating washing of the structures within. Benefits from nasal irrigation may be related to removal of nasal discharge and crusts, mucus thinning and enhancing mucociliary clearance of nasal secretions. Nasal irrigation also may decrease mucosal inflammation by osmotic changes10). This procedure has been used safely for both adults and children, and has no documented serious adverse effects. Patients treated with nasal irrigation rely less on other medications and make fewer visits to physicians. Treatment guidelines in both Canada and the US now advocate use of nasal irrigation for all causes of rhinosinusitis and for postoperative cleaning of the nasal cavity22).
Management of acute sinusitis is a controversial issue. Antibacterial treatment may be effective in selected children, but direct evidence is limited. A systematic assessment of cure rates with various antibacterial shows no consistent differences between classes22).
In conclusion, regarding to high rate of antimicrobial agent resistance in study area according to previous study of Khoshdel et al.13) and the effectiveness of high dose amoxicillin and saline irrigation in the same manner, it seems that saline nasal irrigation could be effective in treatment of acute sinusitis in children, but uses of antibiotics for acute sinusitis confer a small therapeutic benefit over the nasal irrigation. The current rates of antimicrobial resistance among commonly implicated pathogens should be considered in therapeutic decisions in acute sinusitis. Nasal irrigation is a simple and inexpensive treatment that relieves the symptoms of sinusitis, reduces use of medical resources, and could help minimize antibiotic resistance. Further research is needed to determine whether the interventions are beneficial in the treatment of children with acute sinusitis.
Acknowledgments
We would like to thank the parents of children who participated in this study. This study was financially supported by Shahrekord Medical University of Sciences, and registered in IRCT by 2012111511470N1.
Notes
No potential conflict of interest relevant to this article was reported.