A case of bilateral submandibular gland mucoceles in a 16-month-old child
Article information
Abstract
Mucoceles are common benign cystic lesions of the oral cavity that develop following extravasation or retention of mucous material from the major or minor salivary glands. Mucoceles are usually located in the lower lip (60 to 70% of cases), and the floor of the mouth is only involved in 6 to 15% of cases. Submandibular gland mucocele is extremely rare but should be considered in the differential diagnosis of swelling at the submandibular triangle in young children. We present the rare case of a 16-month-old child who was diagnosed with bilateral submandibular gland mucocele, presenting as serial swellings in both submandibular regions. We removed the cystic mass with the submandibular and sublingual glands to prevent recurrence.
Introduction
The differential diagnosis of neck mass in childhood encompasses congenital, inflammatory, and neoplastic origins. The majority of pediatric neck masses are either of inflammatory or congenital origin. A congenital neck mass is usually present at birth, however may present at any age. Among the non-inflammatory neck masses in children, branchial cleft cyst, thyroglossal duct cyst, hemangioma, laryngocele, mucocele, teratoma, dermoid cyst, and thymic cyst are mostly well-known categories1).
Mucoceles are common benign cystic lesions of the oral cavity that develop following extravasation or retention of mucous material from the major or minor salivary glands. Mucoceles are usually located in the lower lip (60 to 70% of cases), and the floor of the mouth is only involved in 6 to 15% of cases2). However submandibular mucocele is extremely rare, with only 10 cases reported in English literature3). The age of those affected has ranged from 7 to 39 years. In the Korean literature, Kang et al.4) reported the case of a retension cyst that replaced the submandibular gland in a 19-year-old man. Yoo et al.5) reported the unusual case of huge extravasation mucocele arising from the submandibular gland in a 21-year-old woman. However, to date there has been no description of a case involving a child under the age of 5 years. Herein, we report the rare case of submandibular mucocele in a 16-month-old young child who was referred to our department complaining of serial swellings in both submandibular regions.
Case report
A 16-month-old female child was referred to our department of pediatrics complaining of a swelling in the left submandibular region that had been enlarging progressively for several days. There was no history of local trauma, surgery, or infection on that side of the face and neck. Her medical and family histories were also unremarkable. Physical examination revealed a soft, mobile, well-circumscribed superficial mass 2×2 cm in diameter in the left submandibular area. An intraoral examination revealed an absence of swelling on the floor of the mouth. Complete blood count, liver function test, C-reactive protein, tuberculosis skin test, and chest X-ray were unremarkable. Ultrasound revealed a well-circumscribed hypoechoic cystic mass measuring 2×2 cm in the anterior aspect of the left submandibular gland. A computed tomography (CT) scan with intravenous contrast revealed a well-circumscribed cystic mass measuring 2×2×2.5 cm in the left anterior submandibular gland without a "tail" sign. The mass contained no calcifications. Fine needle aspiration cytology was undertaken and revealed that the aspirated material was composed of mucus with some inflammatory cells. Surgical exploration revealed a cystic mass, which was dissected with the left submandibular and sublingual glands. A pathological examination revealed a non-epithelial lined cyst filled with mucus and mucuscontaining macrophages in the submandibular gland. There was no complication in the 2-month postoperative period.
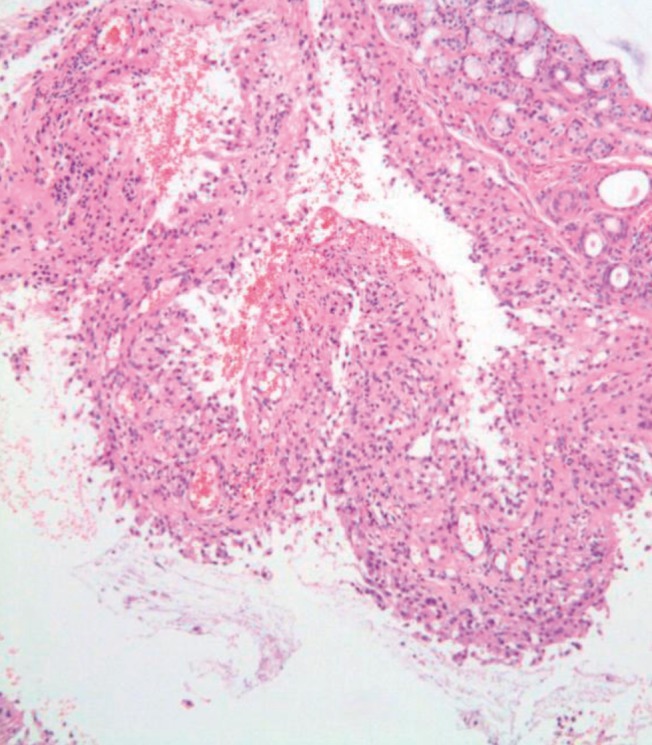
Two months later, the patient presented with swelling in the right submandibular region. CT revealed a well-circumscribed low attenuation mass measuring 2×2×2.5 cm in the right submandibular space without evidence of the "tail" sign. A post-contrast magnetic resonance imaging (MRI) examination revealed an approximately 2×2×2.5 cm sized, well-defined cystic mass containing a thick rim-enhancing smaller mass medially in the right submandibular space without evidence of the "tail" sign (Fig. 1). During surgery, the cyst was observed to be closely related to the submandibullar and sublingual glands, and also tightly adherent to the mandible bone. The cyst was totally excised with the submandibular and sublingual glands via the external cervical approach (Fig. 2). Histopathologic examination showed a mucocele ruptured with extravasation into the adjacent tissue (Fig. 3). There was no complication in the postoperative period. There was no recurrence during the 2-year follow-up period.
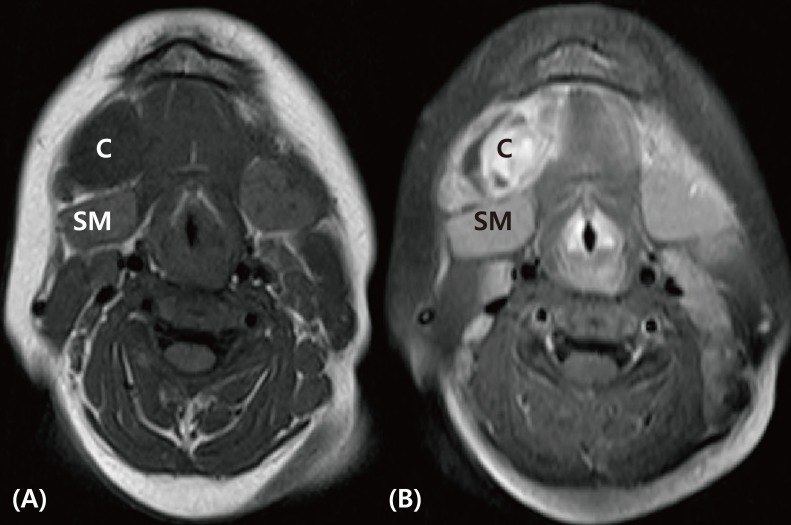
Axial magnetic resonance images through the submandibular region (postcontrast MRI). A well-defined cystic mass, about 2×2×2.5 cm in size, with thick rim-enhancing one medially in right submandibular space (C). It is in close proximity to the right submandibular gland (SM), without evidence of a "tail" sign. (A) T1-weighted (low signal intensity), (B) T2-weighted (high signal intensity). C, cyst.
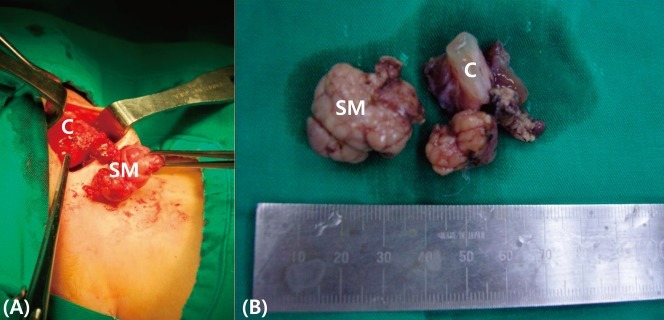
(A) Operative resection of the mass. The relationship between the cyst and submandibular is seen. (B) Gross examination of the excised specimen. C, cyst; SM, submandibular gland.
Discussion
Mucocele is a painless, slow-growing, and fluctuant swelling that is a mucus extravasation or retention of mucous material arising from the salivary gland6). The vast majorities of salivary gland cysts are of minor gland origin, comprise 6% of all parotid lesions, and are non-neoplastic and localized lesions of the duct system7). Mucocele occupies 70% of the salivary cysts and they usually arise from minor salivary glands. It is a rare occurrence in the major salivary glands (parotid, sublingual and submandibular). Extravasation cyst is found in children and young adults, while retention cyst is found in the elderly8). Mucocele originating in the submandibular gland is extremely rare. Our case was a very rare presentation as sequential masses in both submandibular regions of a 16-month-old child. Mucocle has a slight female prevalence of about 1.3:19). Our case was also female.
A mucocele is an acquired cyst of traumatic or non-traumatic origin and develops from the salivary glands10). There are two types of mucoceles-one in which mucus has extravasated into the tissues (extravasation cyst) and one which is lined with epithelium (retention cyst). Partial obstruction of the distal end of the duct will produce dilatation resulting in an epithelial-lined retention cyst, whereas disruption of the duct with mucus extravasation will produce a pseudocyst without a distint lining11,12). Our case was compatible with extravasation cyst.
Ranula is a clinical term used to designate a mucocele that occurs in the floor of the mouth. Plunging ranula and cervical ranula extend below the mylohyoid muscle, beyond the sublingual space, and involve the submandibular space and adjacent structures13). Clinically, it is difficult to distinguish plunging ranulas from mucoceles originating from the submandibular gland. Elevation of the floor of the mouth on the affected side and a bluish discoloration hint at the origin of these lesions; however, these are not always present. A CT scan with contrast and MRI can be helpful in demonstrating the origin of these lesions. Usually, when the lesion arises from the sublingual gland, a so-called "tail" sign is diagnostic14). This is a radiolucent and duct-like extension between the lesion and the sublingual gland, and it is usually located at the posterior margin of the mylohyoid muscle or in a dehiscence in the muscle. In this case, CT and MRI did not show the "tail" sign.
The diagnosis of mucocele is based principally on the clinical examination and radiographic findings. Fine needle aspiration cytology should be performed and demonstrates mucus with inflammatory cells and also can exclude other neoplastic lesions, such as malignant lymphoma. Chemical analysis of mucus contents reveals high amylase and protein contents15). CT scanning and MRI can provide accurate localization of the lesion and assist in determining its origin. Sialography provides minimal information16). After excision of the mass, histopathologic diagnosis prove confirmatory, demonstrating a cyst-like structure that is bordered by granulation tissue with no epithelial lining detected; the present case produced compatible findings.
Treatment of submandibular mucocele involves marsupialization, incision, drainage, cystectomy, excision of the sublingual gland and/or the submandibular gland with mass, irradiation, and injection of sclerosing agents17). Several investigators have suggested that to prevent recurrence, treatment of submandibular mucocele should be managed by removing the lesion with both the submandibular and the sublingual glands. The surgical modes are accomplished through transoral and transcervical approaches or through combined transoral and transcervical approaches18). The presented case, with left submandibular gland mucocele, was treated by removing the lesion. When the patient showed a right submandibular gland mucocle 2 months later, we removed the cystic mass with the submandibular and sublingual glands to prevent recurrence. Our case did not show recurrence following the second operation that removed the lesion and the submandibular and sublingual glands, in agreement with the previous literature3).
To the best of our knowledge, this is the first case of bilateral serial submandibular gland mucocele in a young child in Korea or elsewhere.
In conclusion, we describe an unusual case of bilateral serial submandibular gland mucocele in a 16-month-old female child. Submandibular mucocele is an extremely rare lesion, but should be considered in the differential diagnosis of a neck mass, even in a young child.
Acknowledgment
This case was presented by poster session at the 60th annual meeting of Korean Pediatric Society, in autumn, 2010.