Urinary bladder rupture during voiding cystourethrography
Article information
Abstract
Voiding cystourethrography (VCUG) is a commonly performed diagnostic procedure for the evaluation of vesicoureteral reflux with urinary tract infection or congenital renal diseases in children. The procedure is relatively simple and cost-effective, and complications are very rare. The iatrogenic complication of VCUG range from discomfort, urinary tract infection to bacteremia, as well as bladder rupture. Bladder rupture is a rare complication of VCUG, and only a few cases were reported. Bladder rupture among healthy children during VCUG is an especially uncommon event. Bladder rupture associated with VCUG is usually more common in chronically unused bladders like chronic renal failure. Presented is a case of bladder rupture that occurred during a VCUG in a healthy 9-month-old infant, due to instilled action of dye by high pressure. This injury completely healed after 7 days of operation, and it was confirmed with a postoperative cystography. The patient's bladder volume, underlying disease, velocity of the contrast media instilled, catheter size, and styles of instillation are important factors to prevent bladder rupture during VCUG. Management of bladder rupture should be individualized, but the majority of infants are treated with the operation. In conclusion, bladder rupture is a rare complication, however, delicate attention is needed in order to prevent more dire situations.
Introduction
Voiding cystourethrography (VCUG) is a commonly performed diagnostic procedure for the evaluation of vesicoureteral reflux (VUR) in children with urinary tract infections (UTI) or congenital renal diseases such as hydronephrosis, bladder diverticula, and posterior urethral valves1). VCUG is a relatively invasive procedure that uses a simple and practical device when compared to computed tomography or magnetic resonance imaging2), and it rarely has complications. Thus, VCUG is often ordered by a pediatric nephrologist to detect VUR.
However, it is important to be cognizant of the rare complications that can occur. Some reported complications of VCUG range from urinary discomfort, UTI to bacteremia, as well as bladder rupture3). Bladder rupture is sometimes associated with a diseased bladder wall, such as with congenital bladder diverticula or a chronically unused bladder in chronic renal failure but is less common in healthy children and there has been only few cases reported4). We report a case of iatrogenic bladder rupture during VCUG in a child with no specific underlying disease.
Case report
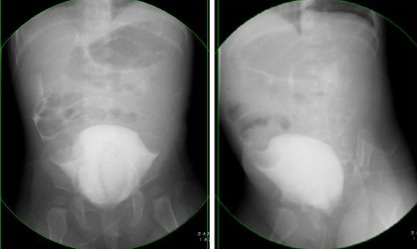
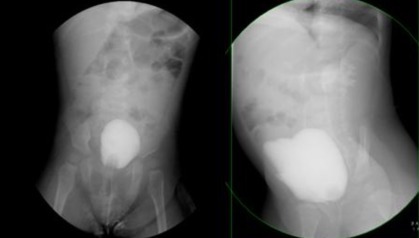
A 9-month-old female infant with no significant medical or surgical history was admitted due to a febrile UTI. Her urine culture study demonstrated Escherichia coli of more than 100,000 colony forming units/mL. During evaluation, renal ultrasonography showed normal findings, but VCUG was performed to detect VUR by a skilled pediatric radiologist and pediatrician on the seventh day of her hospital stay. A 5-Fr. foley catheter with a balloon was inserted into the urethra, and residual urine was removed. An 80 mL - a mixture of saline and contrast media, was instilled using a 50-mL syringe, under a fluoroscopic guide until the dome of the bladder completely distended. The bladder was normal in contour, and a grade II VUR within the right ureter and a grade III VUR within the left ureter were noted (Fig. 1). Afterwards, the 5-Fr. foley catheter was removed. During the voiding time, she voided spontaneously. However, in just a few seconds, intraperitoneal contrast media was observed (Fig. 2). On physical examination, the patient was found tachypneic with a distended and tender abdomen. Her vital sign was checked as respiratory rate was 32 per minute, and blood pressure was 103/67. The patient was transferred to the urology department. She was immediately sent to the operating room and underwent exploration. Urine, blood clots and contrast media were evacuated from the peritoneum. An approximately 3 cm long bladder rupture from the left side of the bladder wall was found after removal of the contrast media remnant from the peritoneum. The bladder was closed in two layers using an absorbable 5-0 vicryl sutures. A 5-Fr. foley catheter was left per urethra. A suprapubic tube was not used. Perioperative antibiotics were administered, and the foley catheter was removed on postoperative day 7. No leakage of the bladder upon postoperative cystography was noted. The patient's recovery was uneventful and she can void spontaneously to date.
The voiding cystourethrogram shows the filling phase after the instillation of 80 mL of contrast media.
Discussion
VCUG is a radiologic procedure for the evaluation of the bladder and urethra, which is valuable for examining and following-up on a VUR and for helping the prevention of renal damage. Iatrogenic complications associated with VCUG are rare events, but some complications include UTI, allergic reaction after procedure, contact dermatitis, knotting of the urethral catheter, and bladder rupture5-10). In Korea, one study reported that 32.7% of patients with VCUG showed complications such as bladder rupture, dysuria, irritability, and hematuria11). Bladder rupture associated with VCUG is more common in instances of chronically unused bladders such as chronic renal failure, and six cases of bladder rupture were reported in chronic renal failure12). Bladder rupture is a rare complication and delicate attention is needed due to its emergency situation10).
To perform a safe VCUG, we should pay attention to some factors such as bladder volume, the patient's underlying disease, the velocity of the contrast instilled, and catheter size13). At birth, bladder volume is about 30 mL regardless of sex, and two formulas have been proposed for bladder volume estimation in children according to their age and weight: age<1 year, bladder volume (mL)=38+(2.5×age [mo]); age>1 year, bladder volume (mL)=(age [yr]+1)×3014,15). However, the bladder volume is different among individuals, and the bladder dome which is the weakest part of bladder can easily be ruptured when excess volume is injected rapidly11).
Also, catheter size and type has significance. For short-term catheterization to obtain a urine specimen or to perform an investigative procedure, a 5-Fr. feeding tube is recommended for neonates and an 8-Fr. feeding tube for children16). Using a Foley catheters is risky because the balloon can block the urinary flow and the bladder can rupture17). Therefore, much care is necessary in using a Foley catheter instead of feeding tube.
Proper catheter insertion, fluoroscopic guide, pressure, and number of filling cycles should be considered in for the instillation18). To avoid pressure overload, pressured manual injection of the contrast material must not be used, while a gravity method must be used18,19). At this time, the contrast container should not be placed higher than 60 cm from the patient. More than two cycles of filling does not appear to be necessary18,20). Underlying diseases such as chronic renal failure are also another important determining factor12,21).
Five cases of iatrogenic bladder perforation have been reported in children following VCUG. Most of all (4 cases), the main cause of bladder rupture was manual injection of the contrast material and in one case, the chief cause was underlying disease (hutch diverticula)22-26).
In this case, the main causes of the bladder rupture are considered to be the use of the Foley catheter instead of a feeding tube, manual injection of contrast media, and the excess volume instilled more than expected volume.
Management of infantile bladder rupture should be individualized case to case. In the review by Trulock et al.27), the majority of reported infants were treated with abdominal exploration and repair of the bladder leakage site, but some of the patients could be managed by the implementation of a vesicotomy or urethral catheter alone.
In conclusion, the majority of complications associated with VCUG are not critical, but in several cases, severe complications such as bacteremia and bladder rupture can occur in several cases. Therefore, the operator should be well informed of the procedure, and aseptic techniques, while delicate observation of potential for the complication is needed.
Acknowledgment
This case report was presented as a poster at the Korean pediatric society fall symposium of 2011.