Analysis of clinical characteristics and causes of chest pain in children and adolescents
Article information
Abstract
Purpose
Chest pain is common in children and adolescents and is a reason for referral to pediatric cardiologists. Although most cases of chest pain in these age groups are benign and do not require treatment, timely diagnosis is important not to miss life-threatening diseases requiring prompt treatment. We investigated certain clinical characteristics that may be useful in the diagnosis of such critical diseases.
Methods
Patient medical records between July 2006 and September 2013 were retrospectively examined. We included 517 patients who presented with chest pain to the Department of Pediatrics at Kyung Hee University Hospital in Gangdong.
Results
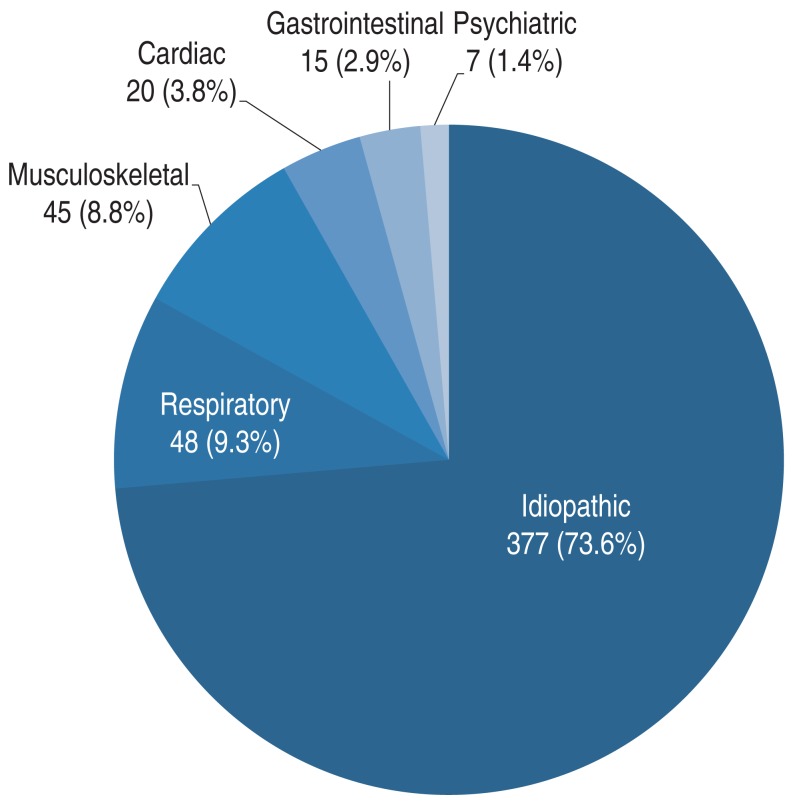
Most cases of chest pain were idiopathic in origin (73.6%), followed by cases with respiratory (9.3%), musculoskeletal (8.8%), cardiac (3.8%), gastrointestinal (2.9%), and psychiatric (1.4%) causes. In 6 patients (1.2%) with air-leak syndrome including pneumothorax or pneumomediastinum, the pain was abrupt, continuous, and lasted for a short period of 1-2 days after onset in the older adolescents. Of the patients with cardiac pain, 13 had cardiac arrhythmias (65.0%), 6 had congenital heart diseases (30%), and 1 had coronary aneurysms caused by Kawasaki disease (5.0%). One patient with atrial flutter had only symptoms of syncope and chest pain.
Conclusion
The abrupt, continuous chest pain of a short duration in the older children was characteristic of air-leak syndrome. In patients with pneumomediastinum, radiological diagnosis was difficult without careful examination. Combined syncope should not be neglected and further cardiac workup is essential in such patients.
Introduction
Chest pain is a common symptom that results in visits to the Emergency Department or outpatient pediatric clinics12). After cardiac murmurs, this is the second most common symptom that is referred to pediatric cardiologists. When chest pain occurs, family members become worried because of the fear of cardiac disease. However, serious illnesses such as severe coronary ischemia appear rarely in children and adolescents345). The main causes of chest pain are idiopathic and musculoskeletal diseases; therefore, most patients with chest pain do not require any special treatment678910). Moreover, patients who show symptoms of chest pain may not need to undergo all available tests, including echocardiography. However, for patients with a serious disease that requires rapid diagnosis and treatment, failure to perform a timely diagnose may result in fatalities. Careful examination of medical history, performance of relevant medical tests, and physical examination are required in order to diagnose such diseases. Here, we intended to discover clinical characteristics that may be useful in the diagnosis of some critical diseases that may manifest as chest pain in children and adolescents.
Materials and methods
We retrospectively reviewed medical records from July 2006 to September 2013. Subjects were comprised of 517 children with chest pain who visited Kyung Hee University Hospital at Gangdong. By conducting systematic interviews, we reviewed the patients' medical history, age, sex, height, weight, and family history, as well as the chest pain characteristics, symptom duration, associated symptoms, and time from the onset of symptoms to visiting the hospital. We also noted the presence or absence of chest wall tenderness, heart abnormalities, and lung sounds. Laboratory tests, including chest radiography, electrocardiography (ECG), echocardiography, blood examinations, and 24-hour Holter monitoring, were performed as indicated. Finally, the final diagnosis and method of treatment were investigated. We categorized chest pain as "musculoskeletal" origin when the patient had physical findings of chest wall tenderness, pain aggravated with inspiration, muscle strain or pain that is reproducible with movement, and tenderness on palpation of costochondral junctions. Chest pain of "respiratory" origin was categorized based on chest radiography of lung lesion or chest pain secondary to acute onset of cough or asthma with recent wheezing. When the chest pain was associated with indigestion, heartburn, and vomiting or when patients were diagnosed as gastroesophageal reflux or gastritis in gastroscopy, it was categorized as "gastrointestinal". We categorized chest pain as "cardiac" origin in patients with congenital heart disease, Kawasaki disease or arrhythmias. Although patients with chest pain had cardiac disease, we categorized this group of patients as other causes such as "idiopathic" of "musculoskeletal" origin in cases that we thought the pain was not originated from cardiac diseases per se. Though laboratory findings including ECG, echocardiography, chest radiography were normal in patients with cardiac diseases when they visited a pediatrician, we categorized these patients as "cardiac" origin if we could not find other causes of chest pain. When there were clear emotional or psychological causes including school problems, family troubles such as parents' divorce without contributing organic causes, it was categorized as "psychogenic". Patients without any organic etiology or any psychological factors were caterorized as "idiopathic".
Results
1. Demographic data
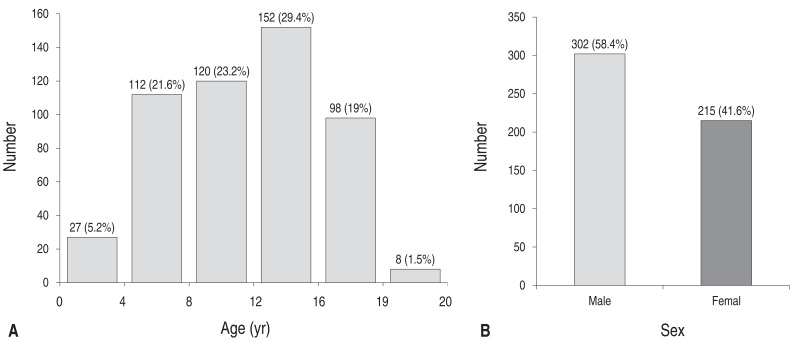
The patients' ages ranged from 2 to 19 years (mean, 9.6±4.6 years) (Fig. 1). We investigated 517 subjects who were divided into groups according to 1-year age intervals. The 15- to 16-year age group was the most common and consisted of 44 patients (8.5%). Meanwhile, the 19-year or older age group was the least common and consisted of 8 patients (5%). In sex distribution, of the 517 patients, 302 were male (58.4%) and 215 were female (41.6%).
Data showed that the body-weight distribution was between 11.5 and 93 kg (mean, 38±34.1 kg). Most of the patients (202, 41.8%) weighed between 10 and 30 kg.
2. Chest pain characteristics
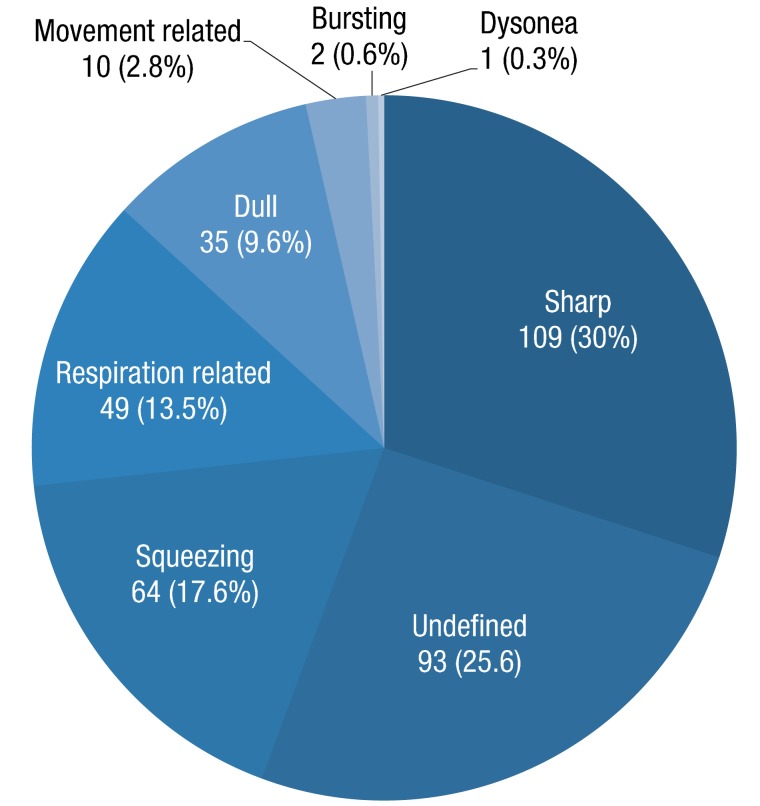
We investigated the chest pain characteristics in 363 subjects (70%) (Fig. 2). Sharp pain was the most common and was present in 109 patients (30%). Chest pain was not clearly identified in 93 cases (25.6%). The other characteristics were described as squeezing (64 patients, 17.6%), respiratory-related (49 patients, 13.5%), and dull aches (35 patients, 9.6%). Chest pain associated with exercise was observed in 10 patients (2.8%), and bursts of sensation were noted in 2 patients (0.6%).
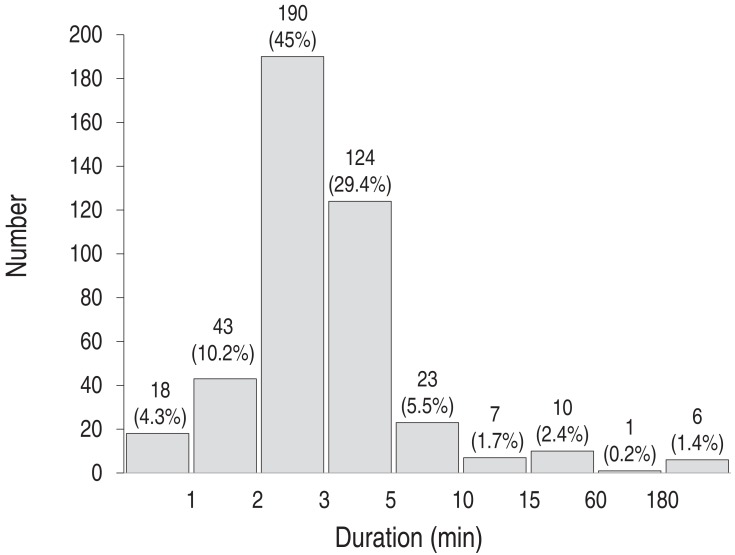
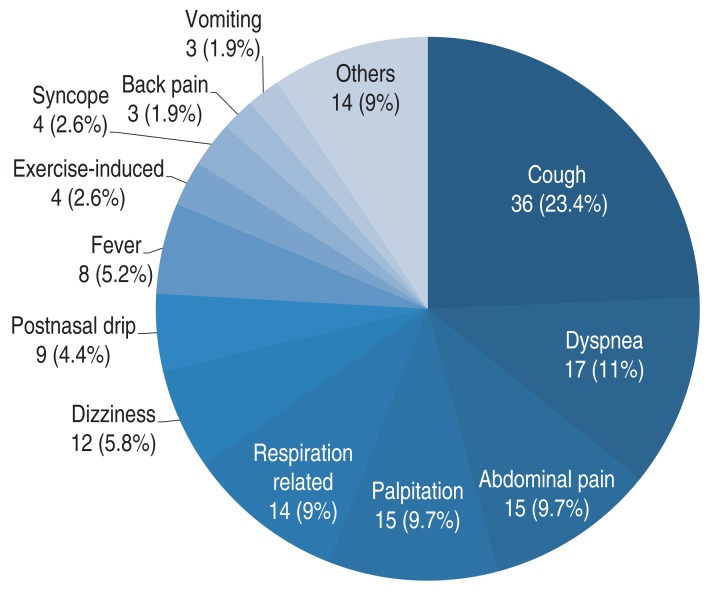
Symptom duration was investigated in 422 patients (81.6%). Symptoms lasted 2-3 minutes in 190 patients (45%) and 3-5 minutes in 124 patients (29.8%) (Fig. 3). Chest pain with associated symptoms occurred in 154 patients (30%). Cough, which appeared in 36 cases (23.4%), was the most common symptom (Fig. 4), followed by dyspnea (17, 11%), abdominal pain (15, 9.7%), palpitations (15, 9.7%), respiratory problems (14, 9%), dizziness (12, 5.8%), and postnasal drip (9, 4.4%). Syncope (4, 2.6%) and back pain (3, 1.9%) also occurred. The other symptoms mentioned were fatigue, frequent urination, anxiety, cyanosis, seizure, and hyperventilation. Associated symptoms occurred either solely or with overlaps of more than one symptom.
Time from onset to visit to a hospital was investigated in 282 patients (55%) (Fig. 5); it ranged from 1 day to 6 years. Of the 282 patients, 131 visited within 10 days (46%) and almost all individuals (266, 94%) visited within a year.
3. Diagnosis and treatment of chest pain
The most common causes of chest pain were idiopathic, which accounted for 377 cases (73.6%) (Fig. 6). Respiratory problems accounted for 48 cases (9.3%); and musculoskeletal problems, 45 cases (8.8%). Cardiac problems accounted for 20 cases (3.8%). In addition, gastrointestinal origins accounted for 15 cases (2.9%); and psychiatric problems, 7 cases (1.4%).
1) Idiopathic
Idiopathic problems, which were the most common cause of chest pain, accounted for 377 cases (73.6%). Many of these were attributed to musculoskeletal disorders. Duration of chest pain was 2-3 minutes on average and evaluation of chest pain including chest radiography, ECG was normal. The symptom improved without any treatments.
2) Musculoskeletal origins
Chest pain caused by musculoskeletal problems accounted for 43 cases (8.9%). In 12 cases, chest wall tenderness was observed. Osteomyelitis of the sternum was diagnosed in 1 patient. The symptoms of the children in these cases improved naturally after follow-up or with the use of nonsteroidal anti-inflammatory drugs (NSAIDs) or use of antibiotics when necessary. Idiopathic, which were the most common cause of chest pain, accounted for 72.9% of the cases. Many of the cases were attributed to musculoskeletal disorders.
3) Respiratory diseases
Chest pain due to respiratory diseases was present in 48 patients (9.3%). Asthma was observed in 8 patients; acute bronchitis, in 21 patients; and pneumonia, in 13 patients. Pneumomediastinum and pneumothorax were found in 6 patients (12.5%). These diseases demonstrated characteristics of persistent pain for 1 to 2 days in 15- to 17-year-old male patients. All the patients with pneumothorax were diagnosed using chest radiography. In the patient with pneumomediastinum, whose chest radiographic findings were vague, chest computed tomography (CT) confirmed the diagnosis. All the 5 patients who were diagnosed with pneumothorax had a chest tube inserted, and the patient with pneumomediastinum improved spontaneously after follow-up.
4) Cardiac origins
Chest pain caused by heart problems accounted for 20 cases (3.8%), indicating a relatively low incidence. Among the 20 cases, 6 were congenital heart diseases, including 3 cases of large atrial septal defect (ASD), 1 case of pulmonary artery stenosis with ventricular septal defect (VSD), 1 case of aortic arch anomaly, and 1 case of large patent ductus arteriosus (PDA) with Eisenmenger syndrome. Two cases of pulmonary valve stenosis and two cases of VSD were classified as "idiopathic".
Arrhythmia was found in 13 patients, of whom 6 had paroxysmal supraventricular tachycardia and 3 had ventricular premature contraction. A 4-year-old female patient with atrial flutter presented with symptoms of syncope and chest pain only. After ECG diagnosis of the atrial flutter, treatment with adenosine, amiodarone, and direct current cardioversion were performed. In addition, Mobitz type II block, atrial premature contraction, second-degree atrioventricular block, and atrial paroxysmal tachycardia were found in 1 patient, respectively. Meanwhile, coronary aneurysm caused by Kawasaki disease was observed in 1 patient. In the 20 patients with heart disease, the chest pain was believed to be associated with chest wall origin or idiopathic causes rather than the heart problem itself in 4 patients who are classified as idiopathic cause.
5) Miscellaneous
Fifteen cases (2.9%) with chest pain were due to gastrointestinal origin. In detail, it was determined as gastritis in 8 cases, gastroesophageal reflux in 5 cases, and acute gastroenteritis and dyspepsia in 1 case. Psychiatric problems can also cause chest pain. We observed 7 cases caused by psychiatric problems, of which 4 were attributed to anxiety disorder and 3 were attributed to panic disorder.
Discussion
Pediatric and adolescent chest pains were found to be mostly due to noncardiac diseases. Idiopathic (73.6%) was the most common cause of chest pain in this study. This was followed by respiratory (9.3%), musculoskeletal (8.8%). gastrointestinal (2.9%), and psychiatric problems (1.4%). Cardiac problems accounted for only 3.8% of the cases. These results were similar to the results of previous studies678910).
In this study, we would like to emphasize a careful diagnostic approach for chest pain. We categorized "idiopathic" chest pain as having an unknown origin or normal test results for chest pain, including physical examination, chest radiography, ECG, echocardiography, and 24-hour Holter monitoring when necessary. The term "idiopathic" is essentially used when symptoms improve or resolve within 1 year after the occurrence of chest pain411). The mean chest pain duration was 2-3 minutes, and the symptoms improved by the use of analgesics such as NSAIDs or sometimes even with mere follow-up. NSAIDs were generally given on a weekly basis, and their doses were reduced as symptoms improved. In the case of idiopathic chest pain, control of symptoms was sufficient treatment.
Most cases of musculoskeletal chest pain were associated with difficulties in breathing and movement (14 cases, 30%). In some cases, idiopathic chest pain was also associated with difficulties in breathing (51 cases, 14%). It is difficult to accurately distinguish between idiopathic and musculoskeletal chest pains. In the 2 types of pain, the symptoms may overlap and the features of idiopathic and musculoskeletal chest pains are very similar. Sharp pain was present in 62 cases (17%) of idiopathic chest pain and 13 cases (28%) of musculoskeletal chest pain. Symptom duration was 2-4 minutes for idiopathic chest pain and 2-3 minutes for musculoskeletal chest pain.
Many children with musculoskeletal chest pain experienced tenderness upon physical examination (16 cases, 34%). In 23 cases (49%), pain was felt in the anterior chest, and 9 cases (19%) were diagnosed as costochondritis. Most cases of idiopathic chest pain were attributed to problems of the musculoskeletal system. Although idiopathic or musculoskeletal chest pain occurs temporarily and improves even without specific treatment, follow-up is necessary at a later date.
In previous study, asthma and pneumonia are common diseases accompanied by chest pain (17%)12). In our study, asthma also was accounted for a large portion (16.7%) of the respiratory problems. Therefore, a detailed medical history report is necessary for differentiation from other diseases13). Intravenous or oral antibiotics were used for the treatment of respiratory diseases, and chest pain dissipated after recovery. Generally, a bronchodilator was used for symptom improvement. Bronchodilators could help in the diagnosis of respiratory diseases if it is found to be effective for symptom relief12).
Pneumomediastinum or pneumothorax occurred in 6 of the 48 patients (12.5%) with respiratory diseases (1.2% as a whole). In this study, all the patients with pneumothorax received a chest tube insertion as soon as diagnosed. Accurate and immediate diagnosis is the first step in an appropriate treatment, the prevention of complications, and good prognosis. Tachycardia with pleuritic chest pain was demonstrated on physical examination in pneumothorax patients. Dyspnea also occurred with more severe pneumothorax14). If these symptoms are seen in a patient with chest pain, clinicians should consider an air-leak syndrome such as pneumothorax. Pain occurs suddenly and constantly in air-leak syndromes and runs a short course of 1-2 days in older children and adolescents. Air-leak syndromes, including pneumothorax and pneumomediastinum, are diagnosed using radiological investigation1415). In patients with pneumomediastinum, the lesions are easily missed on chest radiology without careful assessment. In our study, the chest radiological findings were vague, and chest CT was needed to confirm the diagnosis. Therefore, it is necessary to pay attention to the radiological findings in patients before performing echocardiography when symptoms are suspected to be due to air-leak syndrome.
In this study, as in previous studies, the patients with chest pain due to cardiac diseases comprised only a small percentage (3.8%). In the patients with chest pain associated with congenital heart diseases (6/20 cases, 30.0%), the data showed various heart diseases such as large ASD, VSD, pulmonary valve stenosis, VSD with pulmonary artery stenosis, aortic arch anomaly, and large PDA with Eisenmenger syndrome. However, these diseases were diagnosed before the chest pain occurred. When the chest pain occurred, the findings in the examinations such as chest radiography, laboratory work, and ECG were nonspecific. One patient with large, 2-hole secundum ASD who had received a percutaneous ASD device closure in the previous year revisited the hospital because of chest pain, but his chest radiography, echocardiography, and ECG showed nonspecific findings.
Among the patients who were diagnosed with arrhythmia previously, sinus rhythms were found in many of the patients during the chest pain evaluation when they were referred to a pediatric cardiologist. Therefore, the origin of pain could not likely be directly associated with cardiac diseases even in the patients who previously had cardiac diseases. One case of heart disease was diagnosed as an atrial flutter, and this was accompanied by chest pain and syncope. As described in other studies, chest pain with syncope may have been indicative of a heart disease131617). In general, chest pain and other systemic symptoms are considered independently. In the diagnoses of chest pain, associated symptoms could be informative in identifying the origin of the chest pain. Therefore, medical staff should not overlook related symptoms and must recognize that they can be signs of a more severe underlying disease that requires further evaluation at a later date13161718).
In the patient in this study who had a coronary aneurysm due to Kawasaki disease, the chest pain was caused by Kawasaki disease per se and did not originate from cardiac ischemia. All the cardiac problems were caused by an underlying disease. The chest pain characteristics and laboratory findings showed that the chest pain was not caused by a heart disease. Severe cardiac disease is rare in pediatric patients with complaints of chest pain678910141516171920).
Regurgitation and dyspepsia were associated with gastroesophageal reflux1920). Referral pain from the upper gastric tract to the chest also occurred in cases of chest pain with gastrointestinal problems2122). Chest pain is usually elicited by diet22). For the evaluation of chest pain due to gastrointestinal diseases, knowing these characteristics is useful in diagnosis. Gastritis or gastroesophageal reflux was diagnosed based on clinical symptoms and imaging studies such as an endoscopy or upper gastrointestinal series23). After treatment with NSAIDs and proton pump inhibitors, symptoms improved upon follow-up.
Psychiatric problem in the chest pain was often associated with dyspnea (3 cases, 50%) or hyperventilation in panic disorder (3 cases, 50%). Hyperventilation is a common sign of a mood disorder24). Most subjects (4 cases, 67%) described their chest pain as a squeezing sensation. The results of examinations of chest pain (ECG, chest radiography, blood examination, physical examination, and echocardiography) were normal. Symptoms were revealed by evaluating the mood of the individual due to circumstances and their environment25). Problems included circumstances such as school maladjustment (2 cases, 29%) and family issues such as divorce (2 cases, 29%) at the time the chest pain occurred. Life events such as these can be stressful and may induce chest pain5). Chest pain induced by a psychiatric or mood disorder is sometimes confused with idiopathic chest pain, or they can occur simultaneously26).
Regarding study limitations, as a retrospective study, we were unable to perform uniform laboratory examinations in all the patients. A prospective study with a standardized assessment protocol may delineate more accurate clinical characteristics for diagnosis and management of pediatric chest pain. Moreover, the number of patients with chest pain with cardiac disease was rather small. A larger-scale study, including more patients with cardiac diseases, may be necessary for more-refined results.
In conclusion, although most chest pain cases in the pediatric and adolescent patients were benign, we found that it is important not to miss certain critical underlying diseases in such patients. An acute, continuous chest pain with a short duration of 1-2 days in older children was characteristic of an air-leak syndrome. Pneumomediastinum, in particular, is difficult to detect using radiological methods, unless the patient is suspected to have the disease. If the chest pain is combined with syncope, one should strongly suspect cardiac origins; therefore, meticulous medical examination should be performed.
Acknowledgments
This study was presented as oral abstract at the 63rd Annual Meeting of the Korean Pediatrics Society in Seoul, Korea.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.