Need for national guidance regarding proactive care of infants born at 22–23 weeks' gestation
Article information
Abstract
With recent rapid improvements in neonatal intensive care, the limit of viability has shifted downward to 22–23 weeks' gestation. The younger the gestational age of preterm infants, the higher the risk of survival despite severe neurodevelopmental impairments. For infants born at 22–23 weeks' gestation, the limit of viability, neurodevelopmental outcomes, and survival rates may be determined by the quality of proactive care. Owing to the high risk of severe neurodevelopmental impairment in 22–23 weeks' gestation, proactive care is sometimes withheld according to ethical or legal considerations, and there are significant differences in the provision of proactive care and survival rates across countries or institutions. Additionally, there are differing or even lacking guidelines regarding the care of these infants across countries and institutions. Japan and Sweden are countries with well-established national guidance and proactive care for infants born at 22–23 weeks’ gestation, resulting in higher survival rates among them. In Korea, where there is an extreme shortage of neonatologists, maternal transfer before delivery at 22–23 weeks' gestation to high-activity regions with appropriate neonatal intensive care unit resources, such as adequate personnel and facilities similar to the centralized care model seen in Sweden, is crucial for improving the survival rates of infants born at 22–23 weeks' gestation. The survival of these infants largely depends on the quality of proactive care provided. This rate is not static and can be improved through proactive care based on national guidance and the implementation of enhanced neonatal intensive care practices, including centralization of care.
Key message
With advancements in neonatal intensive care, the limit of viability has shifted to 22–23 weeks' gestation, whose survival rates vary across countries and institutions. These rates are not static and can be improved through the proactive and centralized care guided by national protocols, including maternal transfer to high-activity regions with better neonatal intensive care practices before delivery.
Graphical abstract
Introduction
With recent rapid improvements in neonatal intensive care, the limit of viability has shifted downward to 22–23 weeks' gestation [1]. The younger the gestational age of preterm infants at birth, the higher the risk of survival with severe neurodevelopmental impairments [2,3]. However, for infants born at 22–23 weeks’ gestation, the limits of viability, neurodevelopmental outcomes, and survival rates may be determined by the quality of proactive care [4]. Owing to the high risk of severe neurodevelopmental impairment in periviable births at 22–23 weeks' gestation, proactive care is sometimes withheld due to ethical or legal considerations, and the provision of proactive care and survival rates vary widely across countries or institutions. This study aimed to examine whether survival rates of infants born at 22-23 weeks’ gestation vary between countries and institutions, and to identify the reasons for these variations. It also seeks to assess the impact of proactive care on survival rates, the effect of centralized care, and how national guidelines influence survival rates. Furthermore, this article suggests the need for guidance and centralization of care to improve the survival rates of vulnerable infants.
Periviable birth
What is considered periviable birth? What is the limit of viability? The term periviable birth refers to newborns delivered near the limit of viability, with neonatal outcomes ranging from certain or near-certain death to likely survival, often accompanied by a high likelihood of severe lifelong impairments. The definition of periviable birth was based on proceedings from a joint workshop by the Society for Maternal-Fetal Medicine, the National Institute of Child Health and Human Development (NICHD), the perinatal pediatrics section of the American Academy of Pediatrics guidelines, and the American College of Obstetricians and Gynecologists. It is defined as delivery occurring between 20 0/7 weeks and 25 6/7 weeks' gestation [5]. There are no documented cases of surviving infants born at 20 weeks' gestation and only a few case reports of surviving infants born at 21 weeks' gestation. Therefore, infants born at 22–23 weeks' gestation are often referred to as vulnerable "gray-zone" infants [6].
Survival rates vary by hospital and country
The survival rate of infants born at 22–23 weeks’ gestation varies significantly by hospital and country. However, at more advanced gestational ages, the survival rates are more consistent.
Ishii et al. [7] reported results from the Neonatal Research Network of Japan (NRNJ) in 2013 showing that the survival rate at 3 years was 36% for infants born at 22 weeks' gestation and 63% for those born at 23 weeks' gestation. Kusuda et al. [8] later highlighted a noteworthy improvement in the survival rate of infants born at 22 weeks' gestation; the mortality rate in 2018 was 40% for those born at 22 weeks' gestation and 20% for those born at 23 weeks' gestation.
Younge et al. [9] reported results from the NICHD Neonatal Research Network (NRN) in 2017, indicating that 22% of infants born at 22 weeks' gestation and 71% of those born at 23 weeks' gestation received proactive care. The survival rate of infants born at 22 weeks' gestation was less than 10%, significantly lower than that reported by the NRNJ.
There is wide variation in survival without severe complications at 22–23 weeks' gestation among hospitals and countries. Moore et al. [10] reported results from a meta analysis showing that moderate to severe neurodevelopmental impairment at 4–8 years of age decreased progressively with increasing gestational age: 43% for infants born at 22 weeks, 40% for those born at 23 weeks, 28% for those born at 24 weeks, and 24% for those born at 25 weeks. Severe neurodevelopmental impairment was defined as cerebral palsy, blindness, profound hearing loss, or developmental delay with a developmental quotient of more than 2 standard deviations below the mean requiring special educational support and supervision of daily activities. Rysavy et al. [11] reported results from the NICHD NRN showing a survival rate of 5.1% for infants born at 22 weeks' gestation, with only 3.4% of such infants surviving without severe neurodevelopmental impairment. As such, rates of survival and survival without severe disability vary among country or hospital, especially for infants born at 22–23 weeks' gestation.
Proactive care
Proactive treatment begins with active prenatal management, which includes the use of antenatal corticosteroids, tocolysis, antenatal magnesium sulfate for neuroprotection, antibiotics for preterm premature rupture of membranes, and cesarean delivery for specific fetal indications [5]. It also encompasses active postnatal management, such as resuscitation by skilled neonatologists and surfactant administration [5].
The survival of infants born during the periviable period depends largely on resuscitation and support efforts. In the United States, parental opinions often carry more weight than doctors' opinions for births at 22–24 weeks' gestation, leading to selective care based on parental preferences. At 22–25 weeks’ gestation, some families choose to forgo resuscitation or support. Furthermore, practices vary significantly among states. The American Academy of Pediatrics recommends an individualized approach to decision-making for births at 22–24 weeks' gestation [5]. The American College of Obstetricians and Gynecologists recommends resuscitation beginning at 24 weeks with consideration of resuscitation at 22 and 23 weeks' gestation [12].
Antenatal corticosteroid administration before an anticipated preterm birth is one of the most important antenatal therapies that can improve neonatal outcomes. At 22 weeks' gestation, no significant differences in outcomes were noted; therefore, the administration of antenatal corticosteroids was not recommended. However, it can be considered at 23 weeks' gestation and is recommended from 24 weeks' gestation onward. In the United States, the American College of Obstetricians and Gynecologists advises against the use of antenatal corticosteroids at 22 weeks' gestation and recommends that clinicians “consider” its use at 23 weeks' gestation. In contrast, the national guidelines in Germany and the United Kingdom [13] recommend administering antenatal steroids starting at 22 weeks' gestation when resuscitation is planned.
Antenatal magnesium sulfate is known to improve neurological outcomes and lowers the incidence of cerebral palsy when administered before 30 weeks' gestation. Magnesium sulfate prophylaxis is recommended if the periviable delivery of a potentially viable infant is expected. Its administration is advised to start at 24 weeks' gestation, can be considered at 23 weeks' gestation, and is not recommended at 22 weeks' gestation.
In the United Kingdom, decisions regarding active interventions should be made with parents using the best available evidence on the prognosis of individual babies [14]. According to a report by the British Association of Perinatal Medicine, the risk of severe impairment is roughly one in 7 among babies who receive active care and survive birth at 24 weeks' gestation, one in 4 among those at 23 weeks' gestation, and one in 3 among those at 22 weeks' gestation. Severe impairment is defined as any of the following: (1) severe cognitive impairment with an intelligence quotient <55 (<-3 standard deviation) requiring special educational support and supervision of daily activities; (2) severe cerebral palsy, classified as Gross Motor Function Classification System grade ≥3; or (3) blindness or profound hearing impairment.
For pregnancies at 22–23 weeks' gestation, decisions should consider factors beyond gestational age [14]. Risk factors such as being at the "beginning of the week" and "fetal growth restriction" increase the risk, while factors including being at the "end of the week," "female sex," and "singleton pregnancy" may lower it. Infants born at 22 weeks' gestation with unfavorable risk factors face an extremely high risk, as do those born at 23 weeks' gestation with severe fetal growth restriction. Infants born at 22–23 weeks' gestation with favorable risk factors are still considered at high risk. Palliative care is recommended for those with an extremely high risk of death or severe impairment despite treatment. For high-risk infants (those with a >50% chance of death or severe impairment), the decision to pursue proactive treatment should be thoroughly discussed with the parents. Active management is generally recommended for infants at moderate risk (with a <50% chance of death or severe impairment).
Proactive care and survival rates of periviable births
What is more important: survival, or survival without lifelong complications? The decision to prioritize mere survival over survival without severe complications influences the approach to proactive treatment for infants born at 22–23 weeks’ gestation. The approach to proactive care for these infants varies significantly according to the ethical views of the country and institution, thereby affecting their survival rates. Thus, the survival rate of infants born at 22–23 weeks' gestation depends largely on the level of proactive care provided.
According to data from the Vermont Oxford Network in the United States, the rate of proactive treatment for infants born at 22 weeks' gestation increased from 26% in 2007 to 58% in 2019. Consequently, their survival rate has tripled, rising from 5% in 2007 to 17% in 2019. This finding indicates that the survival rates of infants born at 22 weeks' gestation can improve with better neonatal intensive care practices and more proactive treatment. Additionally, variations in care practices have significantly affected the survival rates of these infants [6].
Backes et al. [15] compared the survival rates and outcomes of infants born at 22 weeks' gestation between a proactive care center in Sweden and a center in the United States that provided selective proactive care. At Uppsala University Children's Hospital (UUCH) in Sweden, all mother-infant pairs received proactive care, whereas only 22% of such pairs received proactive care at a selective center in the United States.
Infants receiving proactive care at UUCH had higher in-hospital survival rates (53% vs. 8%), greater exposure to delivery room surfactants (100% vs. 56%), and a more frequent presence of neonatologists (100% vs. 75%) than those receiving selective care. Survival up to 1 year was markedly higher in infants receiving proactive care for UUCH (53% vs. 19%). Furthermore, all mothers at UUCH received at least one dose of antenatal corticosteroids (100% vs. 20%), while 85% completed one cycle of antenatal corticosteroids (85% vs. 9%). Among survivors, those with UUCH had lower rates of severe head injury (10% vs. 67%) and neurodevelopmental impairments (30% vs. 100%).
Research using data from the United States Centers for Disease Control and Prevention across 10 regions in the United States revealed that proactive care was positively correlated with the survival rate of infants born at 22–23 weeks’ gestation [16]. The overall survival rate at 22 weeks was <20%, that at 23 weeks was 50%, and that at 24 weeks was 70%. For infants born at 22 weeks of age, survival rates ranged from 8.4% to 27.6% depending on the region. Regions with higher rates of antenatal corticosteroid administration, active postnatal care, and active neonatal intensive care unit (NICU) admission had higher survival rates for infants born at 22 weeks.
One reason for the differences in gestational age thresholds for proactive care among countries is the variation in the value placed on saving a newborn’s life versus concerns about the long-term burden of a newborn’s disabilities [17]. Neonatologists’ perceptions of the risk of severe impairment among survivors also differ. The Extremely Preterm Infants in Sweden Study (EXPRESS) Group found no association between active resuscitation and increased rates of severe impairment, which may support the more proactive approach in Sweden [18]. In contrast, the United Kingdom EPICure study reported that earlier gestation was associated with higher severe impairment rates, which may discourage United Kingdom neonatologists from resuscitating extremely preterm infants [19]. According to another survey, 33% of Swedish respondents would initiate resuscitation regardless of the infant's chances of survival compared to 21% in the United Kingdom and 6% in the Netherlands. These findings highlight the different factors influencing gestational age thresholds for resuscitating extremely preterm infants [17].
Need for centralization of care (maternal transfer before delivery)
Centralization or regionalization of care, including maternal transfer before delivery, significantly affects the survival rate of infants born at 22–23 weeks’ gestation. In Sweden, in 2014, the National Board of Health and Welfare recommended centralized care for all extremely preterm births at 6 university hospitals. Following this recommendation, the 1-year survival rate for infants born at 22 weeks' gestation in Sweden tripled from 10% in 2004– 2007 to 30% in 2014–2016, while the stillbirth rate nearly halved from 65% to 35% [4].
According to a study that analyzed United States National Database data to investigate the relationship between hospital factors and survival rates for infants born at 22–23 weeks' gestation, survival rates at birth and during the first 2 days of life were higher in urban teaching hospitals than in rural hospitals and urban non-teaching hospitals [20]. Furthermore, there was a delay in postnatal mortality among these infants from 2010 to 2018. These findings indicate that hospital factors significantly affect the survival rates of infants born at 22–23 weeks' gestation, highlighting the importance of regionalizing care and maternal transfer before delivery [20].
The survival rates of infants born at 22–25 weeks’ gestation were 62%–63% in 19 United States centers within the NRN, 66% in 637 United States centers within the Vermont Oxford Network in 2006–2012, and 70% in the Vermont Oxford Network in 2013–2016 [21]. The hospital at birth contributed as much as gestational age to predicting the survival rate, which also substantially contributed to predicting survival.
Yang et al. [22] analyzed data from the Korean Neonatal Network (KNN) and demonstrated that the survival rate of preterm infants with a birth weight of ≤500 g in Korea varies significantly depending on neonatal intensive care quality. When the NICU quality of hospitals registered with the KNN was classified into 2 groups (higher survival group and lower survival group) based on the survival rates of infants born at 23–24 weeks' gestation (≥50% vs. <50%), the survival rates of preterm infants with a birth weight of ≤500 g was significantly different (40.2% vs. 14.3%). Decreased mortality within the first 7 days of life was the primary contributor to the improved survival in higher survival group. These nationwide data showed that the survival rate of periviable infants with a birth weight of ≤500 g is not fixed and can be improved with better NICU quality care practices, starting with delivery room resuscitation. Furthermore, hospital factors, particularly the number of neonatologists working in a NICU, were independently associated with mortality rates of preterm infants in Korea [23]. The regionalization of periviable infants is essential to ensuring higher NICU quality.
National guidance
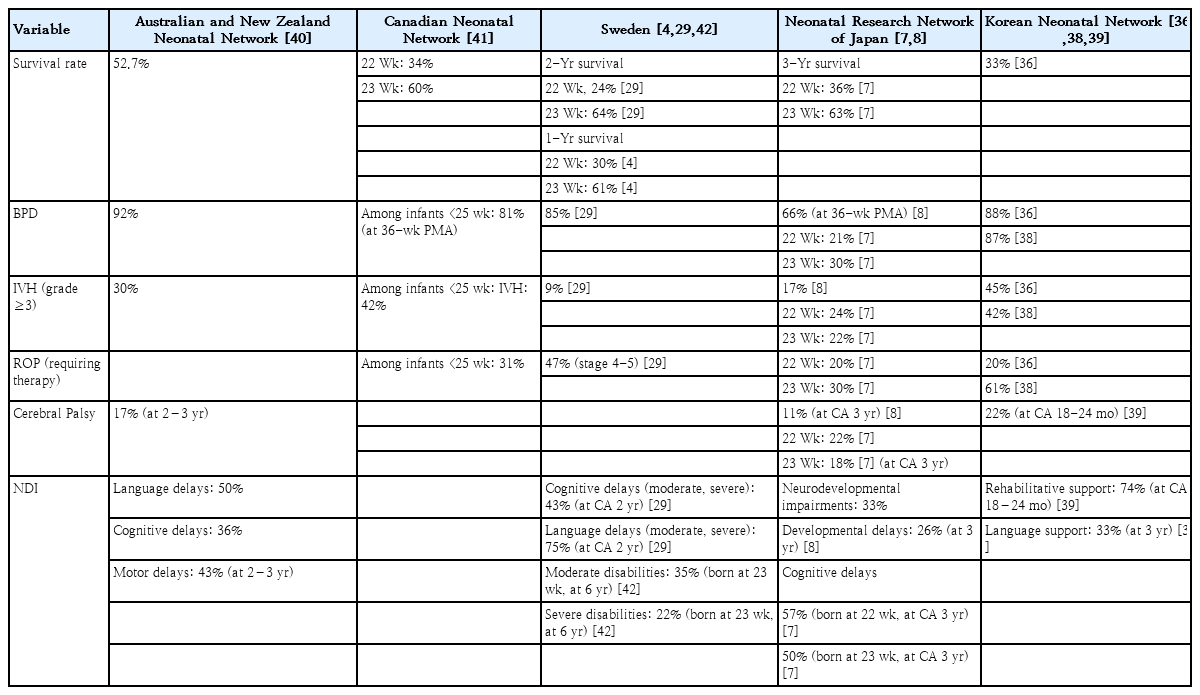
Most countries do not have national guidance and often rely on recommendations instead. Some examples of known national guidance or recommendations include the following. In 1991, the Japanese Society of Pediatrics recommended lowering the threshold for intensive care from 24 to 22 weeks based on national study data showing the survival rates of infants born at 22 and 23 weeks [24]. Following this recommendation, a 2012 national survey of the majority of Japanese NICU found that 81% of infants born at 22 weeks' gestation and 85% of infants born at 23 weeks' gestation received active resuscitation (Table 1).
In 2020, the British Association of Perinatal Medicine updated its guidelines to recommend survival-focused care for babies born at 22 weeks' gestation based on risk assessment and parental discussion [14]. Following these guidelines, survival-focused care for infants born at 22 weeks' gestation increased from 11.3% to 38.4%. NICU admissions increased from 7.4% to 28.1%, while survival to discharge improved from 2.5% to 8.2%.25) This shift to a risk-based approach has significantly enhanced survival-focused care, admission rates, and survival rates. According to the National Neonatal Network Guideline (Scottish Perinatal Network) for the management of extreme preterm infants (between 22 0/7 and 23 6/7 weeks' gestation), if infants born at 22–23 weeks' gestation receive initial resuscitation efforts including intubation and surfactant administration but remain bradycardic, an assessment should be conducted at 10 minutes of life.26) Following this assessment, a discussion with parents should be held to determine whether to continue resuscitation or focus on providing comfort care to the baby and family. If there are no signs of life by 20 minutes of life, it is considered acceptable to discontinue resuscitation efforts.
Serenius et al. [18,27] concluded that the level of proactive perinatal care affected the survival and outcomes of periviable births in Sweden. This was demonstrated by the EXPRESS group, which divided university hospitals into 2 categories based on activity levels (using perinatal activity scores derived from obstetric and neonatal indicators). Proactive perinatal care is associated with decreased mortality without increased risk of neurodevelopmental impairment at a corrected age of 2.5 years in periviable infants. This finding supports the proactive approach to optimistic expectations [27]. Consequently, in 2014, Sweden introduced new national interventionist guidelines recommending the centralization of care for all extremely preterm births at 6 university hospitals [28]. These guidelines suggest that a neonatologist should be present at birth and intensive care should be considered at 22 weeks' gestation and is generally recommended at 23 weeks. Following these guidelines, the mortality rate of infants born at 22 weeks decreased from 96% to 76%, while the 2-year survival rate increased from 4% to 24%. For infants born at 23 weeks' gestation, the mortality rate decreased from 56% to 27%, while the 2-year survival rate increased from 42% to 64% [29].
In Australia, a consensus statement developed in 2006 for the management of extremely preterm infants recommended against proactive care for infants born before 24 weeks' gestation [30]. This statement has not been revised since [31]. However, Sinclair et al. [32] found that resuscitation rates for these infants have recently increased, suggesting that the recommendations should be revised to reflect changes in clinical practice and improve the survival rate of periviable births. Kusuda [33] highlighted the findings of Sinclair et al. [32], noting that as the resuscitation rate for infants born at 22–23 weeks' gestation increased, the survival rate also improved. In the Netherlands and Denmark, intensive care is not recommended for infants born at 22–23 weeks and is only considered beyond 24 weeks’ gestation [6,17]. In France, the general policy is to withhold intervention before 24 weeks' gestation; preterm infants born earlier receive palliative rather than proactive care. Some physicians in France have extended this practice of withholding care to infants born at 25–27 weeks' gestation owing to concerns about adverse outcomes [34,35].
Outcomes of infants born at 22–23 weeks' gestation in KNN
A study by Lee et al. [36] of infants born in 2013–2016 using data from the KNN, a prospective nationwide cohort study covering more than 80% of preterm infants and including 70 participating centers in Korea [37], found that antenatal corticosteroids were administered to 63% of mothers at 22–23 weeks' gestation. The survival rate of infants born therein was 33% [36] consistent with the findings of another study of infants born in 2013–2020 [38].
Most infants had respiratory distress syndrome, with bronchopulmonary dysplasia (BPD) occurring in 88% of those born at 22–23 weeks' gestation in 2013–2016 [36] versus 87% born in 2013–2020 [38]. High-grade intraventricular hemorrhage (IVH) (grade ≥3) was observed in 45% of infants born at 22–23 weeks' gestation during 2013–2016 [36] compared to 42% during 2013–2020 [38]. Periventricular leukomalacia (PVL) occurs in 15% of infants born at 22–23 weeks’ gestation during both periods [36,38]. Additionally, 20% of infants born at 22–23 weeks' gestation in 2013–2016 required therapy for advanced retinopathy of prematurity (ROP) [36] compared to 61% of those born in 2013–2020 [38].
At a corrected age of 18–24 months, 30%–40% of infants born at 22–23 weeks’ gestation in 2013–2018 had weight, height, and head circumference measurements below the 5th percentile [39]. Specifically, 32% had a weight, 35% had a height, and 41% had a head circumference below the 5th percentile. Additionally, 74% of these infants required rehabilitative support and 22% were diagnosed with cerebral palsy, a figure that increased to 30% when cases of unknown status were included. By the age of 3 years, 33% required language support [39].
Outcomes of infants born at 22–23 weeks' gestation in other countries
According to the 2022 annual report of the Australian and New Zealand Neonatal Network, the survival rate among infants born at 22–23 weeks' gestation was 52.7% (Table 2) [40]. BPD occurred in 92% of infants, while high-grade IVH (grade≥3) was observed in 30%. At 2–3 years of age, the following delays and conditions were noted: language delays in 50%, cognitive delays in 36%, motor delays in 43%, and cerebral palsy in 17%.
According to the 2022 annual report of the Canadian Neonatal Network, an increasing proportion of infants born at 22–23 weeks' gestation are receiving proactive care in the delivery room at level 3 NICU [41]. At 22 weeks' gestation, 44% of the infants received proactive care (an increase from 24% in 2014), while at 23 weeks' gestation, 75% received proactive care (an increase from 70% in 2014). The survival rate of infants born at 22–23 weeks' gestation who received proactive care has also improved. At 22 weeks' gestation, 34% of the infants who received proactive care survived (vs. 8% in 2014). At 23 weeks' gestation, 60% of the infants who received proactive care survived (vs. 35% in 2014). Among infants born before 25 weeks' gestation, 42% had IVH, 20% had intraparenchymal lesions, and 6% (8%, including unknown cases) had PVL. At 36 weeks postmenstrual age, 81% had chronic lung disease and 31% required therapy for ROP such as laser treatment or anti-vascular endothelial growth factor therapy.
In Sweden, the survival rate was 24% at 22 weeks' gestation and 64% at 23 weeks [29]. At the 6-year follow-up of the EXPRESS study, 35% of infants born at 23 weeks' gestation had moderate disabilities, while 22% had severe disabilities. Among the infants born at 22 weeks' gestation, only 5 survived. Of them, 2 had moderate disabilities and 1 had a severe disability. However, due to the small sample size, it is challenging to draw definitive conclusions from the follow-up data of infants born at 22 weeks' gestation [42]. Among survivors born at 22–23 weeks' gestation in Sweden, 85% had BPD, 9% had IVH (grade≥3), and 47% had ROP (stage 4–5). At 2 years of corrected age, 43% of survivors had moderate to severe cognitive delays, while 75% had moderate to severe language delays [29].
According to Kusuda et al. [8], based on NRNJ data from 2003 to 2018, the overall mortality rate of infants born at 22–24 weeks’ gestation was 25%. Chronic lung disease (defined as requiring oxygen at 36 weeks postmenstrual age) occurred in 66% of cases. The incidence of IVH (grade≥3) was 17%, while that of PVL was 4%. At the 3-year follow-up, 33% of infants had neurodevelopmental impairments, with cerebral palsy in 11% and developmental delays in 26%. Ishii et al. [7] reported that 21% of infants born at 22 weeks' gestation versus 30% of those born at 23 weeks' gestation had BPD. IVH (grade ≥3) was present in 24% of infants born at 22 weeks' gestation versus 22% of those born at 23 weeks' gestation. Advanced ROP required surgery in 20% of infants born at 22 weeks' gestation versus 30% of those born at 23 weeks' gestation. At a corrected age of 3 years, cerebral palsy was observed in 22% and 18% of infants born at 22 and 23 weeks' gestation, respectively, whereas cognitive delays affected 57% and 50% of infants born at 23 weeks' gestation, respectively.
Conclusion
The approach to proactive care for infants born at 22–23 weeks' gestation varies significantly depending on the ethical views of the country and institution. Additionally, guidelines regarding the care of these infants across countries and institutions differ or are lacking completely. Japan and Sweden are example countries with well-established national guidance and proactive care protocols for infants born at 22–23 weeks’ gestation, resulting in higher survival rates. In Korea, where there is an extreme shortage of neonatologists, maternal transfer before delivery at 22–23 weeks’ gestation to high-activity regions with appropriate NICU resources, such as adequate personnel and facilities, similar to the centralization of care observed in Sweden, is crucial for improving the survival rate of infants born at 22–23 weeks’ gestation, which depends heavily on the level of proactive care provided. This rate is not static and can be improved through proactive care based on national guidance and the implementation of enhanced NICU quality care practices, including centralization of care.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This work was supported by the Inha University Research Grant.