Waist-to-height ratio as a screening tool for obesity and cardiometabolic risk
Article information
Abstract
The waist-to-height ratio (WHtR), calculated by dividing the waist circumference (WC) by height, has recently gained attention as an anthropometric index for central adiposity. It is an easy-to-use and less age-dependent index to identify individuals with increased cardiometabolic risk. A WHtR cutoff of 0.5 can be used in different sex and ethnic groups and is generally accepted as a universal cutoff for central obesity in children (aged ≥6 years) and adults. However, the WHtR has not been validated in preschool children, and the routine use of WHtR in children under age 6 is not recommended. Prospective studies and meta-analysis in adults revealed that the WHtR is equivalent to or slightly better than WC and superior to body mass index (BMI) in predicting higher cardiometabolic risk. In children and adolescents, studies have shown that the WHtR is similar to both BMI and WC in identifying those at an increased cardiometabolic risk. Additional use of WHtR with BMI or WC may be helpful because WHtR considers both height and central obesity. WHtR may be preferred because of its simplicity and because it does not require sex- and age-dependent cutoffs; additionally, the simple message 'keep your WC to less than half your height' may be particularly useful. This review article summarizes recent publications on the usefulness of using WHtR especially when compared to BMI and WC as a screening tool for obesity and related cardiometabolic risks, and recommends the use of WHtR in clinical practice for obesity screening in children and adolescents.
Introduction
Obesity results from a chronic imbalance between caloric intake and energy expenditure1). The prevalence of obesity has been increasing worldwide for the past 30 years, possibly because of increased caloric intake and decreased physical activity2). The increasing prevalence of pediatric obesity may be problematic because not only it increases the prevalence of, but also it can advance the age of onset of obesity-related chronic diseases such as type 2 diabetes and cardiovascular diseases34). According to the results of a cohort study in American Indians, the death rate before age 55 years from endogenous causes among children in the highest quartile of body mass index (BMI) was more than double that among children in the lowest BMI quartile5).
As the prevention and early detection of childhood obesity is critically important for public health, pediatricians should pay attention to changes of adiposity indices in children and alert parents before the onset of obesity-related medical problems. BMI and waist circumference (WC) are commonly used parameters to define obesity and central adiposity. The threshold for increased cardiometabolic risks can differ according to gender and ethnicity, and lower BMI cutoffs are used for Asians, and the use of ethnicity and sex-specific WC cutoffs are recommended67). Both BMI and WC are highly age-dependent in children and adolescents, and clinicians must refer to tables to determine gender- and age-dependent cutoffs8). However, it is inconvenient to use tables for each patient in busy outpatient clinic settings, indicating the need for an adiposity index that is reliable but easier to use.
The waist-to-height ratio (WHtR), calculated by dividing WC by height, has recently gained attention as an anthropometric index for measuring central adiposity. WHtR is a more sensitive universal screening tool than BMI to detect health risks and is cheaper and easier to use910). It was suggested that a WHtR cutoff of 0.5 can be used in different sex and ethnic groups and that the same cutoff can be applied in children and adults11). The message 'keep your WC to less than half your height' may be particularly useful for public health as well as in clinical settings12).
This review article summarizes recent publications related to the usefulness of WHtR compared to that of BMI and WC, as a screening tool for obesity and related cardiovascular and metabolic risks, and recommends the use of WHtR in clinical practice for screening obesity in children and adolescents.
Limitations of currently used measures of adiposity
1. Body mass index
Age- and sex-specific BMI percentiles have been used in the standard definition for child overweight and obesity worldwide13). However, BMI alone cannot distinguish individuals with excess body fat from those with high muscle mass and cannot reflect fat distribution14). Although BMI generally correlates well with other measures of adiposity and cardiometabolic risks, indices of abdominal obesity have been reported as better discriminators of cardiovascular risk factors, and the WC is used in the current definition of metabolic syndrome71516). According to a large European prospective study that reported nearly 15,000 deaths among more than 350,000 subjects, WC was strongly associated with the risk of death after adjusting for BMI17). The additional use of WHtR can be helpful when screening for obesity based on BMI in adolescents, as WHtR represents central adiposity. In our recent study, among adolescents with BMI ≥85th percentile, metabolic syndrome was more common in those with a WHtR≥0.5 than in those with a WHtR<0.518).
2. Waist circumference
Although the WC is an excellent index for measuring central adiposity, tables for age- and sex-dependent WC cutoffs are required in children and adolescents716). An advantage of WHtR is that a single cutoff can be used and it does not require age-dependent cutoffs1119).
WC is a height-dependent variable, and taller children generally have a larger WC than shorter children. However, height is not taken into account when obesity is defined based on age-dependent WC percentiles10). The degree of central adiposity can be overestimated in tall children, whereas it can be underestimated in short children if it is defined only by age-dependent WC cutoffs11). Approximately 3% of adolescents with WC <90th percentile had a WHtR of ≥0.5 and were significantly shorter compared to their low-WHtR counterparts, and the prevalence of multiple cardiometabolic risk factors was significantly higher in the WC <90th percentile/WHtR ≥0.5 group compared to that in the WC <90th percentile/WHtR <0.5 group in our recent study18). In addition, 16.7% of adolescents with a WC ≥90th percentile had a WHtR of <0.5 and were significantly taller compared to their high-WHtR counterparts, and the prevalence of metabolic syndrome was 7.4% in adolescents with WHtR <0.5 and 19.4% in those with WHtR ≥0.5 among those with a WC ≥90th percentile18). Because the WHtR is adjusted for height, it appears to be useful for identifying individuals with cardiometabolic risk, even when used in combination with WC.
Moreover, the cardiometabolic risk may differ between people with the same WC but different heights. It was reported that taller populations have lower mortality from ischemic heart disease and stroke20), whereas shorter people have higher metabolic risk than taller people with the same WC21). Schneider et al.22) reported that short subjects were at a higher risk and had a 30% higher prevalence of metabolic syndrome than tall subjects when grouped by WC and not by WHtR, and suggested that WHtR rather than WC should be included in the definition of metabolic syndrome. Both height and central adiposity should be considered when identifying individuals at higher metabolic risk, and the WHtR appears to be the best alternative tool.
Correlation between WHtR and other adiposity indices
The agreement between WC and WHtR was good in United States (US) children aged 6 years or older23). WHtR showed a high degree of concordance with percent body fat (calculated from measurements of skin fold thickness) in 6- to 14-year-old Spanish children24). The WHtR showed better results than WC and BMI (64% vs. 31% and 32%) for predicting percent body fat, measured by dual energy X-ray absorptiometry, in US children and adolescents aged 8–18 years25). However, a recent systemic review comparing measures of body fat in 7- to 10-year-old children reported that BMI and WC were strongly correlated with body fat as measured by bioelectrical impedance or skinfolds, whereas the WHtR showed a moderate positive correlation between body fat estimated by air-displacement plethymography26).
Validity of WHtR for predicting cardiometabolic risks
1. Studies in adults
According to a meta-analysis by Lee et al.15) which included more than 88,000 adults mainly from Asian countries, WHtR was the best discriminator for hypertension, diabetes, and dyslipidemia in both sexes, whereas BMI was the poorest discriminator for cardiovascular risk factors. In another meta-analysis including more than 300,000 adults, the WHtR was superior compared to BMI and WC in identifying adults with cardiometabolic risks; WC improved the discrimination of adverse outcomes by 3% and WHtR improved discrimination by 4%–5% compared to that by BMI11).
In a study of Korean adults based on the ‘Korea National Health and Nutrition Examination Survey (KNHANES)’ 2008–2011, WHtR showed better performance than BMI in predicting the presence of metabolic syndrome27). Kim et al.28) reported that the area under the curve of WHtR was the highest, followed by WC and BMI, in identifying Korean adults with a 10-year Framingham coronary heart disease risk score of 20% or more, and they suggested the clinical use of WHtR as a marker for obesity.
A prospective study of body size and risk of stroke among more than 45,000 women below age 60 years showed that measures of abdominal obesity (WHtR>WC) were strong predictors of stroke in the 11 years of follow-up, whereas BMI was not significantly associated with stroke29). In a prospective study of German adults followed up for 5–12 years, stronger associations were found between measures of abdominal obesity (such as WC and WHtR) and incident type 2 diabetes mellitus (DM) compared to that with BMI, and WHtR was the strongest predictor for the development of type 2 DM30). According to a study in which more than 16,000 male subjects were followed for 14 years and 32,000 female subjects for 5.5 years, WHtR showed the strongest association with cardiovascular disease compared with that by BMI and WC, although the differences were small and likely not clinically important31).
2. Studies in children and adolescents
WHtR and BMI showed equivalent results in identifying high blood pressure (BP) in German adolescents18), and BMI-for-age and WHtR showed similar ability in identifying US children aged 5–17 years with cardiovascular risk factors32). The WHtR and WC percentiles performed similarly to BMI percentile for discriminating elevated insulin and the clustering of risk factors in the HEALTHY study33). In 6- to 10-year-old children in Brazil, WHtR and BMI area under the curve (AUC) were similar for all cardiometabolic parameters34), suggesting that WHtR has advantages such as its simplicity, although it may not be superior in discriminating higher metabolic risk in children and adolescents.
Both WC (>90th percentile) and WHtR (>0.5) were used to identify higher metabolic risk among 5- to 15-year-old overweight children classified using International Obesity Task Force BMI cutoffs35). According to a study in which overweight and obese children categorized based on the BMI percentiles were further stratified by WHtR, overweight and obese children with a WHtR <0.5 had a cardiometabolic risk approaching that of subjects in a normal BMI percentile category36). An increased WHtR was significantly associated with an increased cardiometabolic risk, even in overweight and obese children, and the authors suggested that WHtR should be included in the routine screening and assessment of overweight and obese children36).
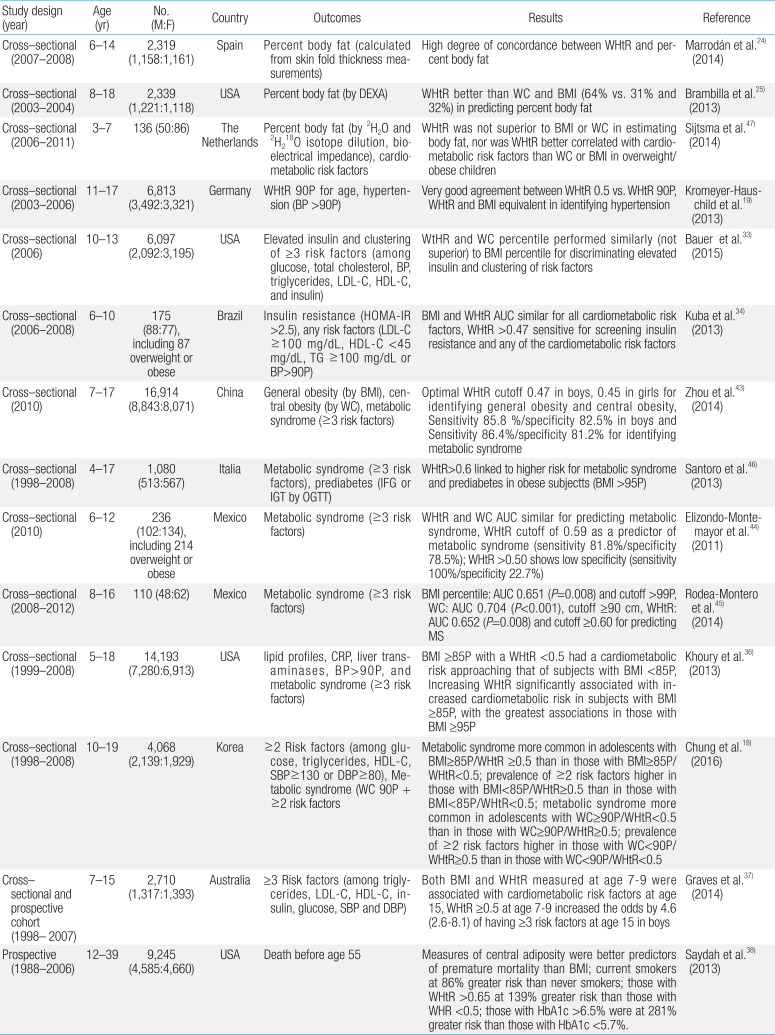
Prospective studies are important, but enormous efforts are required to perform long-term prospective studies in children and adolescents, and thus few of these studies have been conducted. In an Australian cohort study, both BMI and WHtR measured during childhood were associated with cardiometabolic risk factors in adolescents, and a WHtR≥0.5 at 7–9 years increased the odds of having ≥3 cardiometabolic risk factors in boys by 4.6 (2.6–8.1)37). In a prospective study in the US, measures of central adiposity were better predictors of premature mortality than BMI, and those with a WHtR>0.65 aged 12–39 years were at a 139% greater risk of death before age 55 years compared to those with a WHtR<0.538). These findings underscore the importance of obesity control in youths, particularly the early detection and intervention for those with central obesity. Recent publications the validity of WHtR in children and adolescents are summarized in Table 1.
Optimal WHtR cutoff
1. Optimal cutoff in adults
According to a systemic review, the mean boundary values for WHtR covering all cardiometabolic outcomes from studies in 14 different countries and including Caucasian, Asian, and Central American subjects were 0.5 for both men and women39). In a recent study of Chinese adults, the optimal WHtR cutoff for the CVD cluster was 0.5; the upper boundary values of WHtR for detecting the risk factor cluster with specificity above 90% were 0.55 and 0.58 for men and women, respectively40). In a recent study based on KNHANES 2007–2010, the optimal WHtR cutoff points for identifying those with high coronary heart disease risk were 0.50 and 0.52 in Korean men and women, respectively28).
2. Optimal cutoff in children
A WHtR cutoff of 0.5 has been suggested as a universal cutoff in children as well as in adults10). Although it seems that the WHtR is less dependent on age and sex, small variance may present according to ethnic backgrounds. According to a study in New Zealand children aged 5–14 years, although a WHtR>0.5 was more common in Pacific and Maori children than in those of other ethnicities and ethnicity influenced the relationship between BMI and WHtR, the differences were clinically insignificant and WHtR values for a given BMI were similar (WHtR of 0.47 in Maori, 0.46 in Pacific, and 0.48 in European boys at the 85th percentile)41).
The WHtR cutoff of 0.5 showed very good agreement with age- and sex-specific WHtR 90th percentiles in German adolescents18). However, sex- and ethnicity-specific WHtR cutoff values may improve sensitivity and specificity for identifying those at higher metabolic risk. In Korean children aged 6–18 years, the WHtR cutoffs for overweight (85th percentile≤BMI<95th percentile) were 0.48 in boys and 0.47 in girls and those for obesity (BMI≥95 percentile) were 0.51 in boys and 0.49 in girls42). In Chinese children aged 7–17 years, the optimal WHtR cutoffs for identifying those with general and central obesity were 0.47 in boys and 0.45 in girls43).
Different criteria and study methods may also increase the variance in optimal cutoffs between studies, and caution should be used when interpreting different study results. A WHtR cutoff of >0.47 was sensitive for screening insulin resistance (Homeostatic Model of Assessment-Insulin Resistance>2.5) and any cardiometabolic risk factors (low density lipoprotein-cholesterol≥ 100 mg/dL, high density lipoprotein [HDL]-cholesterol<45 mg/dL, triglycerides≥100 mg/dL, or BP>90th percentile) in 6- to 10-year-old Brazilian children34), whereas a WHtR cutoff of 0.59 was suggested as a predictor of metabolic syndrome (≥3 risk factors among WC≥90th percentile, glucose≥110 mg/dL, HDL-cholesterol <40 mg/dL, triglycerides≥110 mg/dL, or systolic or diastolic BP≥90th percentile) in 6- to 12-year-old Mexican children44).
Thus, a higher WHtR cutoff (0.6 or 0.65) may be useful in high-risk populations to identify individuals with even higher cardiometabolic risk363845). A WHtR>0.6 was linked to a higher risk of metabolic syndrome and prediabetes among obese Italian children and adolescents46), and those with WHtR>0.65 at age 12–39 years were at a 139% greater risk of death before age 55 years than those with a WHR<0.538).
Limitations and controversies
1. Use of WHtR in infants and preschool children
The relationship between WHtR and other obesity indices or cardiometabolic risk factors in younger children have not been validated, and the routine use of WHtR in children under age 6 years cannot be recommended. The agreement between the WC 90th percentile versus WHtR cutoff of 0.5 was poor for 2- to 5-year-olds in the US, and a WHtR cutoff of 0.5 may overestimate central obesity in very young children23). WHtR significantly decreased with age in Korean children, and values were more age-dependent in the 2- to 5-year-old age group42). In Dutch children aged 3–7 years, WHtR was not superior compared to BMI or WC in estimating body fat; the correlation of WHtR with cardiometabolic risk factors was not better than that of WC or BMI in overweight/obese children47).
2. Methodology for WC measurements
It was reported that the reliability of WC measurement is lower than that of weight and height measurement, and WC showed significant interobserver differences48). It is essential to standardize the methodology in order to decrease measurement error, and acceptable intra- and interobserver agreement can be achieved by training the participating staff49).
Different techniques for conducting WC measurements may result in different WC and WHtR values. WC should be measured using plastic or metal tape in the standing position over bare skin or light undergarments. It is most commonly measured at the narrowest part of the trunk, but can be measured at the midpoint, umbilicus, or iliac crest level. A systematic review of 120 studies suggested that the WC measurement protocol has no substantial influence on the association between mortality, CVD, and diabetes50).
Conclusions
WHtR is a reliable, easy-to-use, and less age-dependent index for identifying children and adolescents with increased cardiometabolic risk related to central adiposity. A WHtR cutoff of 0.5 is generally accepted as a universal cutoff for central obesity in children aged ≥6 years as well as in adults. However, the WHtR has not been validated in infants and preschool children. Even in older children, sex- and ethnicity-specific WHtR cutoffs may improve sensitivity and specificity for identifying those at higher metabolic risk. The additional use of WHtR with BMI or WC also appears to be helpful for screening those with higher cardiometabolic risk. Most recent studies now include the WHtR as a major adiposity index, regarding it as a validated and universal index of central adiposity515253).
Prospective studies and meta-analyses of adults have revealed that the WHtR is equivalent to or slightly better than WC and superior to BMI in predicting higher cardiometabolic risk. Studies in children and adolescents showed that WHtR is similar to both BMI and WC for identifying those with increased cardiometabolic risk. Additional large-scale prospective studies are needed to confirm the usefulness of WHtR for predicting comorbidities of obesity in children and adolescents.
Notes
Conflicts of interest: No potential conflict of interest relevant to this article was reported.