Unsustainable and overworked: unpacking the challenges faced by pediatric cardiologists and cardiac surgeons in Korea
Article information
Abstract
Background
Pediatric cardiologists (PCs) and pediatric cardiac surgeons (PedCSs) in Korea face growing workforce shortages due to declining birth rates, decreasing interest among trainees, and increasing burnout.
Purpose
This study investigated the working conditions, job satisfaction, and burnout levels among Korean PCs and PedCSs.
Methods
In June 2023, the Korean Pediatric Heart Society distributed a structured questionnaire via email to 149 members actively practicing pediatric cardiac care (115 PCs, 34 PedCSs). Responses from 122 members were analyzed. Descriptive statistics and regression analyses were performed to identify the factors associated with burnout (P<0.05).
Results
A total of 122 physicians (96 PCs, 26 PedCSs) completed the survey (response rates: overall, 81.9%; PCs, 83.5%; PedCSs, 76.5%). Among the PCs, 79.2% worked more than 51 hr/wk, 57.3% worked night shifts, and 70.8% experienced emergency callbacks at least once per month. PedCSs reported comparably heavy burdens, with 80.8% working >51 hr/wk and 88.5% experiencing monthly emergency callbacks. Regional disparities were notable: 48.2% of PCs in the Seoul metropolitan area (SMA) performed >51 catheterizations annually versus 7.1% in other regions, while 62.5% of PedCSs in the SMA performed >30 surgeries annually versus 20% elsewhere. Litigation, reported by 66.7% of PCs versus 84.6% of PedCSs, contributed to dissatisfaction and burnout. The key drivers included limited research time, legal risks, and nonspecialized duties. Overall, 64.0% of the PCs and 61.6% of the PedCSs reported experiencing burnout. In the multivariable analysis, answering ≥6 emergency callbacks/mo (adjusted odds ratio [aOR], 7.91; 95% confidence interval [CI], 1.28–48.79), occupational dissatisfaction (aOR, 2.57; 95% CI, 1.09–6.04), and work environment dissatisfaction (aOR, 2.74; 95% CI, 1.16–7.14) independently predicted burnout, whereas the working >51 hr/wk variable did not remain significant postadjustment.
Conclusion
Excessive workload, frequent emergency callbacks, regional maldistribution of case volumes, litigation pressure, and occupational dissatisfaction drive high burnout among Korean pediatric cardiac specialists. These findings highlight persistent workforce challenges in Korea’s pediatric cardiac system. Regular surveys and ongoing research are essential to ensuring sustainable pediatric cardiac care.
Key message
Question: What are the key challenges affecting pediatric cardiologists and cardiac surgeons in Korea?
Finding: Excessive workloads, low procedural volumes, and legal risks contribute to high burnout. Regional disparities limit skill maintenance and threaten workforce sustainability.
Meaning: Targeted policies ensuring fair workloads, legal protections, and regional support are essential to stabilizing the pediatric cardiac workforce and maintaining high-quality care.
Graphical abstract
Introduction
Congenital heart disease (CHD) affects approximately 1% of live births and requires coordinated care from pediatric cardiologists (PCs) and cardiac surgeons (PedCSs), spanning prenatal diagnosis to long-term management [1]. In addition to CHD, these specialists also treat acquired heart conditions such as myocarditis, arrhythmias, and Kawasaki disease.
As of 2023, 298 PCs and PedCS were registered with the Korean Pediatric Heart Society (KPHS). However, only 151 PCs and 44 PedCSs either maintained or temporarily suspended their board certifications, while others had subspecialty certifications that were either expired or revoked. Compared to 2011, the number of certified PCs increased (from 137 to 151), whereas that of certified PedCSs declined (from 61 to 44). A growing shortage of residency applicants in pediatrics, thoracic and cardiovascular surgery, and obstetrics has become a major concern in Korea [2-4]. This trend has directly contributed to the aging of the PCs and PedCS workforce, as fewer young specialists are entering the field to replace the retiring generation. As of 2023, the median age had increased from 47 to 51 years for PCs and from 48 to 52.5 years for PedCSs (Supplementary Fig. 1). These aging trends, combined with Korea’s declining birth rate and regional disparities in medical resources, have raised urgent concerns about the long-term sustainability of the pediatric cardiac workforce. Reflecting this concern, the number of practicing PedCSs in Korea is projected to decline from 35 in 2021 to 17 by 2035, representing a 51.4% reduction over 14 years [5].
While workforce assessments are regularly conducted in the US, and Japan has recently carried out a similar study on PedCSs, such evaluations are still lacking in Korea [6-8].
To better understand and address the growing challenges in the pediatric cardiac workforce, the KPHS conducted a nationwide survey in June 2023. The survey aimed to identify key issues faced by PCs and PedCSs, including workload, job satisfaction, and burnout. This study analyzes the survey findings to provide evidence for future workforce planning and policy development in Korea.
Methods
This study is a secondary analysis of data from a cross-sectional survey conducted by the KPHS. The survey targeted 149 KPHS members (115 PCs and 34 PedCSs) who were actively engaged in pediatric cardiac care, including those whose subspecialty board certification was either active or temporarily suspended, as well as those actively practicing in the field regardless of certification status.
To collect data, we distributed a structured online questionnaire via email in 3 successive rounds between June 1 and June 30, 2023. A task force led by the KPHS chairman developed the questionnaire based on existing surveys from the Korean Society of Emergency Medicine, the Japanese Society of Pediatric Cardiology and Cardiac Surgery, and the American Academy of Pediatrics, adapting the content to the Korean healthcare context [7-9].
The anonymous web-based survey collected information on demographics (sex, age, and career stage), work environment, job satisfaction, burnout, fellowship training, career development, and healthcare policy perceptions. Given the differences in roles and workloads between PCs and PedCSs, separate but parallel questionnaires were used for each group. This analysis primarily focused on workforce status and burnout-related outcomes.
1. Statistical analysis
All statistical analyses were performed using SAS 9 (SAS Institute Inc., USA). Survey responses are summarized using descriptive statistics, including frequency distributions and measures of central tendencies. The results are presented as counts with percentages and medians (interquartile ranges). Univariate and multivariate regression analyses were performed along with chi-square tests. Statistical significance was set at P<0.05.
2. Ethics statement
Because this study relied on a previously conducted survey, the Institutional Review Board of Ajou University Hospital waived the requirement for ethical review (approval no: AJOUIRB-EX-2024-374).
Results
1. Respondent characteristics
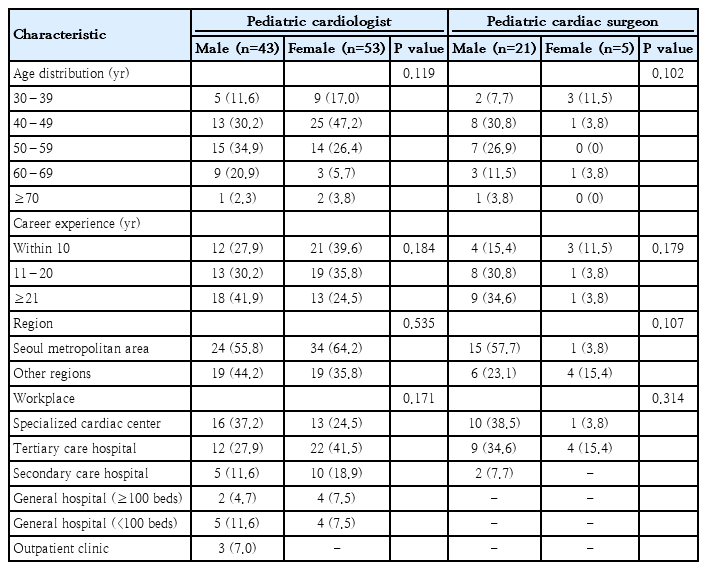
Overall, 115 PCs and PedCSs were invited to participate in the survey, and 122 responded—96 PCs (response rate: 83.4%) and 26 PedCSs (response rate: 76.5%). Among the respondents, 43 PCs (44.8%) and 21 PedCSs (80.8%) were male. Most PCs worked in specialized cardiac centers (n=29, 30.2%) or tertiary care hospitals (n=32, 35.4%), while PedCSs were similarly concentrated in specialized centers (n=11, 42.3%) and tertiary hospitals (n=13, 50.0%), with a minority (n=2, 7.7%) employed at secondary hospitals with over 100 beds. Geographically, a majority of both PCs (60.4%) and PedCSs (61.5%) were based in the Seoul metropolitan area (SMA), while the remaining 38 PCs (39.6%) and 10 PedCSs (38.6%) worked in non-Seoul metropolitan areas (non-SMA) regions (Table 1).
2. Work intensity and work content
1) Weekly working hours
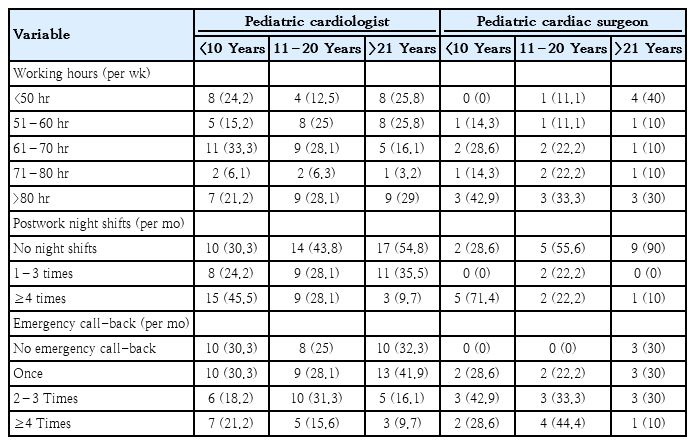
Among PCs, 76 (79.2%) worked >51 hours per week, and 25 (26.0%) worked >81 hours. Of the 31 PCs with >21 years of experience, 23 (74.2%) worked >51 hours, including 9 (29.0%) who worked >81 hours.
Similarly, 21 PedCSs (80.8%) reported working >51 hours per week, and 9 (34.6%) worked >81 hours. Among the 10 PedCSs with >21 years of experience, 6 (60.0%) and 3 (30.0%) exceeded 50 and 80 hours, respectively (Table 2).
2) Postwork night shifts
In this study, postwork night shifts refer to overnight duty following a full day of clinical work. A total of 55 PCs (57.3%) and 10 PedCSs (38.5%) reported working postwork night shifts. Among them, 27 PCs (28.1%) and 8 PedCSs (30.7%) experienced postwork night shifts more than 4 times per month. Postwork night shifts were less common among PedCSs with more colleagues or >21 years of experience and among PCs in smaller hospitals or with extended professional experience (Table 2).
Following postwork night shifts, only 5 PCs (9.1%) took the next day off, while the majority either resumed regular duties (n=36, 65.5%) or followed a routine schedule the next day (n=14, 25.5%). Similarly, 9 PedCSs (90%) resumed regular duties immediately, with only one reporting a variable schedule.
Night-shift duties for both PCs and PedCSs often extended beyond pediatric cardiac care. PCs frequently managed general pediatric inpatients (69.1%), emergency room cases (45.5%), and patients in neonatal or general intensive care unit (ICU), while only 25.4% were assigned to the pediatric cardiac ICU. PedCSs similarly covered thoracic and cardiovascular ICU, emergency department, and general inpatient ward, with only 20% involved in post-operative pediatric cardiac ICU cases.
3) On-call duties and emergency callbacks
Among PCs, 68 (70.8%) experienced at least one emergency call-back per month—defined as being required to return to the hospital in person after completing regular or overnight duties—with 15 (15.6%) reporting 4 or more such instances. This trend was consistent across career stages: emergency call-back at least once per month was reported by 69.7% of those with <10 years, 75% with 11–20 years, and 67.7% with >21 years of experience. Similarly, among PedCSs, 23 (88.5%) reported at least one emergency call-back per month, and 7 (26.9%) experienced 4 or more instances (Table 2).
4) Presence of colleagues
Among PCs working in the SMA, 27 (46.6%) reported working alone, compared to 31 (81.6%) in non-SMA regions. Conversely, 29 PCs (50.0%) in SMA and only 3 (7.9%) in non-SMA regions worked with 3 or more colleagues. Additionally, 21 PCs (36.2%) in SMA worked alongside 7 or more colleagues. Among PedCSs, 3 (18.8%) in SMA and 2 (20.0%) in non-SMA regions worked alone. In contrast, 9 PedCSs (56.2%) in SMA and 2 (20.0%) in non-SMA regions reported working with 3 or more colleagues.
2. Case volume and skill maintenance
1) Cardiac catheterization volumes
To maintain technical proficiency in cardiac catheterization, most PCs reported a minimum number of annual procedures as necessary. Specifically, 36 PCs (37.5%) recommended at least 30 procedures annually, while 26 (27.5%) suggested >50 procedures annually. Among 84 PCs working at hospitals equipped for catheterization, 27 (48.2%) in the SMA and 2 (7.1%) in non-SMA regions performed ≥51 procedures annually (Fig. 1A).
Annual volumes of cardiac catheterizations and surgeries for congenital heart disease (CHD) stratified by geographic region and years of experience. (A) Annual volume of cardiac catheterizations by geographic region. (B) CHD surgery volumes by geographic region. (C) CHD surgery volumes by years of professional experience. The bar segments represent the proportion (%) of respondents in each category, with the number of respondents (n) shown within each segment. In panel A, “Capable but not performed” refers to respondents who are qualified to perform procedures but unable to do so owing to institutional constraints.
Despite having access to the necessary facilities, a substantial proportion (15 PCs [26.7%] in the SMA and 16 [57.1%] in the non-SMA regions) were unable to perform cardiac catheterizations.
The primary barriers cited were the absence of cardiothoracic surgical backup (70.9%), limited procedural opportunities (54.8%), and patient preferences for transfer to larger centers (35.5%).
2) CHD surgical volumes
When asked about the minimum number of CHD surgeries required to maintain surgical proficiency, 36% of PedCSs suggested 50 cases annually, 32% suggested 25, 32% suggested 100, and 4% suggested 150. However, only 8 PedCSs (32%) performed >100 surgeries annually, while 4 (16%) performed 61–100, 4 (16%) performed 30–60, 9 (34.6%) performed <30, and 1 performed none. Regarding regional distribution, 62.5% of PedCSs in SMA performed >30 surgeries annually, compared to just 20% in non-SMA regions (Fig. 1B). When stratified by career stage, only 28.5% of PedCSs with <10 years of experience performed >60 surgeries, compared to 55.5% of those with 11–20 years and 50% of those with >20 years (Fig. 1C).
Respondents primarily attributed the decline in CHD surgeries to falling birth rates (n=11) and the concentration of patients at large metropolitan hospitals (n=10). Additional factors identified included hospital oversaturation (n=1), a decrease in the number of foreign patients following the COVID-19 pandemic (n=1) in SMA areas, an inadequate hospital infrastructure (n=2), and limited clinical experience among local specialists (n=2) in non-SMA regions.
3. Medical disputes and litigation experience
Among PCs, 33.3% had direct and 33.3% had indirect experience with legal disputes related to medical incidents, including prelitigation processes such as mediation or settlements. Among those with direct experience, half reported reducing care for high-risk patients, while 34.4% with indirect experience reported similar changes.
Litigation-related experiences were more common among PedCSs, with 50% (n=13) reporting direct involvement and 34.6% (n=9) reporting indirect involvement. After direct disputes, one PedCS reduced the number of high-risk surgeries, while the others continued their practice despite concerns. Among those with indirect experience, one PedCS reduced procedures, and 7 acknowledged risks without changing their practice.
4. Satisfaction and burnout
1) Professional pride and identity satisfaction
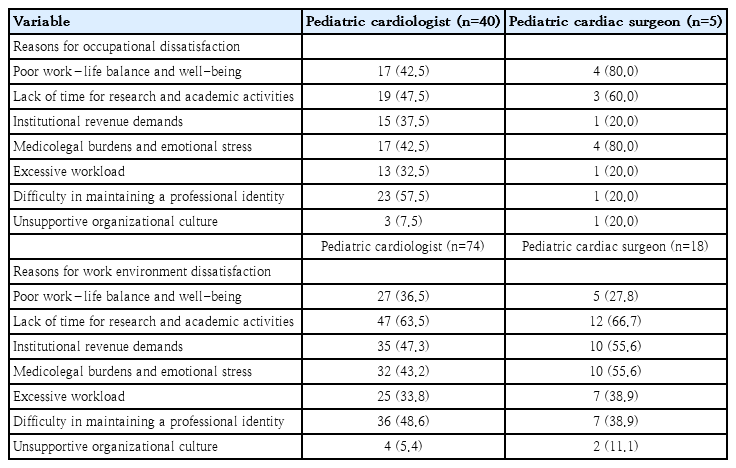
Among the respondents, 58.3% of PCs and 80.7% of PedCSs reported being satisfied with their roles as pediatric cardiac specialists. Dissatisfaction among PCs was primarily associated with a lack of time for family and self-care (n=27, 67.5%), difficulty maintaining professional identity due to nonspecialized clinical assignments (n=23, 57.5%), limited time for research activities, declining patient volumes (n=19, 47.5%), and concerns regarding legal risks and the psychological burden of treating critically ill pediatric patients (n=13, 32.5%). Among PedCSs, dissatisfaction was primarily attributed to a lack of time for family and self-care (n=3), legal risks and psychological burdens (n=3), and a decrease in patient numbers and research opportunities (n=2) (Table 3). Multiple responses were allowed in the survey.
2) Work environment satisfaction
When asked about satisfaction with their current work environment, 77.1% (n=74) of PCs and 73.1% (n=19) of PedCSs expressed dissatisfaction. Among PCs, the most common reasons for dissatisfaction included limited time available for research, the impact of decreasing patient numbers on academic activities (n=40, 54.1%). Additionally, many respondents reported challenges in preserving their professional identity due to non-cardiology clinical duties (n=36, 48.6%). Financial pressures related to revenue targets and inadequate compensation for workload demands were also reported by 40.5% (n=30). Similarly, dissatisfaction among PedCSs was associated with declining patient volumes, restricted research opportunities, legal risks, psychological stress, revenue constraints, and insufficient financial incentives. Additional contributing factors included excessive workloads, difficulties in maintaining professional identity, and challenges in achieving a work–life balance (Table 3). Multiple responses were permitted in the survey.
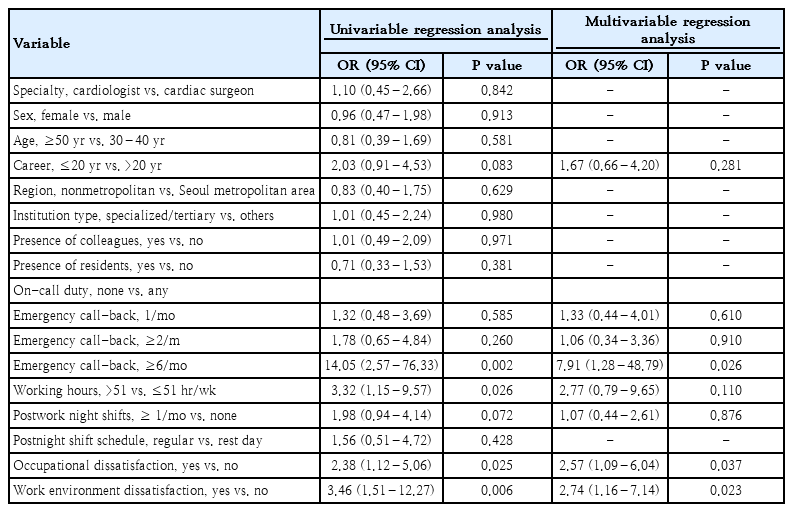
3) Burnout
Burnout was reported by 64.0% (n=61) of PCs and 61.6% (n=16) of PedCSs, with no significant differences based on sex or specialty. In the univariable analysis, being on-call and frequent emergency callbacks more than 6 times per month were significantly associated with burnout (odds ratio [OR] 14.05, 95% confidence interval [CI] 2.57–76.33, P=0.002). Additional significant factors included working >51 hours per week (OR, 3.32; 95% CI, 1.15–9.57; P=0.026), dissatisfaction with professional pride or identity (OR, 2.38; 95% CI, 1.12–5.06; P=0.025), and dissatisfaction with the work environment (OR, 3.46; 95% C,I 1.51–12.27; P=0.006). Although not statistically significant, having <20 years of clinical experience and working postwork night shifts more than once a month showed a trend toward increased burnout risk. Moreover, the presence of colleagues, residents, or practicing in nonmetropolitan areas was not significantly associated with burnout (Table 4). In the multivariable analysis, being emergency callbacks more than 6 times per month remained a strong independent predictor of burnout (OR, 7.91; 95% CI 1.28–48.79; P=0.026). Dissatisfaction with professional pride or identity (OR, 2.57; P=0.037) and dissatisfaction with the work environment (OR, 2.74; P=0.023) also remained significantly associated with burnout. In contrast, after adjustment working >51 hours per week was not significantly associated with burnout (OR, 2.77; P=0.110) (Table 4).
Discussion
This national survey highlights the critical workforce challenges facing PCs and PedCSs in Korea. Factors contributing to dissatisfaction and burnout among these specialists include excessive workloads, frequent postwork night shifts, emergency callbacks, declining case volumes, legal risks, and insufficient support systems. The findings confirmed that excessive working hours and frequent emergency callbacks are closely associated with burnout. Particularly, being on-call and called back to the hospital more than 6 times per month remained a strong independent predictor of burnout. Dissatisfaction with professional pride or identity and dissatisfaction with the work environment were also significant contributing factors.
Beyond the issue of burnout, maintaining procedural skills is essential for ensuring patient safety and delivering quality care [10-12]. However, only 48.2% of PCs in the SMA and 7.1% in non-SMA reported performing more than 51 catheterizations annually, a threshold respondents considered necessary for maintaining technical proficiency. Similarly, among PedCSs, only 62.5% in SMA and 20% in non-SMA regions performed over 30 CHD surgeries annually. Lower case volumes were particularly evident among junior surgeons, indicating the impact of declining birth rates and regional centralization of pediatric cardiac care. International studies consistently show that higher surgical and procedural volumes are associated with better outcomes, including lower mortality and complication rates [10-14].
Recommendations from professional societies in Europe and Japan have emphasized the need for minimum institutional volumes and specialist numbers to sustain high-quality pediatric cardiac surgery [15-17]. For instance, Japan’s Ministry of Health, Labour and Welfare recommends that institutions performing congenital heart surgery conduct at least 100 cases annually, with each surgeon ideally performing 30 or more. Similarly, in the United Kingdom and parts of Europe, expert consensus and accreditation standards often suggest institutional volumes of 250–300 surgeries per year to ensure optimal outcomes. Given these international benchmarks, the low procedural volumes observed in our survey raise concerns about skill maintenance and patient safety, particularly in hospitals in non-SMA regions.
In addition to clinical workload concerns, medical-legal risks were widespread. A substantial proportion of PCs (66.7%) and PedCSs (84.6%) reported direct or indirect involvement in legal disputes. Among PCs, nearly half of those who had experienced litigation subsequently reduced the scope of care provided to high-risk patients. Although most PedCSs continued their practice scope following legal disputes, many cited legal risks as a major contributor to psychological burden and dissatisfaction with the work environment (Table 3). These findings underscore the urgent need for legal protection measures to support physicians managing high-risk pediatric patients.
Interestingly, despite the burdens, many respondents expressed satisfaction with their professional roles. However, this sense of fulfillment often coexisted with significant dissatisfaction towards their work environment. Major causes of dissatisfaction, particularly among PCs, included limited time for research activities, disruption of professional identity owing to nonspecialized clinical tasks, revenue pressures, and legal risks (Table 3). Nonspecialized duties, such as general pediatric care or administrative responsibilities, may dilute one’s sense of professional identity and contribute toward disengagement. PedCSs reported similar challenges, including constraints on research, financial burdens, and psychological stress, although issues related to professional identity were relatively less prominent compared to PCs. This contrast underscores the need not only to support individual motivation and resilience, but also to implement system-level improvements in working conditions, institutional support, and job design.
Furthermore, regional disparities exacerbated workforce instability. PCs and PedCSs practicing outside the SMA encountered lower case volumes, fewer opportunities for skill development, and greater employment insecurity. Notably, this study highlights a structural paradox: despite facing excessive clinical workload, including long working hours and frequent postwork night shifts, many PCs and PedCS specialists reported limited procedural volumes—particularly in nonmetropolitan areas. This mismatch between workload intensity and opportunities for procedural reinforcement undermines both skill maintenance and workforce morale, posing a serious threat to long-term retention. Addressing this imbalance is critical to ensuring both the quality and sustainability of pediatric cardiac care nationwide. In particular, the lack of surgical backup regional centers was a significant barrier to performing invasive procedures; this led to reduced procedural opportunities and further erosion of professional identity.
The Korean government's 2024 initiative to expand medical school enrollments may not adequately address specialist shortages in pediatric cardiology and cardiac surgery. Without addressing the fundamental issues of declining pediatric populations, low procedural volume, employment insecurity, and legal vulnerability, merely increasing the number of trainees alone will be insufficient.
To effectively confront these challenges, targeted strategies are required. First, reimbursement policies should be revised to offer differentiated, higher compensation for complex and high-risk pediatric cardiac procedures, better reflecting their clinical difficulty and the resources required. Adequate financial incentives are essential not only to sustain the clinical practice of high-risk pediatric specialists but also to attract new trainees to this demanding field. Second, legal reforms should be introduced to establish structured mediation systems for medical disputes and to strengthen legal protections for physicians managing high-risk pediatric patients. Reducing litigation risks and psychological burdens is critical to maintaining professional engagement in high-risk pediatric care. Third, proactive government interventions are needed to address the overconcentration of pediatric cardiac patients in the SMA and to support medical infrastructure in non-SMA regions.
Proposed strategies include strengthening regional referral systems, supporting interregional patient transfers, providing direct funding to non-SMA hospitals, and implementing workforce incentive programs to encourage a more equitable distribution of specialists beyond metropolitan areas. Enhancing the capacity of non-SMA hospitals is essential to ensure nationwide access to high-quality pediatric cardiac care. Fourth, addressing the erosion of professional identity, particularly in non-SMA regions, will require not only institutional efforts but also coordinated action at the national level. A more in-depth discussion is needed to identify strategies that preserve the specialized roles of pediatric cardiac professionals while ensuring sufficient procedural exposure and ongoing skill development. Professional societies must take a leading role in establishing standardized guidelines for minimum procedural volumes, institutional requirements for invasive practice, and support systems for specialists working in resource-limited settings.
Moreover, national health policy initiatives should prioritize the reinforcement of pediatric cardiac services in non-SMA regions through targeted resource allocation, workforce incentive programs, and the development of structured regional networks for patient transfer and surgical support. Collaborative efforts between academic societies and government agencies will be essential to stabilize the workforce, protect specialist identity, and sustain high-quality pediatric cardiac care across all regions. Collectively, these strategies are crucial for addressing the current workforce challenges, ensuring continuous recruitment of new specialists, and sustaining a stable pediatric cardiac care system in the long term.
However, this study has certain limitations, including potential selection bias and limited generalizability owing to the voluntary nature of survey participation. Nevertheless, this study provides the first comprehensive national data describing the current status, burdens, and professional challenges faced by pediatric cardiology and cardiac surgery specialists in Korea. These findings offer critical insights for future workforce planning and policy development.
In conclusion, urgent systemic reforms are necessary to sustain the pediatric cardiac workforce. While this study focuses on Korea, similar challenges are likely to arise in other countries with shrinking pediatric populations and high-intensity specialties. Our findings may offer broader insights for international workforce planning in pediatric cardiac care. Ensuring appropriate procedural volumes, legal protections, and supportive work environments will be essential to preserve the professional pride and clinical excellence of future generations of pediatric cardiac specialists. Regular surveys and continued research are necessary to guide future improvements and inform long-term healthcare workforce projections in these critical fields.
Supplementary materials
Supplementary Fig. 1 is available at https://doi.org/10.3345/cep.2025.01123.
Age distribution of the respondents, including pediatric cardiologists (A) and pediatric cardiac surgeons (B). The exact number of individuals (n) is shown above each bar. IQR, interquartile range.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Acknowledgments
The authors gratefully acknowledge all members who generously participated in the survey. Their thoughtful responses provided critical insights that made this study possible.
Author Contribution
Conceptualization: MYH, CHL; Data curation: SIJ, GIBK, SHK, JYN, HJS, SWY, LYE, SYL, Cha SG, Choi KH; Formal analysis: SIJ, GIBK, SHK, JYN, HJS, SWY, LYE, SYL, SGC, KHC; Investigation: MYH, GIBK, SHK, JYN, HJS, SWY, LYE SYL, SGC, KHC; Methodology: SIJ, MYH, GIBK, SHK, JYN, HJS, SWY, LYE, SYL, SGC, KHC; Project administration: MYH, CHL; Visualization: SIJ, MYH; Writing - original draft: SIJ, MYH; Writing - review & editing: SIJ, GIBK, SHK, JYN, HJS, SWY, LYE, SYL, CHL, KHC, SGC, MYH