Effectiveness of comprehensive hand hygiene module on preschool children in Klang Valley, Malaysia
Article information
To the editor,
Preschool children are exposed to infectious diseases such as hand, foot, and mouth disease and colds due to their close relationship with other children at school and their weak immune systems. It has been proven that proper hand hygiene practices can curb the risk of developing these illnesses. This effectiveness study aimed to test a hand hygiene module developed for preschool children at 2 public preschools owned by Majlis Agama Islam Wilayah Persekutuan in Klang Valley, Malaysia. A total of 356 children were involved in this study; of them, 49% were boys, 45.2% were 5 years old and the rest were 6 years old.
The test group (school P) underwent 3 phases of the study, namely phase I (preintervention), phase II (intervention), and phase III (postintervention). The control group (school C) underwent only phase I and phase III. The questionnaire consisted of 2 main components: hand washing technique and hand washing knowledge. The interviewers first observed and assessed the students’ hand washing techniques. Eleven steps (adapted from the World Health Organization guidelines) were listed on the questionnaire. No hand washing education was given to the students prior to the assessment. For each hand washing step performed, the student was given one point; thus, the maximum score was 11 points. The students’ hand washing knowledge was assessed by asking them whether they wash their hands at the 5 crucial moments of after toileting, before and after meals, after playing outdoors, after sneezing and coughing, and after being in contact with pets. For each crucial moment hand washing was performed, each of the students was given one point. Thus, the maximum score was 5 points. The intervention started with of a half-day interactive hand hygiene education program that consisted of hand hygiene talk, practical sessions, and quizzes. Posters on hand hygiene steps and were put at the washing areas and notice board. Children were also given educational cards and articles to bring home. The children were educated on the importance of hand hygiene and proper hand washing technique with the aid of songs and animations. A good hand washing technique and high compliance could effectively reduce the bacterial loads on the hands [1]. To emphasize the role of hand washing in germ removal, an experiential learning approach [2] using Glo Germ liquid (Glo-Germ Product Co., Moab, UT, USA) was demonstrated, which showed that the hands might appear clean but in fact are covered with many bacteria.
The intervention was followed by 2-month-long electronic monitoring of hand washing technique using BETADINE antiseptic skin cleanser (Povidone-iodine 7.5% w/v) via the Hand Hygiene application provided by Mundipharma Pharmaceutical Sdn. Bhd (Selangor, Malaysia). A total of 22 Android-based tablets with the Hand Hygiene application were mounted at all the student’s sinks in school P. The application automatically switched on during the school session every time a student washed their hands at the sink by displaying a 2-dimensional hand washing animation while simultaneously detecting movements to monitor the students’ progress and reward them by giving stars after each hand washing step completed to facilitate and motivate the children to perform good hand hygiene practices. The data on the students’ progress was extracted once a week and exported in Excel format from the online administrator dashboard. The collected data were analyzed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA).
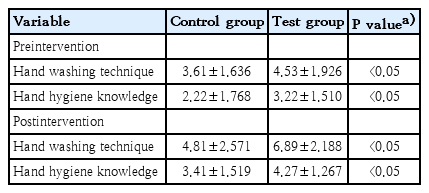
The results indicated significant (P<0.05) improvement of 52.1% for all hand washing steps in the test group after program implementation. There were statistically significant differences of 32.6% in the number of students performing hand washing at 4 of the 5 crucial times. The same results were demonstrated by similar studies in which there was an increase in hand washing frequency among children after a hand hygiene educational program [3]. Surprisingly, those who did not receive the intervention also showed improvements in hand hygiene practice. This could be a result of the Hawthorne effect [4], in which the mere presence of the researchers during the first interview might have inspired the school teachers to improve the students’ hand washing technique prior to the second interview. Nevertheless, the mean postintervention score of the control group was still lower than that of the test group (Table 1).
Another important element in hand hygiene promotion is long-term monitoring [5] because long-term and extensive initiatives can enhance the awareness of hand washing effectiveness [6]. Since the monitoring ran for a short 8-week period, the tablets provided the added advantage of saving human resources as physical guidance since monitoring requires much time and manpower [5]. However, direct observation is the most reliable monitoring method since it allows the observer to pinpoint strengths and weaknesses [7] and provide immediate education when necessary. Having a positive role model, especially among teachers and parents, also plays an important role in sustaining a social norm of hand washing among students [8]. The limitation of this study was its short intervention and monitoring period since it was conducted toward the end of the school term, resulting in the exclusion of a high number of samples mainly because of absenteeism. Additionally, the findings on hand hygiene knowledge were based on self-reported data by the preschool children.
In conclusion, this effective multifaceted approach module was designed to comply with three of 5 action areas of the Ottawa Charter for Health Promotion [9] by providing hand hygiene educational program, complete basic needs for hand washing including tissues, posters, and electronic monitoring applications, and strengthening community action by encouraging parents and teachers to adopt and enforce proper hand hygiene practice.
Notes
Ethical statement
Ethics approval was obtained from the Medical Human Ethics Committee of Universiti Sains Islam Malaysia (USIM) (USIM/JKEP/2017-20).
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was supported by Mundipharma Pharmaceutical Sdn. Bhd. (USIM/MUNDI/FPSK/052002/42817).