Phenotypes of allergic diseases in children and their application in clinical situations
Article information
Abstract
Allergic diseases, including allergic rhinitis, asthma, and atopic dermatitis, are common heterogeneous diseases that encompass diverse phenotypes and different pathogeneses. Phenotype studies of allergic diseases can facilitate the identification of risk factors and their underlying pathophysiology, resulting in the application of more effective treatment, selection of better treatment responses, and prediction of prognosis for each phenotype. In the early phase of phenotype studies in allergic diseases, artificial classifications were usually performed based on clinical features, such as triggering factors or the presence of atopy, which can result in the biased classification of phenotypes and limit the characterization of heterogeneous allergic diseases. Subsequent phenotype studies have suggested more diverse phenotypes for each allergic disease using relatively unbiased statistical methods, such as cluster analysis or latent class analysis. The classifications of phenotypes in allergic diseases may overlap or be unstable over time due to their complex interactions with genetic and encountered environmental factors during the illness, which may affect the disease course and pathophysiology. In this review, diverse phenotype classifications of allergic diseases, including atopic dermatitis, asthma, and wheezing in children, allergic rhinitis, and atopy, are described. The review also discusses the applications of the results obtained from phenotype studies performed in other countries to Korean children. Consideration of changes in the characteristics of each phenotype over time in an individual’s lifespan is needed in future studies.
Graphical Abstract
Introduction
Diverse allergic diseases, including atopic dermatitis (AD), asthma, and allergic rhinitis (AR), develop as a result of complex interactions between genetic and environmental factors. In the early era, phenotypes were artificially classified based on clinical course or chief symptoms without considering the pathophysiology of the underlying heterogeneous manifestations of allergic diseases. The recent advent of diverse cluster analysis methods, which allows complex simultaneous considerations of genetic factors, long-term clinical course, and prognosis, has contributed to the identification of more diverse phenotypes of allergic diseases (Tables 1-4). Diverse studies of the phenotypes of allergic diseases, combined with the underlying endotypes encompassing all available biomarkers, have contributed to better identification of the pathophysiology of each disease and development of treatment strategies and biologics specifically applicable to each disease phenotype [1]. Therefore, the previous concept of “one size fits all” is being replaced by the concept of “personalized medicine.”
Phenotype classification may overlap or crossover with other phenotypes during long-term follow-up. A clear-cut classification of phenotypes in allergic diseases might be impossible due to the common pathways underlying the diseases. Nevertheless, phenotype studies of allergic diseases may contribute to better understanding of the underlying pathophysiology, thereby enabling the development of personalized therapies against these diseases [2].
Considering endophenotypes, defined as a biological phenomenon in the causal chain between genotype and related symptoms [3], might better explain the complex and heterogeneous allergic diseases and, therefore, be usefully applied in clinical practice. A comprehensive approach considering the diverse environmental factors and characteristic diverse clinical symptoms combined with characteristic pathophysiologies might be the target of personalized medicine for individuals with differing genetic backgrounds and would be helpful in identifying and understanding the heterogeneous phenotypes of allergic diseases. Here we summarize the results of phenotype studies on diverse allergic diseases and atopy in children that are usually subjected to unbiased phenotype classifications [4], especially during long-term follow-up, and suggest directions for related future research.
Phenotypes of AD in children
AD is characterized by a wide spectrum, from very mild forms of dryness with minimal eczema to severe forms with later development of other allergic diseases. Some cases of AD are characterized by remission with age, with recurrence after a considerable period in other cases [5]. The diverse clinical courses of AD suggest the presence of diverse phenotypes according to the underlying pathophysiology. Predicting the clinical course at the time of AD diagnosis might help the planning of individualized treatment measures.
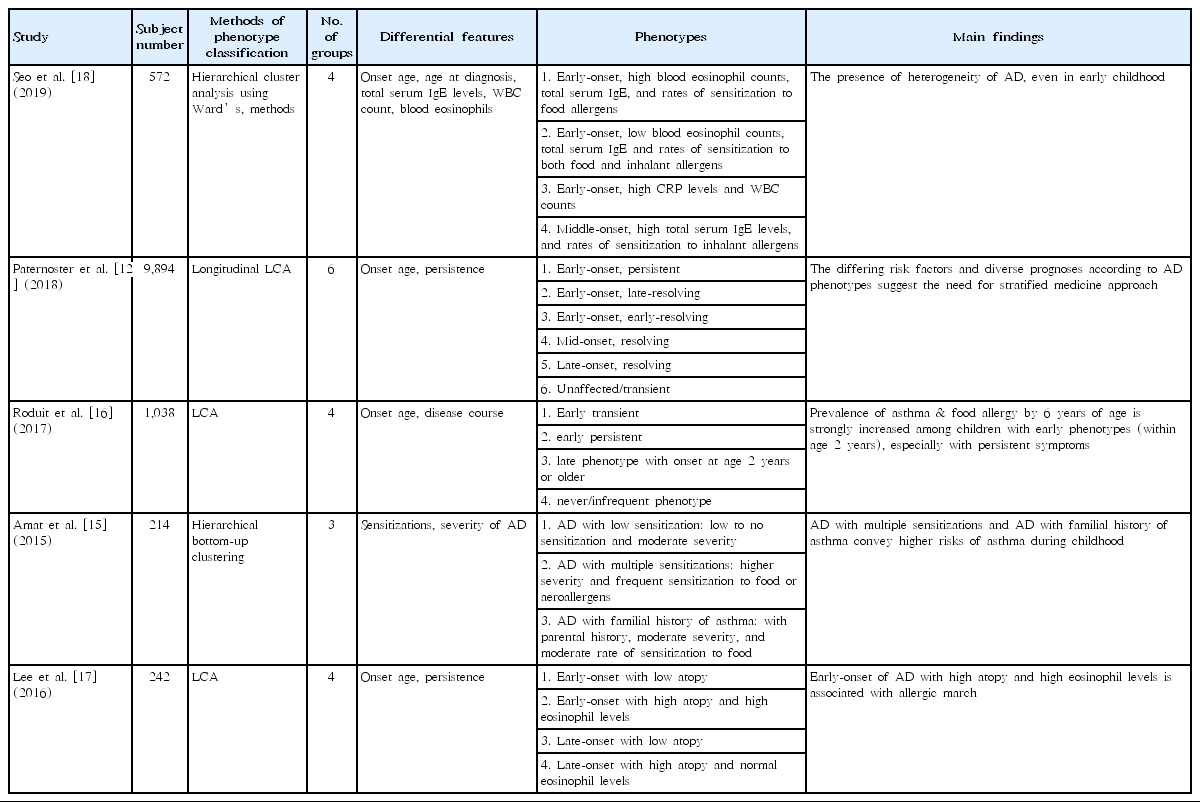
Classically, AD was divided into intrinsic and extrinsic forms [6]. The former is characterized by normal total serum immunoglobulin E (IgE) levels with nonatopy, while the latter is characterized by high total serum IgE levels with atopy [6]. However, not only do the two forms of AD have common findings, such as clinical appearance, family history, disease duration, and serum levels of interleukin (IL)-5 and IL-13 [7,8], the dichotomized classification is insufficient to explain the heterogeneous clinical courses, prognoses, and responses to specific treatment in children with AD [9]. Subsequent studies have introduced more diverse AD phenotypes, which are divided into 4–6 groups (Table 1).
The differentiating features in the classification of AD phenotypes include onset age [10-12], severity [13], treatment [14], atopy, disease course (persistence or remission), skin barrier dysfunction, and biomarkers (blood eosinophil and total serum IgE) (Table 1). Since AD develops at a relatively young age compared with other allergic diseases, studies on AD phenotypes have attempted to identify its persistence and the later development of other allergic diseases in each phenotype [15-17]. Multiple sensitizations, combined with high levels of total serum IgE and eosinophils, are commonly associated with the later development of asthma [15,17,18]. In addition, the onset age of AD combined with the presence of a food allergy is associated with asthma development in later life [16,17]. Since AD persistence affects the development of asthma and AR [19], treatment adherence in AD impacts its control and clinical course [20]; thus, adherence should be considered a strong predictor of cluster assignment in AD. However, no phenotype studies of AD have considered treatment adherence as a differential point.
Although a comprehensive concept that explains AD development has changed from complex but simple interactions between genetic and environmental factors to both skin barrier dysfunction and altered immune responses and their associated genetic background [9], phenotype studies including these factors are lacking. Genetic factors associated with skin barrier function include serine protease inhibitor Kazal-type 5 (SPINK5) and filaggrin, while those associated with immune regulation include subsets of Toll-like receptors and interleukin families [21-23]. Phenotype studies considering genetic susceptibility and explaining the differences underlying skin barrier dysfunction and altered immune regulation might better explain the pathophysiology of AD [24].
Since AD phenotypes might differ among ethnicities [24], extrapolation of the identified AD phenotypes in foreign countries arouses concerns with regard to its application to Korean children. Considering the comprehensive factors associated with AD, the identification of its phenotypes apposite to Korean children is needed to establish tailored prevention and therapeutic strategies.
Phenotypes of asthma and wheezing in children
Phenotype studies of allergic diseases have been most commonly performed in asthma and wheezing in children due to the high prevalence in early life [25]. Although the natural courses of asthma and wheezing episodes are quite heterogeneous, especially in preschool children, asthma was conventionally classified into 2 groups: extrinsic (allergic) and intrinsic (nonallergic) [26]. This dichotomized classification implies important intergroup differences in pathophysiology, such as T-cell function and cytokine levels [27]. Subsequent studies of asthma and wheezing phenotypes have considered more diverse factors, such as onset age, triggers, persistence, severity, or pulmonary function levels using unbiased methods to better reflect the underlying pathophysiology, prognosis, and treatment response for classifying phenotypes (Table 2) [28].
The first and widely used phenotypes of asthma and wheezing in children originated from the Tucson Children’s Respiratory Study [28]. In that study, wheezing phenotypes were classified into 4 groups: never wheeze, early transient wheeze, persistent wheeze, and late-onset wheeze. Among these groups, children in the IgE-associated persistent wheeze and late-onset wheeze groups showed an increased risk of asthma [28]. The results were validated in children from other countries, including Italian children [29]. These wheezing phenotypes are very helpful for pediatricians predicting the risk of asthma in preschool children with wheezing.
Subsequent wheezing phenotype studies were performed in the Avon Longitudinal Study of Parents And Children (ALSPAC) and Prevention and Incidence of Asthma and Mite Allergy (PIAMA) studies on the basis of longitudinal data from birth to 8 years of age [30,31]. In the ALSPAC study, wheezing in the preschool period was classified into 6 groups: never/infrequent wheeze, transient early wheeze, prolonged early wheeze, intermediate-onset wheeze, late-onset wheeze, and persistent wheeze [31]. In the PIAMA study, wheezing in early life was classified into 5 groups: never/infrequent wheeze, transient early wheeze, intermediate-onset wheeze, late-onset wheeze, and persistent wheeze [30]. The persistent wheeze phenotype showed an increased risk of asthma. These studies were significant in that their results suggested evidence for predicting asthma in preschool children with wheezing.
Efforts aimed at designing more sophisticated and diverse approaches to characterizing asthma phenotypes and endotypes have resulted in the identification of inflammatory phenotypes (eosinophilic, neutrophilic, mixed granulocytic, and paucigranulocytic) [32]; severe asthma phenotypes [33-36]; and diverse phenotypes encompassing asthma control status and diverse biomarkers, such as levels of exhaled nitric oxide and blood eosinophils, lung function, and cytokines [33,37]. Among the diverse variables used to classify asthma clusters, onset age of asthma or wheezing, sex, and atopy have been consistently included as important differential features [38].
The application of asthma phenotypes that originated from foreign countries to Korean children requires further validation since race affects asthma phenotypes [39]. In an asthma phenotype study of Korean school-aged children using latent class analysis, 4 phenotypes were identified: high prevalence of atopy with mild symptoms, less atopy and normal lung function but intermittent troublesome asthma, late-onset atopic troublesome asthma with decreased lung function combined with low socioeconomic status, and early-onset and less-atopic infrequent asthma [40]. Socioeconomic factors might contribute to the development and prognosis of asthma through the microbiome and its related immune responses [41].
Although phenotype studies have contributed to increasing our understanding of the pathophysiology of asthma and wheezing in children, there are some limitations to the application of the diverse phenotypes in clinical practice due to the heterogeneous characteristics of asthma. A multidisciplinary approach including molecular phenotypes, biomarkers, and clinical markers might allow the identification of asthma and wheezing phenotypes in children worldwide, thereby contributing to improvements in personalized care in children with asthma.
Phenotypes of AR in children
Although AR is common, accounting for approximately 30%–40% of children, its effect on quality of life is substantial [42], while concerns regarding AR have received less attention. Therefore, studies of AR phenotypes are relatively lacking compared with other allergic diseases. Rhinitis is conventionally classified into AR, infectious rhinitis, and nonallergic and noninfectious rhinitis, with combinations of more than 2 types in some cases. The initial classification of AR included seasonal AR and perennial AR (PAR) based on symptom timing and triggering allergens [43]. In the 2001 revision of Allergic Rhinitis and its Impact on Asthma [44], the terms “duration” and “severity” were introduced due to the considerable impact of AR on quality of life. The classification of AR based on duration (intermittent vs. persistent), severity, and its impact on quality of life (mild or moderate vs. severe) is helpful for the selection of optimal treatment [45].
However, these classifications had limited ability to explain the underlying pathophysiology and predict AR prognosis. The subsequent diverse studies on AR phenotypes used unsupervised cluster analysis methods without observer bias to better reflect the heterogeneity of AR [42,46]. Sensitization patterns, comorbidities, and treatment responses in AR are important differential features for classifying AR phenotypes (Table 3) [42,47]. AR phenotypes can be classified according to the underlying pathophysiologic features, such as high Th2 immune responses, which might be associated with treatment responses [42].
A recent study of AR classification in children with asthma showed that PAR with seasonal exacerbations was the most common type and was associated with difficult-to-control asthma [47], suggesting a linked airway disease of AR and asthma. In a cohort study followed up from birth to 18 years of age, rhinitis was classified based on sex, severity, onset age, and comorbidities into the following 4 phenotypes: moderate childhood-onset rhinitis, mild adolescent-onset female rhinitis, severe earliest-onset rhinitis with asthma, and moderate childhood-onset male rhinitis with asthma [46]. This study suggested that more severe and earlier-onset rhinitis was associated with asthma [46]. In another study in school-aged children in Korea [42], a latent class analysis considering sex, body mass index, socioeconomic status, exposure to environmental tobacco smoke, and parental history of allergic diseases revealed the following 4 phenotypes: nonatopy and low socioeconomic status, high-atopic burden but normal lung function, high-atopic burden and impaired lung function, and low-atopic burden and high socioeconomic status. In that study, children with rhinitis in the high-atopic burden and impaired lung function group exhibited an increased risk of allergic march [42].
As such, studies on AR phenotypes have identified the association between asthma prognosis and AR severity and comorbidities. This might be associated with the need for early intervention to prevent comorbidities in high-risk individuals. Studies on rhinitis phenotypes have even considered biomarkers, enabling the development of more effective treatments and individualized management. The ultimate goal of studies of AR phenotypes is developing the ability to suggest the appropriate treatment for individuals and develop therapeutics for each phenotype, thereby improving quality of life with the introduction of personalized medicine.
Phenotypes of atopy
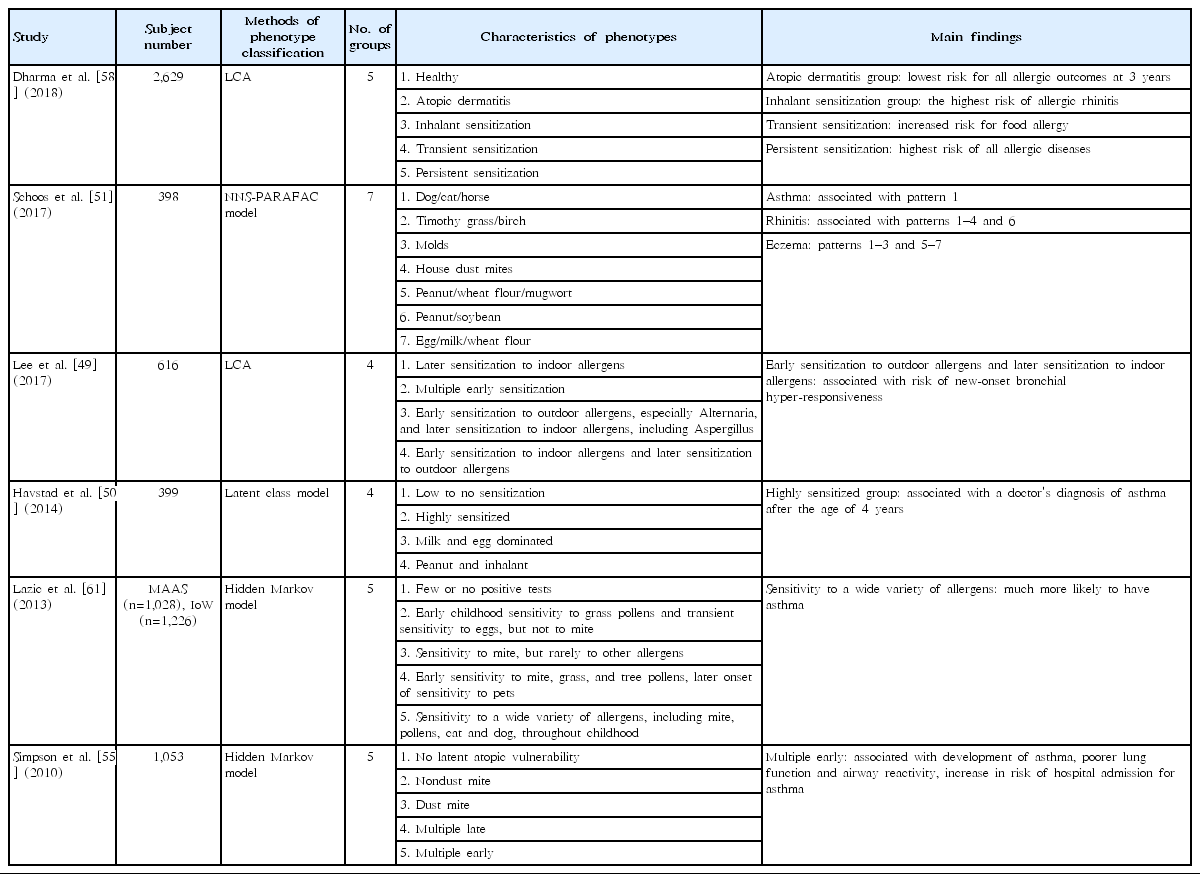
Sensitization may be among the most important features that can be used to classify the important heterogeneous allergic diseases and explain the mechanisms underlying their diverse phenotypes. Concomitant allergic sensitization also affects the risk of comorbidities in children with allergic diseases [48]. Phenotypes of sensitization are classified depending on sensitized allergen types, number of allergens, severity of sensitization, and changing patterns in sensitization during follow-up [49-53]. Since age at sensitization to specific allergens affects the association between sensitization and allergic diseases [54], assessing sensitization merely at one time point at a specific age cannot fully explain the association between sensitization and allergic diseases or their prognosis [51,55]. In addition, sensitization patterns change with age; therefore, the associations between sensitization in early life and allergic diseases might be too weak to define the endotype [54]. Therefore, identifying sensitization phenotypes over a long period and their correlation with clinical outcomes may provide information about the complex association between atopy and allergic diseases and may ultimately help predict the prognosis of allergic diseases and establish prevention strategies for children with them.
In the beginning phase of atopy phenotype studies, sensitization patterns were classified according to sensitized allergens (dust mite vs. nondust mite), number of sensitizations (mono-sensitization vs. multiple sensitizations), and sensitization period (early vs. late) [52,56,57]. These studies provide important information about the associations between sensitization patterns and prognosis of allergic diseases [48,55]. However, these studies have limited ability to explain the mechanisms underlying each phenotype of atopy and the heterogeneous spectra of allergic diseases. Subsequent studies have reported diverse atopy phenotypes encompassing more subdivided patterns and considered changes in sensitization patterns over a long-term period using unsupervised methods to decrease possible bias (Table 4) [49]. Studies considering the association between allergen sensitization, especially during early life, allergen exposure periods, including the perinatal periods, and allergic diseases might provide additional information about these associations and disease prognosis. This might better reflect the complex interactions of sensitization with allergic diseases and underlying pathophysiology [49-51].
The sensitization status is unstable, especially in early life; therefore, the consideration of temporal changes in sensitization is essential to applying the atopy phenotypes in clinical practice [48]. For example, the persistent sensitization from 1 year to 3 years is associated with an increased risk of allergic diseases, including AR, AD, and asthma, whereas transient sensitization at 1 year of age is associated with an increased risk of food allergy only [58]. Early sensitization to outdoor allergens and later sensitization to indoor allergens in school-aged children was associated with an increased risk of bronchial hyperresponsiveness [49].
However, the assessment of chronologic changes in sensitization itself might have limited ability to assess the association between sensitization patterns and allergic diseases [54]. Simultaneous consideration of the combined allergic diseases might better explain the complex association between sensitization and allergic diseases and enable better prediction of the prognosis of allergic diseases [48]. Future studies are needed on atopy phenotypes considering the diverse factors in children followed up until adulthood and their association with an exposure period to specific allergens. Further validation of whether the atopy phenotypes established in other countries can be applied to Korean children despite the differences in ethnicities is needed.
Future perspective
Previous studies have identified diverse phenotypes in each allergic disease and atopy. In the future, the identification of phenotypes that consider disease heterogeneity with regard to the genetic and exposed environmental aspects, including the perinatal period, and lifestyle changes, combined with the underlying pathogenesis, is needed. The clinical features and related immunopathophysiologies as well as long-term prognosis of each phenotype of allergic diseases might differ among ethnicities [59]. Therefore, phenotypes in allergic diseases that can be globally applied should consider the different factors according to ethnicity. Furthermore, phenotypes defined considering changes over time with regard to the pathophysiologies and immunologies, termed endotypes, might be helpful for completely understanding each phenotype of diverse allergic diseases. Research on phenotypes of allergic diseases, especially in birth cohort studies or longitudinal prospective studies, would be helpful for identifying the characteristics of each phenotype in an individual’s lifespan. Ultimately, integrated approaches including omics technology based on phenotypes of allergic diseases may be useful in developing personalized medicine and precision medicine in the future.
Conclusions
Many phenotype studies on allergic diseases using diverse methods from artificial classification to less biased machine learning approaches are available. These approaches enable better identification of the characterization of heterogeneous allergic diseases and the underlying pathophysiology of diverse allergic diseases. The differential features include clinical factors and diverse biomarkers, such as onset age, main inflammation type, persistency, severity, and comorbidities. However, these studies have limited ability to fully explain the heterogeneous diverse phenotypes of allergic diseases. In addition, the extrapolation of various phenotypes of allergic diseases in foreign countries to Korean children requires validation because of ethnicity differences. The recent approaches to phenotype classification of allergic diseases using multiple omics technologies facilitate investigations on the underlying pathophysiology of heterogeneous allergic diseases and development of personalized medicine, which are the ultimate goals of phenotype classification.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was financially supported by Chonnam National University.