Need for palliative care from birth to infancy in pediatric patients with neurological diseases
Article information
Abstract
Background
Palliative care is a comprehensive treatment approach that guarantees comfort for pediatric patients and their families from diagnosis to death. The techniques used for neurological patients in the field of palliative care can enhance the quality of care provided to patients with neurological disorders and support their families.
Purpose
This study aimed to analyze the palliative care protocols in use in our department, describe the palliative course in the clinical setting, and propose the implementation of hospital palliative care for long-term prognosis of patients with neurological diseases.
Methods
This retrospective observational study examined the application of palliative care from birth to early infancy in neurological patients. We studied 34 newborns with diseases affecting the nervous system impairing prognosis. The study was conducted from 2016 to 2020 at the Neonatology Intensive Care Unit and the Pediatric Unit of the San Marco University Hospital in Catania, Sicily, Italy.
Results
Despite current legislation in Italy, no palliative care network has been activated to meet the needs of the population. In our center, given the vast number of patients with neurological conditions requiring palliative care, we should activate a straightforward departmental unit for neurologic pediatric palliative care.
Conclusion
The establishment of specialized reference centers that manage significant neurological illnesses is due to neuroscience research progress in recent decades. Integration with specialized palliative care is sparse but now seems essential.
Key message
Question: What are the current palliative care protocols, palliative course, and implementable palliative care programs for hospitalized pediatric patients with neurological diseases in Italy?
Finding: We studied 34 newborns with nervous system diseases, all of whom had a poor prognosis.
Meaning: Despite current legislation in Italy, no palliative care network has been implemented. Given the vast number of patients with neurological conditions, standardized palliative care guidelines and protocols are required.
Graphical abstract.
Introduction
Palliative care focuses on body, mind, and spirit management of adults or children with incurable illness with no chance of healing, involving the global health of their families [1-4]. The World Health Organization (WHO) has long acknowledged the differences between pediatric and adult palliative care and has importantly stated that “palliative care should be commenced when illness is diagnosed, and should continue regardless of whether a child receives treatment directed at the disease” or not [5]. Within the framework of neonatal intensive care units (NICUs) various conditions are eligible to start palliative care. In case a diagnosis of a life-limiting disease is established prenatally, palliative care and family counseling is required even before birth [6]. Furthermore, most neurologic diseases remain incurable, and lead to significant disability, emotional distress, pain and other physical, psychological, and spiritual sources of pain often difficult to control. Thanks to advances in research, technology and treatment, survival of preterm neonates is increasing and consequently many of these children with neurological conditions live longer, with increasing health- and care needs, such as long-term home ventilation [7], infusion therapy, partial or complete parenteral feeding or feeding via gastrostomy tubes [8]. In these conditions, it is crucial that a multidisciplinary team specifically trained in palliative care and pain therapy coordinates the therapeutic approach with the patient’s family. A pediatric palliative care (PPC) team may be able to follow up these patients listed below throughout the perinatal period: chromosomal or genetic abnormalities, organ problems, infectious diseases, immune system disorders, as well as preterm and related complications [9]. A few neurological conditions are accompanied with behavioral problems, cognitive decline, and motor dysfunction. A multidisciplinary strategy is necessary for the management of these symptoms, and some skills should be used on a regular basis.
For the first time, a summary of children's palliative care advancements was included in the recently released European Association of Palliative Care Atlas on Palliative care in Europe 2019. Results in the Atlas show that there are still many countries in the WHO Europe Region where palliative care for children is not still available [10,11]. In our country, the Ministry of Health estimates that over 11,000 children require PPC. The prevalence of children eligible for such care has continuously and progressively increased in Italy to an estimated 32 cases per 10,000 minors [12]. It is known that only a proportion not exceeding 15% of eligible children have access to a PPC, despite Legislative Decree 38/2010, which defines that PPC is a right of the child.
In this retrospective observational study, we present our experience on palliative cares of children at early infancy and pediatric neurologic patients, whose neurologic disease diagnosis was performed at birth. We aimed to analyze the way in which the palliative care is performed in a clinical setting and to present a proposal for implementation of palliative care for these neurologic patients with poor prognosis.
The aim of our study was to assess the current organization of the palliative care from birth to early infancy in our NICU and Pediatric Unit and the consequence support provided to patients and their families. The analyzed data were gathered from the medical files and register where the records of palliative decision were documented.
We analyzed the data for a period of 4 years because no explicit record related to palliative care was recorded in previous folders.
Methods
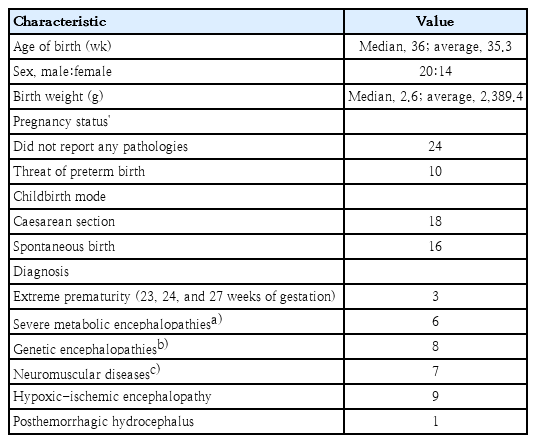
In this retrospective observational study, we analyzed the data of 34 patients, including 20 males and 14 females, born between January 1, 2016, and December 31, 2020, admitted to our NICU and/or pediatric ward for severe neurologic diseases with poor prognosis. Diagnosis of severe neurologic diseases was performed within the patients’ first 28 days of life.
All patients with experience of physical pain, social, spiritual, and emotional pain underwent to palliative cares. Decisions on palliative care were defined according to the needs of patients and their families when setting and revisiting goals of care. A multidisciplinary team assisted in the management and treatment of infants, children, with a serious neurological condition included in our study.
After diagnosis, the following patients were deemed eligible for palliative care: those who were born on the verge of viability or who are vulnerable due to their neurological disease, those who had birth anomalies that might endanger vital functions, and those whose intensive care had been applied appropriately but who were now subjected to interventions that were no longer deemed beneficial but had instead become burdensome, inappropriate, or both [9].
In our study, we excluded those patients with neurologic diseases secondary to other systemic pathologies such as tumors, neurologic coma or hepatic failure (these children were then referred to those Operative Units responsible for treatment and care of their primary disease); patients whose data in their clinical files were incomplete; patients with an incomplete checklist of all received palliative cares during hospitalization.
For each patient, we collected the following data: demographic data, anthropometrical and clinical data; diagnosis of the disease causing a poor prognosis; age at diagnosis; age of onset of palliative care; all procedures that were performed to sustain the vital functions of these children (breathing support, feeding support, pain treatment); the quality of palliative cares provided (timing, setting and healthcare professionals involved in communicating to the family the patient’s state of incurability and opportunity to start palliative care); health professionals involved in palliative cares; type of palliative cares needed by the included patients; causes and setting of death.
The research was performed in accordance with the Declaration of Helsinki guidelines [13]. All methods were carried out in accordance with relevant guidelines and regulations.
The study was approved by Ethical Committee of AOUP Rodolico San Marco - University di Catania (PO12367-21). All parents of the included patients gave their consent to participate to the present study and their consent for publication of the present data in anonymous form.
Results
We analyzed the data of 34 patients born at the NICU, San Marco University Hospital of Catania, Italy, who were diagnosed with pathologies involving the central nervous system with poor prognosis. Three patients suffering from extreme prematurity, 6 with severe metabolic encephalopathies, 8 with genetic encephalopathies, 7 with neuromuscular diseases, 9 with hypoxic-ischemic encephalopathy, and 1 patient suffering from surgically treated posthemorrhagic hydrocephalus were included in the analysis. The extreme premature patients were born at 23, 24, and 27 weeks of gestation, respectively. The 6 patients with severe metabolic encephalopathies were affected by: MELAS (mitochondrial encephalomyopathy, lactic acidosis and stroke-like episodes), MERRF (myoclonus epilepsy with ragged red fibers), Niemann-Pick C disease. The other 3 patients were suffering from neurodegenerative diseases such as: Krabbe disease, X-linked adrenoleukodystrophy, and metachromatic leukodystrophy. Regarding the genetic encephalopathies found in our patients, the specific diagnoses are: West syndrome, Dravet syndrome, SCN2A gene mutation, Rasmussen syndrome, GABRB3 gene mutation, 7q31.32 partial duplication, ATP1A3related disorder and PRRT2 gene variant. Finally, with regard to the 7 patients affected by neuromuscular diseases, the specific diagnoses are the following: Duchenne muscular dystrophy, spinal muscular atrophies (type zero and type one) and congenital myopathies. Diagnosis was performed by genetic tests (including Array-CGH and next sequencing generation) and neuroimaging exams.
This category accounts for 0.8% of those born annually in our hospital. Our data were confined to a subgroup of neonatal population who were candidates for palliative care, considering that in Sicily 42,072 children are born every year, and among them 11,640 were born in Catania.
All the included patients had a predicted end-of-life given since birth, given the severity of the neurological disease on which the palliative supports depended. All patients eligible for palliative care were started at palliation at a medium age of 7.1 months.
1. Palliative care interventions performed on included patients
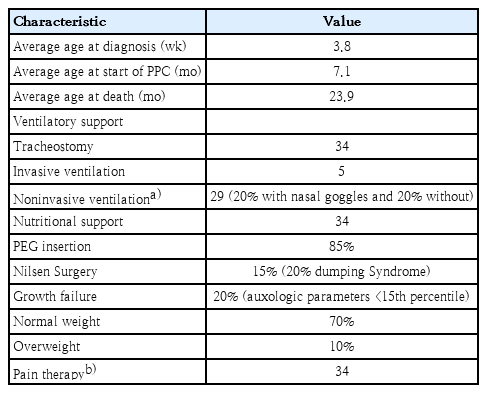
In our patients, diagnosis of a neurologic disease with poor prognosis was performed at 3.8 weeks of life. These patients then underwent to intensive care interventions when their disease worsen and they had to start palliative cares to support their vital functions, at a medium age of 7.1 months.
All patients underwent to palliative cares for ventilatory support, nutritional support, and pain therapy.
As far as the ventilator support is concerned, all patients underwent a tracheostomy. Invasive ventilation was then maintained for 5 patients, while noninvasive ventilation (NIV) was started for 19 patients (20% with nasal goggles and 80% without). NIV was performed in B level mode (inspiratory positive airway pressure 12–24 mmHg and expiratory positive airway pressure 4–7 mmHg).
The nutritional support was mainly assured by percutaneous endoscopic gastrostomy placements in 85% of patients, after 1 month of orogastric tube feeding, while 15% of patients underwent a Nielsen surgery. Among these last, 20% developed a Dumping Syndrome. The efficacy of nutrition was analyzed by the changes on auxologic parameters, and in our patients 20% showed a growth failure and their weight was under 15th percentile. 70% of patients had a normal weight and 10% overweight.
Pain therapy was started with paracetamol in all patients, and at the end-of-life was the continued with tramadol and morphine as add on therapy. Five patients (14.79%) underwent end-of-life sedation procedures with opioids. Not all patients were guaranteed respiratory physiotherapy due to the lack of specialized professional figures permanently present on the ward (Tables 1 and 2).
2. Timing, setting, and healthcare professionals involved in communicating to the family the patient’s state of incurability and opportunity to start palliative care
Between 3 and 50 days after birth, these patients' need to begin a support/palliation course was communicated. The neonatologists on duty conducted this conversation with 9 patients, while the head of the operating room conducted it with 31 patients. A psychologist then initiated conversation. Two families were given access to a weekly psychological support session hosted at the S. Marco Hospital's NICU operating room. There are no certified neonatal-pediatric experts, such as psychologists or spiritual helpers, in the San Marco University Hospital.
The conversation took place within the hospital ward in the medical room, in the chamber of the head of the operational unit, which cannot be isolated from the surrounding settings, because there were no suitable rooms available for counseling.
3. The environment in which PPCs were carried out
Of the 34 patients included in the study, 28 (82.35%) were transferred to the Pediatric Unit of the San Marco University Hospital after reaching a mean age of 50 days and 10 (35.71%) were subsequently discharged home. Of these 10 children, 3 (30%) were referred to the Pediatric Hospice of the GaribaldiNesima Hospital, 4 (40%) to the Integrated Home Care Service and 3 were referred to the Center for Metabolic Diseases in our University Hospital. As for the remaining 12 children, 12 (35%) of them remained in the NICU awaiting transfer and 12 (75%) died.
4. Professionals who were actively involved in the palliative care and therapeutic interventions
Health practitioners' inadequate understanding of Law 38/2010 and what was codified as a right of children to palliative care is one reason why the current situation is so urgent.
During hospitalization both in Neonatology and in the Pediatric Unit, nutritional interventions were performed (feeding through gavage, partial, and total parenteral nutritional therapy), ventilatory support was guaranteed (noninvasive and invasive ventilations), and pharmacological treatments suitable for the type of pathology were performed (antibiotic therapy, antifungal, caffeine, anticonvulsant). All of the infants received orogastric tube feeding and 33 of the 34 patients underwent PEG placement surgery. Five patients underwent tracheostomy and subsequently received assisted ventilation. In only 1 case, the family refused the tracheostomy procedure. The placement of an umbilical venous catheter was reported in 20 patients in the neonatal intensive care unit. None of the patients received analgetic therapy of any kind for procedures such as blood draws, intubation, or central venous catheter placement. Five patients underwent end-of-life sedation procedures with Fentanyl. Not all patients were guaranteed respiratory physiotherapy due to the lack of specialized professional figures permanently present on the ward (Tables 1 and 2).
5. Causes and setting of death
Nine out 34 patients (26.47%) are alive today and followed up at the Centre for Metabolic Diseases. Of the 25 patients who died, 4 of 25 (16%) were admitted to hospice; 15 of 25 (60%) to neonatal intensive care unit and pediatric wards, and 6 of 25 (24%) to the pediatric intensive care unit. One of the enrolled patients died in the delivery room. The causes of death of these patients were: extreme prematurity, cardiac arrest, disseminated intravascular coagulation, and shock.
The average age of death in our cohort was of 23.9 months of life.
Discussion
In our study, those patients eligible for palliative care due to severe neurologic diseases with poor prognosis represent 0.8% of the babies born yearly in our facility. It seems that palliative cares in patients with by neurologic diseases show different features than those performed on oncologic patients. In fact, our study shows that the end-of-life expectation of children with neurologic diseases seems longer than oncologic patients. As a matter of fact, these lasts are usually initiated to palliative cares when their end-of-life is already expected, according to international cancer protocols for diagnosis and treatment. There is no clear end-of-life expectation, instead, for patients with severe neurologic diseases; in fact, these patients are not able to move or speak properly, and their vital functions at the end-of-life are often related to the appropriate support of machines such as ventilator or feeding supports. Moreover, in our cohort, 9 patients (26.47%) who were expected to die, survived after palliative care onset, this underlying the need to clarify what are the right criteria to initiate palliation in these patients.
Another important finding is that neurologic patients often need an external machinery support to maintain their vital functions (mechanical ventilation, machinery feeding). In fact, in our study ventilator and feeding support were the most representative cares needed by the enrolled patients. Thus, while palliative cares in oncologic patients are “pain-centered,” in order to alleviate pain deriving from their main disease, palliative care in neurologic patients is mainly related to the use of proper machinery support. This might explain the longer life expectance of neurologic patients that is strictly related to the proper functioning of external supports.
To our knowledge, to date in the literature, there are no data on pediatric palliative assistance service for patients with neurologic diseases. This service would require specially trained professionals, including not only doctors but also psychologists, psychotherapists, palliative doctors, nutritionists, and physiotherapists. Numerous factors contribute to this, including the complexity of the issue given the patient health characteristics, the involved pathologies, and the difficulties related to the fact that health professionals lack specialized training in this area, cultural and social considerations, organizational challenges, and financial challenges. Despite considerable improvements in the identification and treatment of neurologic illnesses, little has been done to help families of these children navigate the difficult decisions that result in grave consequences for the body and mind. Moreover, there is a shortage of palliative care specialists, especially for children affected by neurologic diseases. It is therefore necessary to formulate standards for primary palliative care education for neurologists, but also to increase access to palliative care education to neurologic pediatric patients for all healthcare providers involved [14]. As seen by the absence of focus on effective pain management, we also require common treatment pathways to be used in patients designated for palliative care. Every individual has a fundamental right to early pain treatment, which is regarded as the lowest degree of care.
The network of palliative care is constantly expanding in Italy. Unfortunately, PPC is now only available to a small percentage of eligible children and only for very brief periods of time. It is also confined to isolated and highly heterogeneous patient groups. Additionally, help is typically given to these individuals in hospitals, frequently in critical care units.
Residential care dedicated to palliative care is considered as an improvement and more adequate response to the needs of the advanced and/or terminal stage of the disease. Even in Sicily, the implementation of palliative care services is continuously developing. The organizational model of the PPC network was primarily developed on a regional basis, with the aim of integrating various levels of assistance to provide real support to the minors and families in charge. On February 12, 2015, a decree was issued by the Health Department for the organization and development of the local palliative care network focusing on 3 types of care settings including hospitals, domiciles, and hospices through counseling [12,15,16]. Criteria for hospice eligibility are well developed for patients affected by oncologic diseases, but tend to be less appropriate or absent for chronic neurodegenerative diseases. Evidence-based hospice criteria for pediatric neurologic illnesses are needed [17]. A Family-Centered Developmentally Focused Care in NICU and in the Pediatric Wards should improve the palliative care support for the child-family system, with a coordinator and the rest of the care team to work closely together to design a customized and early care program for the infant. Finally, it is crucial to consider that a child is always evolving and their needs and preferences vary frequently. This leads to the necessity for moral duty on the part of the family and the medical team to support the needs of these children with an incurable condition.
1. Limitations of the study
To our knowledge, no studies on palliative care to neurologic children have been conducted to date in children with neurologic diseases diagnosed at birth. We could deduce from the presented patient population what is required to implement this therapeutic approach on a larger scale if we take into account that our data are restricted only to a portion of the neonatal population, who are candidates for palliative care for neurologic patients, and to those born in a single local hospital. Our study has some limitations, including a four-year observation duration and the fact that it is a monocentric study with a small sample of patients. To support our findings, prospective multicenter trials with a sizable patient sample are required.
2. What this study adds
The majority of the literature on palliative care up to this point has been on nonneurologic palliative care. Only adult patients have received descriptions of palliative care for neurologic patients up to this point. But it's crucial to note that 25% of diseases requiring palliative care result from severe neonatal circumstances, and 25% are caused by severe congenital abnormalities and/or chromosomal and complicated disorders. This means that about half of all diseases requiring such treatment frequently strike newborns. Tumors, neurological diseases, in particular degenerative and metabolic diseases, contribute to determine the majority of the remaining cases. As already stated in the survey published by Cavicchiolo et al. [1], which describes that in Italy there is no national consensus on palliative cares in the perinatal period, it emerges also from our study that there is no univocal therapeutic approach for patients who are introduced to a palliative care path by the healthcare personnel. In this study, we sought to pay particular attention to how palliative care for neurologic patients has been delivered in our area. We discovered that no palliative care network has been established to serve the requirements of the people, notwithstanding the statutory provisions. The skills necessary for efficient symptom management, communication, and advance care planning must be mastered by all neurologists. Knowing the course of the disease can help identify patient and family requirements quickly and make educated decisions easier.
Our research also demonstrates the need for comfort zones where the family's privacy can be assured in a sensitive and painful situation, as well as the need for regionally uniform protocols and guidelines that are understood by all medical professionals who care for the newborn with an incurable disease. It is necessary to do research on health care disparities in Italy in order to identify the underlying causes and take action to eradicate them. To promote evidence-based treatment, it might also be helpful to evaluate the effectiveness of palliative and palliative care therapies for neurologic patients. PPC is a child's right that is still too much disregarded and should be implemented in all its aspects to guarantee a better quality of life for our patients.
The issue of palliative care for neurologic patients in neonatal and pediatric age is complex and the subject of increasing attention by healthcare personnel [18,19]. It poses important questions of an ethical and also managerial nature, as it emerged from data already available in the literature [20-22]. The majority of the literature on palliative care up to this point has been on nonneurologic palliative care. There are large gaps in the provision of palliative care for people with neurologic conditions. We intended to concentrate on how the palliative care course is taught in our area in this study. Despite the legal requirements, Sicily does not have a palliative care network in place to serve the needs of the populace. Therefore, in the lack of common and established procedures, the treatment of PPC is now handled by medical professionals working in pediatrics or by doctors handling palliative care for adults. It is clear that this service has to be organized, and that a vast network must be built to ensure that such care is provided. Given the large number of kids at our facility who require palliative care treatments due to neurologic diseases, the creation of a straightforward departmental unit devoted to PPC for neurologic patients should be suggested. As soon as the kid need it, palliative care can be introduced to neurologic patients. This allows for a prompt assessment and treatment of pain and other problems, which could lead to less aggressive care and better results at the end-of-life. To provide a higher quality of life for our tiny children, palliative care is a right that is still far too often disregarded.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: RF, SM; Data curation: SM, GV, Carla Moscheo; Formal analysis: GV, SM; Funding acquisition: N/A; Methodology: RF, SM; Project administration: RF, SM, MR; Visualization: RF, SM, CM, LGT, SDM, CS, PP, GV, FS, MR; Writing-original draft: SM, GV, CM, PP; Writing-review & editing: SM, RF