A 2-month-old boy with hemolytic anemia and reticulocytopenia following intravenous immunoglobulin therapy for Kawasaki disease: a case report and literature review
Article information
Abstract
Herein, we report a rare case of hemolytic anemia with reticulocytopenia following intravenous immunoglobulin therapy in a young infant treated for Kawasaki disease. A 2-month-old boy presented with fever lasting 3 days, conjunctival injection, strawberry tongue, erythematous edema of the hands, and macular rash, symptoms and signs suggestive of incomplete Kawasaki disease. His fever resolved 8 days after treatment with aspirin and high dose infusion of intravenous immunoglobulin. The hemoglobin and hematocrit decreased from 9.7 g/dL and 27.1% to 7.4 g/dL and 21.3%, respectively. The patient had normocytic hypochromic anemia with anisocytosis, poikilocytosis, immature neutrophils, and nucleated red blood cells. The direct antiglobulin test result was positive, and the reticulocyte count was 1.39%. The patient had an uneventful recovery. However, reticulocytopenia persisted 1 month after discharge.
Introduction
Kawasaki disease is a multisystemic inflammatory vasculitis that has a high propensity to affect the coronary arteries12). Literature shows that hematologic abnormalities, such as anemia, neutrophilic leukocytosis, and thrombocytosis, are not rarely accompanied by Kawasaki disease, particularly in young infants, and that hemolytic anemia associated with high dose infusion of intravenous immunoglobulin for the treatment of Kawasaki disease often demonstrates reticulocytosis3). However, hemolytic anemia with reticulocytopenia has not been reported in patients following immunoglobulin therapy for Kawasaki disease. In this report, we describe a young infant in whom hemolytic anemia with reticulocytopenia developed during the treatment of Kawasaki disease.
Case report
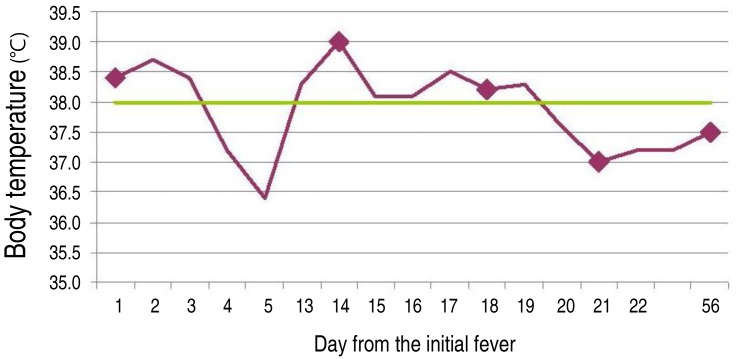
A 2-month-old boy presented with persistent high fever lasting 3 days, erythematous skin rash, red cracked lips, and strawberry tongue. He had been recently admitted and undergone treatment with ampicillin and cefotaxime for the presumptive diagnosis of sepsis. After 6 days of hospitalization without fever for the last 48 hours, he was discharged from hospital against medical advice and was switched to oral antibiotics. After having remained afebrile for 8 days at home, he was readmitted due to high fever for 3 days, conjunctival injection, strawberry tongue and lip changes, erythematous edema of hands, and macular rash on the whole body. His hemoglobin and hematocrit decreased from 9.7 g/dL and 27.1% at the first admission (initial fever) to 8.6 g/dL and 24.0% at the second admission (13th day from the initial fever), respectively. The white blood cell count was 12,340/µL with 68.7% polymorphonuclear cell, 28.8% lymphocyte, and 1.7% monocyte and platelet count was 307,000/µL. The erythrocyte sedimentation rate was 75 mm/hr. C-reactive protein level was 1.06 mg/dL. Concentration of aspartate aminotransferase and alanine aminotransferase was 173 and 224 IU/L, respectively (Fig. 1, Table 1). Lactic acid dehydrogenase was elevated as 858 U/L. The electrocardiograms and echocardiograms performed on the 17th day from the initial fever were normal. His abdominal sonogram showed mild splenomegaly. His urinalysis and cerebrospinal fluid analysis showed normal results.
Although he had merely 3 days of fever (13th day from the initial fever) and no early echocardiographic findings of Kawasaki disease, such as mitral valve regurgitation, pericardial effusion, and perivascular echogenicity, he was diagnosed with incomplete Kawasaki disease based on the other clinical signs and absence of other known causes that could explain the patient's conditions. Once the diagnosis was made, treatment with intravenous immunoglobulin of 2 g/kg and aspirin of 100 mg/kg per day was commenced without delay on the first day of readmission (13th day from the initial fever), based on the notion that children younger than 3 months of age tend to show more frequent coronary artery abnormalities when compared with children of 1 year of age4). Despite the appropriate treatment, he had fever >38.0℃ once or twice a day. On hospital day 5, he was pale and tachycardic, and had a temperature of 38.5℃. The hemoglobin was 7.4 g/dL, hematocrit 21.3%, mean corpuscular volume 85.5 fL, mean corpuscular hemoglobin 29.7 pg, reticulocytes 1.39%, and platelet count 156,000/µL. The white blood cell count was 6,690 cells/µL with 22.0% polymorphonuclear cells, 65.0% lymphocytes, 4.0% monocytes, 4.0% eosinophils, and 4% atypical lymphocytes (Fig. 1, Table 1). Direct Coombs' test was positive and indirect Coombs' test was negative, which led us to suspect the development of hemolytic anemia. Since we speculated that hemolytic anemia could be due to intravenous immunoglobulin, another infusion of immunoglobulin was not commenced in spite that he had persistent fever after the initial immunoglobulin. The hemoglobin and hematocrit stabilized at 7.8 g/dL and 23.7%, respectively on hospital day 8 (Table 1). Peripheral blood smear showed normocytic hypochromic anemia with marked anisocytosis, poikilocytosis, immature neutrophils, and nucleated red blood cells (RBCs), findings suggestive of leukoerythroblastosis (Fig. 2A, B). Iron, transferring iron binding capacity, and ferritin level was 60 µg/dL, 226 µg/dL, and 1991.5 ng/mL, respectively. There was no laboratory evidence suggestive of iron deficiency anemia. Cerebrospinal fluid, urine, and blood cultures showed no bacterial growth. The following serologic tests were all negative: Mycoplasma pneumonia, toxoplasma, rubella, Cytomegalovirus, and herpes simplex virus. Laboratory testing for adenovirus was not performed.

Peripheral blood smear performed on the 17th day from the initial fever showing nucleated red blood cells (RBCs) (A) and normocytic hypochromic anemia with myelocytes (B).
His condition improved on the 8th day from the start of the second fever (the 20th day from the initial fever) and he showed desquamation of fingers on the 10th day from the start of the second fever. He was discharged on hospital day 10 after having remained afebrile and in a stable condition for more than 48 hours. The administration of low dose aspirin was commenced at his discharge from hospital. At one month follow-up visit, he showed hemoglobin of 10.8 g/dL, hematocrit of 29.9%, reticulocyte count of 0.86%, and platelet count of 279,000/µL. The follow-up electrocardiograms and echocardiograms performed at 1, 2, 3.5, and 15 months from the initial fever were normal.
Discussion
Typical hematologic abnormalities in Kawasaki disease are neutrophilic leukocytosis and thrombocytosis. Hemolytic anemia is a rare but reported side effect of intravenous immunoglobulin therapy used for Kawasaki disease; however, there have been no case reports demonstrating that children with Kawasaki disease may show hemolytic anemia with reticulocytopenia following immunoglobulin therapy.
Hemolytic anemia following high dose intravenous immunoglobulin administration has been reported in association with the treatment of Kawasaki disease35). The major mechanism for hemolysis after administration of immunoglobulin is the direct antibody-mediated hemolysis of RBCs3). When hemolysis occurs, compensatory reaction of bone marrow is hyperplasia of erythroid, along with accelerated production of RBCs, which is reflected by reticulocytosis. The balance between RBC destruction and marrow compensation determines the severity of anemia. However, the infant in our case showed reticulocytopenia, instead of reticulocytosis.
Reticulocytopenia may be occasionally observed in a subset of autoimmune hemolytic anemia patients, often in association with leukoerythroblastosis on a blood smear test6), a finding observed in our case. Only approximately 20% of autoimmune hemolytic anemia is associated with reticulocytopenia and marrow erythroid hyperplasia7); this form is often characterized by severe anemia and a poor prognosis67). Conley et al.8) reported four cases of autoimmune hemolytic disease, where rapidly developing anemia was associated with reticulocytopenia despite intensely erythroid bone marrow. Although the pathogenesis of reticulocytopenia in patients with hemolytic anemia remains elusive, possible theories exist to explain this phenomenon. One mechanism is that it may be a consequence of an accelerated immune-mediated destruction of erythroblasts, or of autoantibody-induced apoptosis of RBC precursors in the bone marrow7910). Another mechanism would be that it may result from an inflammatory insult of the unknown microbe that has also caused Kawasaki disease on the bone marrow and its several lineages causing the hematological abnormalities and could well explain the clinical and laboratory findings of our patient. Other causes of reticulocytopenic anemia such as chronic infectious disease, renal disorder, and pure RBC anemia were not compatible with our patient's clinical characteristics.
Although the etiology of Kawasaki disease remains unknown, the epidemiological and clinical characteristics of Kawasaki disease suggest that etiologic agents are pathogenic proteins which are associated with an immature reaction of unknown initial infections, such as mononucleosis, M. pneumoniae, and various viral infections. However, in our patient, Mycoplasma, toxoplasma, rubella, Cytomegalovirus, and herpes simplex virus were not detected.
The limitation of the present study is that we did not perform further laboratory studies inquiring into specific antigens on the RBC surface that could cause hemolysis.
In conclusion, this case report is novel in demonstrating that Kawasaki disease may be complicated by hemolytic anemia with reticulocytopenia following intravenous immunoglobulin therapy in a young infant. Clinicians should be aware of this complication and hemoglobin should be closely monitored during the course of the disease.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.