Current diagnosis and image-guided reduction for intussusception in children: teamwork approach
Article information
Key message
∙ The successful and safe enema reduction of intussusception depends primarily on the experience and preference of the radiologists and the availability of resources.
∙ The establishment of a standardized manual or protocol for reduction and pre-reduction treatment of intussusception, along with the collaboration of pediatricians, radiologists, and surgeons, is expected to improve the treatment success rate.
Pediatricians or emergency physicians should suspect first in young children with cyclic irritability, vomiting, or bloody diarrhea [1]. If abdominal tenderness or palpable mass is present on the child’s abdominal examination, it is more likely to be intussusception.
Abdominal ultrasonography (USG) is the primary diagnostic tool for the diagnosis of intussusception [2]. Although point-ofcare USG by trained pediatric emergency physicians had high sensitivity (100%) and specificity (95.6%) [3], abdominal USG is usually performed by a radiologist rather than a pediatrician or emergency physician because most pediatric intussusception is managed in training hospitals in Korea [4]. The advantage of performing USG by radiologists is that other findings can determine the failure of enema reduction [5], including the blood supply status of the intussusception, presence of intestinal necrosis or ascites, and the pathologic leading causes can also be confirmed.
Image-guided enema reduction is the initial treatment modality for intussusception and is performed by a radiologist. The successful and safe enema reduction of intussusception depends primarily on the experience and preference of the radiologists and the availability of resources [6]. In Korea, the second-grade residents (42%) in the radiology department most commonly performed the enema reduction in training hospitals [4]. In one university hospital, among 657 cases, 596 children were successfully treated, and 12 patients (1.83%) had colon perforation from 1990 to 2001 [7]. The success rate of enema reduction was high and the severe complication of enema reduction was slightly high to the meta-analysis report (0.39%–0.43%) [8]. For safe and successful enema reduction of intussusception, the training of the radiology department residents is essential.
The pediatrician receives a consent form for enema reduction from the parents after diagnosis of intussusception. Enema reduction should be performed with parental understanding and consent of the procedure and complications of enema reduction. It is imperative to explain how to perform enema reduction, its complications, and the possibility of failure. In addition, when enema reduction fails, or complications develop, it is necessary to explain and obtain consent for emergency surgery. Therefore, enema reduction can be performed in hospitals where surgery is possible. In cases of failure of enema reduction, intestinal perforation, and multiple recurrences, only a surgeon can treat it [5], so it is necessary to prepare for surgery by communicating it in advance.
In Korea, the success rate of enema reduction for intussusception is about 82.0% to 90.0% [9,10]. The recurrence of the intussusception rate was 15.0% (4,580 of 30,444 cases) [9]. Most recurrent intussusception is also managed by enema reduction. But multiple recurrent cases are managed by surgery.
Pediatricians always consider the complications of enema reduction before and after the procedure. The most severe complication is the bowel's perforation, requiring urgent surgery. In the review of 12 colonic perforations during pneumatic enema reduction [7], the perforation site was most commonly found at the proximal part of intussusception and had a single perforation. Pathologic reports showed hemorrhagic necrosis and mesenteric laceration at the site of colon perforation. Colonic perforation during pneumatic air enema had 58.3% of tension pneumoperitoneum, requiring immediate decompression [7]. Therefore, the pediatrician should form the surgeon that enema reduction will be performed.
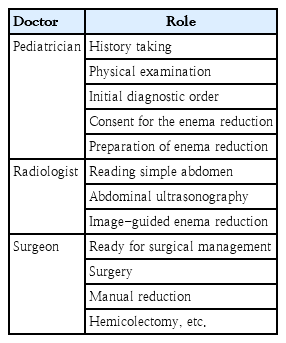
Intussusception is not a disease that a pediatrician can treat alone. The establishment of a standardized manual or protocol for reduction and pre-reduction treatment along with collaboration with related departments is expected to contribute to the reduction of complications and improvement of the treatment success rate [11]. The pediatrician must do all things to suspect the possibility of intussusception, contact the radiologist for abdominal USG, explain and consent to the parents for enema reduction, and informs the surgeon about the possibility of surgery while going for enema reduction (Table 1). In conclusion, pediatricians, radiologists, and surgeons should cooperate closely.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.