Psychosocial adjustment and quality of life of adolescents and adults with congenital heart disease
Article information
Abstract
The incidence of people living with congenital heart disease (CHD) has been increasing every year owing to remarkable advances in surgical and catheter intervention techniques and devices, and improved knowledge of critical care for patients with CHD. However, these patients continue to face physical, psychosocial, and environmental challenges, and a number of studies have shown higher rates of depression and anxiety disorders than the general population. To improve psychosocial functioning and quality of life for adults with CHD, health care providers are recommended to inform CHD patients of an accurate diagnosis, and overall treatment process, beginning in adolescence to facilitate a smooth transition from adolescence to adulthood. Active cooperation with psychiatrists, psychologists, social workers, chaplains, and family members is highly recommended to help CHD patients feel normal and optimistic and to promote good social interactions, close family relationships, and a strong sense of coherence.
Introduction
The incidence of adults living with congenital heart disease (CHD) has been increasing every year due to remarkable advances in surgical and catheter interventional techniques and devices, and knowledge of critical care for patients with CHD1,2,3). However, the definition of a successful outcome of CHD treatment may vary. While clinicians traditionally considered a decrease in morbidity and mortality after treatment of CHD to be a successful outcome, patients may have a more stringent criterion for success.
Like other patients with chronic illness, adults with repaired or unrepaired CHD continue to face physical, psychosocial, and environmental challenges after successful treatment through surgical or catheter interventional treatment4,5). Although the assessment and measures for the improvement of quality of life (QoL) in adults with CHD are still unclear, clinicians should be more attentive to the importance of improving QoL, including psychosocial adjustment, for adolescents and adults with repaired or unrepaired CHD.
Changing profile of adults with CHD
Since the first surgical patent ductus arteriosus ligation in 1938 performed by Dr. Gross and the first open heart repair for a child with Tetralogy of Fallot in 1954 performed by Dr. Lillehei, most varieties of CHDs have been treated successfully by surgery or a catheter intervention1). The noticeable improvement of treatment for CHD and survival of patients with CHD over the last half century has given rise to a continuously increasing number of adults with CHD. Since the development of successful neonatal repair of complex lesions in the 1970s, an estimated 85%-90% of patients survive into adulthood compared with the 20% survival rate 50 years ago4,6). Considering the overall 1% prevalence of CHD in the live birth neonates and recent surgical mortality rates of less than 5% in the most developed countries, about 1 in 150 young adults would be expected to have a form of repaired or unrepaired CHD in the next decade in the developed countries3,6).
Although there is a lack of reliable data on the number of adults with CHD in South Korea, the pattern of increasing numbers of adults with CHD is comparable to most developed countries, because of the increase in number of surgeries for CHD since the late 1970s and the establishment of the Korean Heart Foundation7). Information from the database of the Korean Heart Foundation indicates that about 50,000 adults with CHD are estimated to currently live in South Korea, and more than 4,000 patients enter into adulthood annually (Fig. 1).
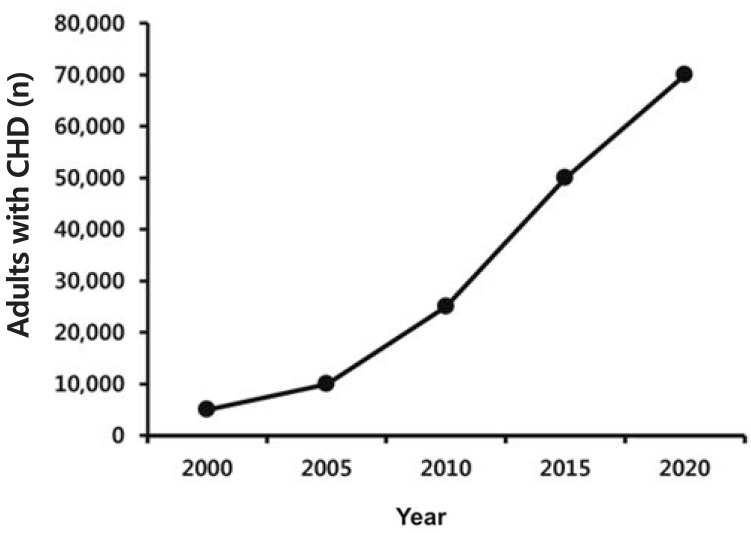
Adult congenital heart disease population in South Korea. From the database of the Korean Heart Foundation, we estimated that about 50,000 adults with congenital heart disease (CHD) live in South Korea and more than 4,000 patients newly enter adulthood every year. At the current rate, we will have about 70,000 by the year 2020.
The need for attention to the psychosocial function of adolescents and adults with CHD
Like other patients with chronic medical conditions, most adolescents and adults with repaired or unrepaired CHD continue to face life-long QoL challenges after successful surgical or catheter interventional treatment. Thus far, a widely accepted definition of QoL has not been established, and current definitions continue to vary from country to country. However, physical, psychosocial, and environmental aspects of life are very important and reasonable domains to assess the QoL of adults patients with CHD4).
In many studies, QoL was excellent and similar to an age- and gender-matched standard population in patients with simple CHDs such as atrial septal defect, ventricular septal defect, and coarctation of aorta4,8). However, many other patients with complex CHDs with or without arrhythmia, such as complete atrioventricular septal defect, Tetralogy of Fallot, and a single ventricle, showed a decrease in physical activities, which also affected physical functioning capacity, emotional well-being, and subsequently limited the patients' ability to conduct activities of daily living4,8,9,10).
Accumulation of medical costs due to repeated procedures and operations is a significant burden to adults with complex CHD and a life-long concern that contributes to psychosocial problems. When the cost of treatment for 55 years of Tetralogy of Fallot was measured in United Kingdom, the overall medical cost was estimated to be approximately 65,310 pounds (about 116,000,000 KRW; Korean Won, the currency of South Korea)11). Total medical costs may increase for adults with CHD as medical care improves in every developed country.
Adolescents and adults with CHD are prone to feel different from generally healthy people because of their various degrees of physical limitations and visible marks, such as surgical wounds. Although this feeling may be influenced by patients' environment, health care system, and personality, it is evident that patients struggle constantly to perceive themselves as normal compared to other healthy people12).
These distinct findings demonstrate that various degrees of decreased physical activity, life-long medical cost burden, and the feeling of being different from healthy people inevitably affect the psychosocial aspects of QoL, possibly contributing to depression and anxiety in adults with CHD. These impairments of psychosocial functions could affect the QoL of adolescents and adults with CHD when they are under great stress, such as adolescent developmental crisis, job-hunting, pregnancy, etc.13). With this in mind, the focus of this review is the means by which psychosocial adjustment can be used to improve the QoL of adolescents and adults with CHD.
Assessment of psychosocial function of adolescents and adults with CHD
Because knowledge about the psychosocial functioning of adolescents and adults with CHD is quite limited, there is no internationally standardized methodology to evaluate psychosocial adjustment in this group. Several measures that have been used for evaluation include TNO-AZL Questionnaire for Adult's Health-related Quality of Life14), Short Form-369), World Health Organization Quality of Life15,16), the Linear Analogue Scale17), and the Satisfaction With Life Scale17). However, these measures provide only a broad evaluation of overall QoL of the patient, and cannot be used for precise screening of mental health concerns, including depressive or anxiety disorders in adults with CHD.
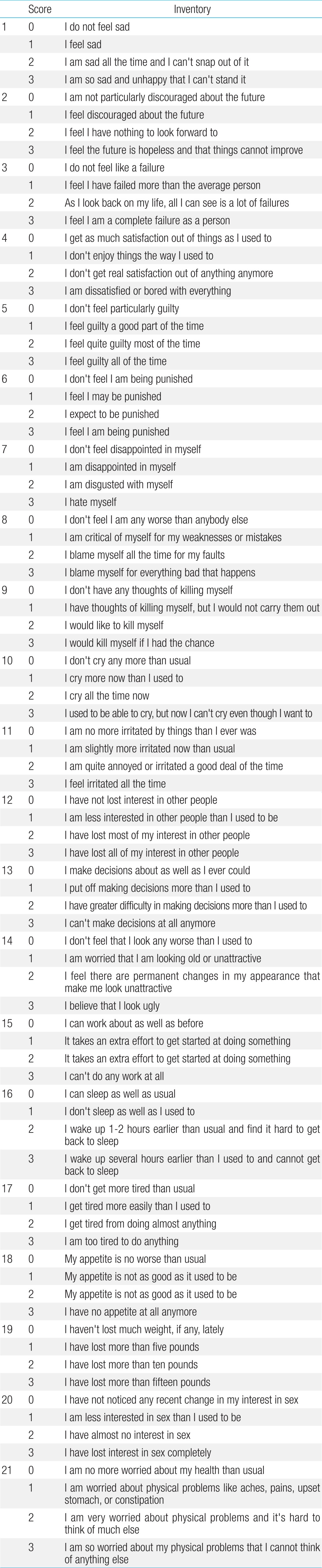
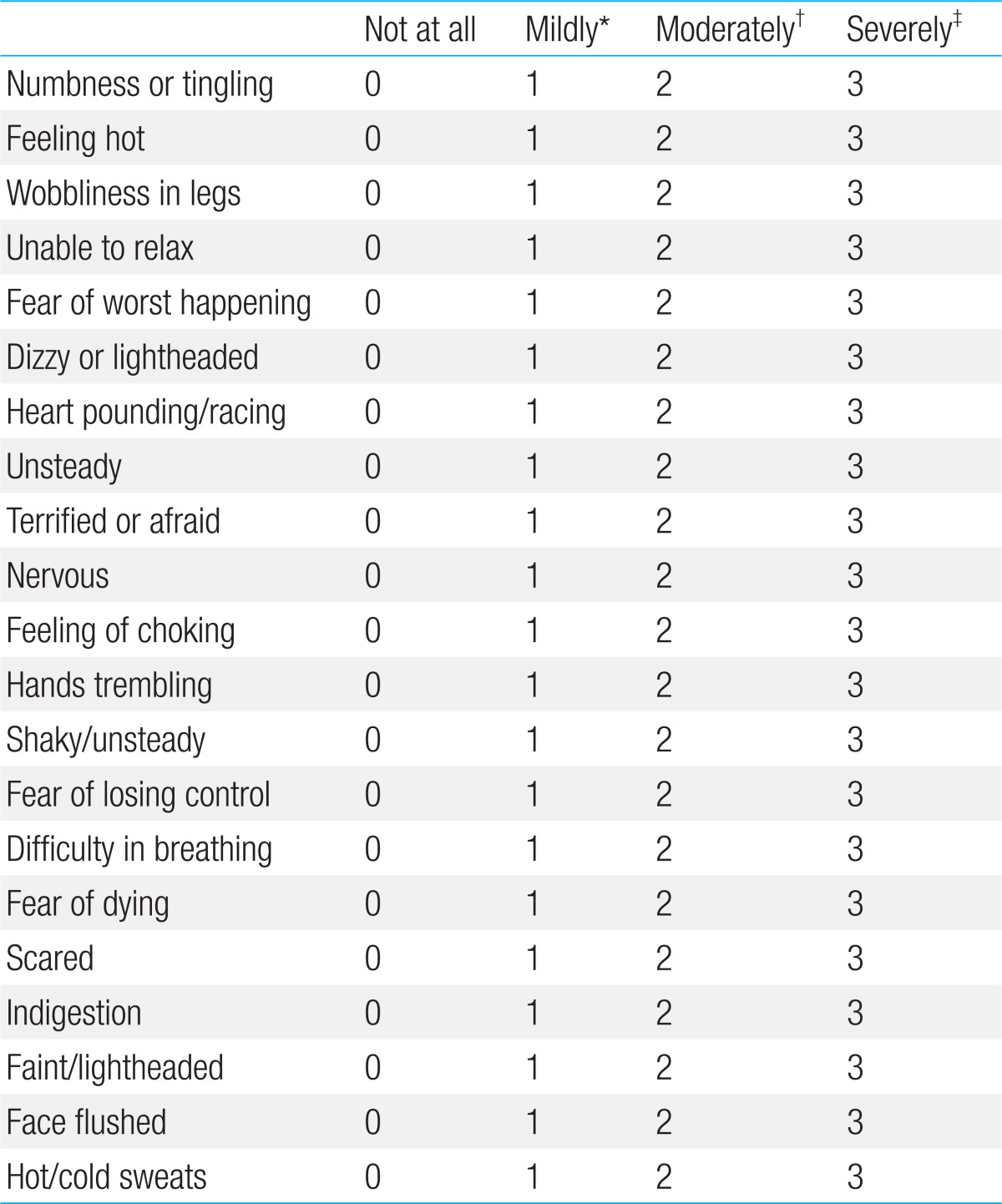
In this context, the Beck Depression Inventory (BDI) and the Beck Anxiety Inventory (BAI) can be good tools to screen for depressive or anxiety disorders in adults with CHD. The BDI is a 21-item self-administered questionnaire used to assess the severity of subjective depressive symptoms (Table 1)16,18). Each item is scored from 0 to 3 points (the total possible score ranges from 0 to 63; 0-9 indicates minimal depression with emotional changes that are considered normal; 10-18 indicates mild depression; 19-29 indicates moderate depression; and 30-63 indicates severe depression)18). The BAI is also a 21-item self-report questionnaire, and is used to assess the subjective feelings expressed as well-known symptoms of anxiety during the previous one week (Table 2)19). Each question has the same set of four possible answers and patients indicate how much they have been bothered by that symptom during the past week including the day of the survey (final scores are interpreted as 0-7, minimal level of anxiety; 8-15, mild anxiety; 16-25, moderate anxiety; and 26-63, severe anxiety)16,20). Women with anxiety disorders tend to score four points higher than men with anxiety disorders20). In the clinical setting, patients with a higher than moderate degree of depression or anxiety on each inventory are recommended for referral to a psychologist for further evaluation and treatment.
Psychosocial adjustment of adolescents and adults with CHD
Although the exact prevalence of depression and anxiety in adolescents and adults with CHD is unknown, a number of studies have shown diverse ranges of depression and anxiety disorders. In assessing psychosocial adjustment, it is important to keep in mind that the prevalence of depression and anxiety varies significantly in adults with CHD, which may be influenced by international differences in economic, medical, and social environments.
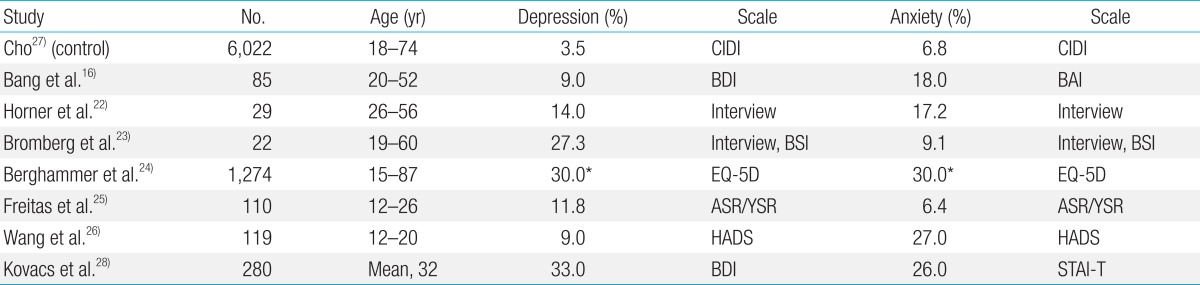
The reported prevalence of depression in adolescents and adults with CHD ranges from 9% to 33%, according to every evaluating scale16,21,22,23,24,25,26). A recent population study evaluating the prevalence of major psychological disorders from 6,022 healthy people (age range, 18-74 years) used the World Health Organization Composite International Diagnostic Interview in South Korea. Results indicated that the prevalence of depressive disorders identified by the criteria of the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) were 7.5% throughout life and 3.5% in the past year27). A recent survey to identify the frequency of depressive disorders in adults with CHD (age range, 20-52 years) using the BDI in the Seoul National University Children's Hospital (SNUCH) found that 18% of patients showed mild depression, 8% showed moderate depression, and 1% showed severe depression. These data suggested that over 9% of adult patients with CHD should be referred to a psychologist16). In a German study of 1,274 adults with CHD by EuroQol-5D, the authors found that 30% of the patients showed problems in the anxiety/depression dimensions24). Additional studies measuring the frequency of depressive disorders using different evaluation scales are presented in Table 3.
The reported prevalence of anxiety in adolescents and adults with CHD was generally higher than that of depression, and ranged from 6.4% to 27% according to each evaluation scale16,26). From a Korean general population study, the life-time and 1-year prevalence of anxiety disorders as identified by the criteria in DSM-IV were 8.7% and 6.8%, respectively27). Meanwhile, we found that 31% of CHD patients showed mild, 16% showed moderate, and 2% showed severe depression from SNUCH data by BAI, which suggests that more than 18% (more than moderate anxiety by BAI) of adult patients with CHD should be referred to a psychologist to be evaluated and properly treated16). Findings from various studies of anxiety disorder prevalence using different evaluating scales are also presented in Table 3.
Factors affecting psychosocial functioning of adolescents and adults with CHD
A number of studies have suggested major risk factors affecting psychosocial functioning in adolescents and adults with repaired or unrepaired CHD. A common assumption is that patients with severe CHD, such as functional single ventricle or Eisenmenger syndrome, would have greater psychosocial dysfunction. Freitas et al.25), reported from a cohort study that females, patients with severe CHD, patients with surgical repair, cyanotic patients, and the patients with severe-to-moderate form of residual lesions showed worse psychosocial adjustment. On the contrary, many other studies have shown that original CHD severity, present heart status, and present New York Heart Association functional class were not predictors of the impairment of psychosocial function of adults with CHD16,17,26,28,29,30). In one study, patients showed greater psychological resilience in response to the severity of their initial CHD, and each patient's disease severity had a harmful effect only when it was evaluated in view of poor functional status16). Another study found that adults with CHD who developed heart failure were particularly vulnerable to disorders of psychosocial functioning31).
A perceived financial burden was reported to be significantly related to anxiety, depression, and somatic symptoms, and lower perceived social support was significantly related to anxiety and depression in the CHD patients25,32). Kovacs et al.28) suggested that significant predictors of depressive mood were loneliness, perceived health status, and fear of negative evaluation, and predictors of patients' anxiety were loneliness and fear of negative evaluation. In this study, CHD severity and poor functional class did not predict patients' depressive mood or levels of anxiety28). Early exposure to stress from CHD and medical treatments from infancy, separation from parents during hospitalizations, and brain damage during treatments have also been known to provoke abnormal emotional adjustment and depression21).
Perception of self-image is also an important factor affecting psychosocial functioning of adults with CHD. An unfavorable self-image can lead patients to view themselves as defective, which subsequently can be associated with self-doubt and insecurity. As a result, this unfavorable perception of self-image strongly affects depressive moods and anxiety30). In addition to perception of self-image, cognitive perceptions are also believed to have a great influence on CHD patients' lives. The more negative perceptions patients had, the higher psychological distress was evident. Negative perception can be more strongly associated with higher distress and poorer psychosocial adjustment than the severity of CHD, which could develop from adolescence33).
Solutions to improve psychosocial function and QoL of adolescents and adults with CHD
A successful, smooth transition from adolescence to adulthood is very important for improving psychosocial functioning and QoL of CHD patients, whether they were repaired or not. To facilitate a successful transition, two important goals have been suggested: to prevent loss of follow-up care and to foster and encourage patients' self-care behaviors34). An accurate knowledge of CHD by patients has been associated with improved psychological functioning and the patients' QoL4,29,35). Although clear insight about their CHD is known to reduce patients' confusion and improve healthy behaviors for dealing with a chronic heart condition29), only 30% of child and adolescent patients indicated good insight into their CHD, and 77% of patients did not know the medical diagnosis of their own CHD, which meant that children and adolescents appeared to be less concerned about their CHD36). Therefore, it is necessary for health care providers to better inform CHD patients of the accurate diagnosis of their own disorder and overall treatment process during adolescence. One recent multicenter study in the United States, conducted to confirm the validity and reliability of the Pediatric Cardiac Quality of Life Inventory, supported the above-mentioned concept of monitoring CHD patients from childhood37).
Even patients with successfully repaired CHD had diverse psychosocial dysfunctions and significantly poorer QoL. However, little has been determined about effective psychological interventions for patients with CHD6,38). Although use of tricyclic antidepressants and selective serotonin receptor inhibitors for the treatment of secondary depression with diverse causes has been widely accepted39), specialized services devoted to individual patients' conditions may be preferable, because they could provide multidisciplinary and comprehensive patient care40). It is important to recognize that treating psychosocial disorders, including depression and anxiety, in CHD patients may require specialized multidisciplinary management to alleviate symptoms from diverse psychosocial dysfunction and to improve QoL40). Therefore, the primary health care provider for CHD patients is encouraged to cooperate actively with psychiatrists, psychologists, social workers, chaplains, and family members to improve psychosocial functioning.
Because feeling different from healthy people is a significant concern in the CHD patients' daily lives as mentioned above, helping CHD patients feel normal is another important intervention when managing patients' suffering12). Wang et al.26) suggested that a feeling of optimism was the most important factor in reducing CHD patients' depression and anxiety and that good social support and a strong sense of coherence were important for psychosocial stability. In our study, good psychosocial adaptation of CHD patients appeared to be the result of close family relationships and involvement making mental adjustment easier16).
Conclusions
The number of adolescents and adults living with CHD has been increasing every year and they continue to face physical, psychosocial, and environmental challenges. Although the exact prevalence of depression and anxiety in adolescents and adults with CHD is unknown, a number of studies have shown higher rates of depression and anxiety disorders than the general population. To improve psychosocial functioning and the QoL for adolescents and adults with CHD, health care providers should inform CHD patients of their accurate diagnosis and overall treatment process from adolescence. Active cooperation with psychiatrists, psychologists, social workers, chaplains, and family members is recommended to help CHD patients feel normal and optimistic, and to encourage good social relationships, close family relationships, and a strong sense of coherence.
Notes
No potential conflict of interest relevant to this article was reported.