Two cases of female hydrocele of the canal of nuck
Article information
Abstract
The processus vaginalis within the inguinal canal forms the canal of Nuck, which is a homolog of the processus vaginalis in women. Incomplete obliteration of the processus vaginalis causes indirect inguinal hernia or hydrocele of the canal of Nuck, a very rare condition in women. Here, we report 2 cases of hydrocele of the canal of Nuck that were diagnosed with ultrasonography in both cases and magnetic resonance imaging in 1 case to confirm the sonographic diagnosis. High ligation and hydrocelectomy were conducted in both patients. In 1 patient, 14 months later, the occurrence of contralateral inguinal hernia was suspected, but did not require surgery. The other patient had a history of surgery for left inguinal hernia 11 months before the occurrence of right hydrocele of the canal of Nuck. In both cases, the occurrence of an inguinal hernia on the contralateral side was noted.
Introduction
The round ligament is attached to the uterus and a small evagination of the parietal peritoneum accompanies the round ligament through the inguinal ring into the inguinal canal in the female1). This small evagination of the parietal peritoneum is the canal of Nuck in the female, which is homologous to the processus vaginalis in males. The canal of Nuck is normally obliterated in the first year of life. Failure to achieve complete obliteration results in an indirect inguinal hernia or hydrocele of the Canal of Nuck1,2). Here, we report two cases with ultrasound and magnetic resonance (MR) findings and we review the literature. Several cases with this rare anomaly have been reported, but MR findings have not previously been reported in the Korean literature. Kim et al.3) reported three cases which were diagnosed with sonography and CT. Park et al.4) reported one case which were diagnosed with sonography and MR imaging. In both cases, the occurrence of contralateral side inguinal hernia was noted although there have been no reports about the recurrence of this anomaly.
Case reports
1. Case 1
A 4-year-old girl presented with a palpable mass in her right inguinal region. The mass was grape sized, tense, but not painful. The swelling was translucent and irreducible. She was in good physical health without any symptoms. There was no heating sensation nor erythematous change in the lesion. The differential diagnosis included hernia or hydrocele.
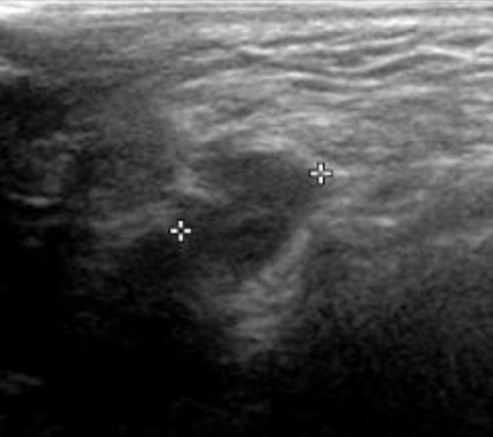
Inguinal ultrasonography with a 5 to 12 MHz linear array transducer revealed an ovoid shaped cystic mass of about 1.8 cm × 2.5 cm in the right inguinal region (Fig. 1). No bowel loop or omental fat was observed during the ultrasonographic examination. But, charicterization was difficult because it seemed a non-specific cystic lesion. MR imaging was requested to confirm the ultrasound finding and identify the relations with the surrounding structures. MR imaging showed a cystic mass in the right inguinal region (Fig. 2). The mass was well-defined cystic lesion without abnormal septation and solid portion.
Inguinal sonography. Ultrasonography of the right inguinal area shows a cystic lesion without internal echoes. During the ultrasonography, no bowel or omental fat herniation was noted.
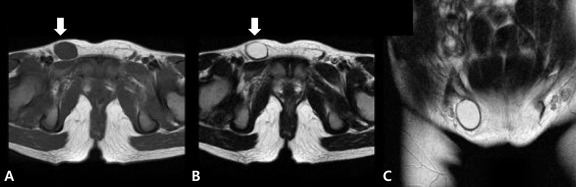
Magnetic resonance findings of a hydrocele of the canal of Nuck. (A) Axial T1-, (B) axial T2-, and (C) coronal T2-weighted images show the cystic mass (low intensity on the T1-weighted image, high intensity on the T2-weighted images) with a thin wall in the right inguinal area (white arrows).
High ligation and hydrocelectomy were performed. The round ligament with the cystic tense mass was excised. The pathologic examination revealed findings compatible with a hydrocele of the Canal of Nuck. Fourteen months later, she revisited the hospital because of a left inguinal mass that was considered to be a left inguinal hernia. However, the mass was reduced spontaneously and did not protrude for the next 4 years.
2. Case 2
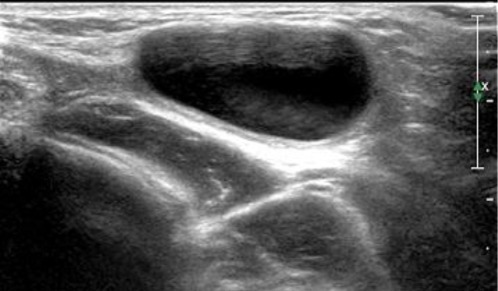
An 18 month-old female patient presented with a small, right inguinal mass with tenderness. Ultrasound examination revealed a small sized, well-defined cystic mass about 0.74 cm×0.63 cm (Fig. 3). She had a history of herniorrhaphy of a left inguinal hernia which was diagnosed with ultrasound examination at the age of 7 months. High ligation of the hernial sac and hydrocelectomy was done, which was confirmed by the pathology report. There was no occurrence of contralateral hydrocele or hernia for the next 3 years.
Discussion
The processus vaginalis, which is a homologue to the canal of Nuck, may be obliterated at any point between the internal inguinal ring and the scrotum, or it may happen incompletely. These variations account for the diverse classification of hernias (the extraabdominal passage of viscus) and hydroceles (the extra-abdominal passage of peritoneal fluid), including complete or scrotal hernias, communicating or non-communicating hydroceles, hydroceles of the spermatic cord in males, and the canal of Nuck in girls5).
Hydroceles are common in children, especially in boys. But hydrocele of the canal of Nuck is an uncommon clinical presentation6).
Although the exact process is unclear, it is generally agreed that obliteration of the processus vaginalis occurs only after the seventh month of gestation7), thus accounting for the higher incidence of inguinal hernias in the premature infant8). Although not clearly defined, there is a known heredity factor associated with the occurrence of hernias that is more frequent in twin gestations and in infants who have a family history of hernia9).
Swelling of the inguinal region in a female may result from a number of conditions, including inguinal hernia, tumor (lipoma, leiomyoma, sarcoma), cyst, abscess, lymphadenopathy, or hydrocele of the canal of Nuck1).
In most cases, the canal of Nuck should be distinguished from hernia. Bowel sounds over the swelling are strongly suggestive of a hernia.
Hydrocele of the canal of Nuck typically presents as a painless, translucent swelling in the inguinolabial region6). There is no nausea or vomiting. If possible, the child should be examined in the supine and standing positions6). In older children, Valsalva's maneuver should be performed to rule out hernia. If the bulge is apparent in the standing position and disappears while supine, a hernia is more plausible10).
Infection is an uncommon complication of hydroceles in children, and until now only 5 cases have been reported in the English language literature, all in boys. Infected hydrocele of the canal of Nuck is rare11).
In the past, a palpable inguinal mass was removed via surgery without an imaging study. Currently, sonography is the imaging modality of choice for evaluation of this type of mass12).
Because sonography is a relatively easy, accessible and accurate procedure4), we recommend that sonography be performed routinely in those females with an inguinal hernia containing an asymptomatic movable mass. But, we cannot identify whether there is a communication between cystic mass and peritoneal cavity with sonography. MR imaging can give more precise images including septation and a communication between cystic lesion and peritoneal cavity, and information on the anatomical relation with adjacent structures4,13). Therefore, MR imaging can help to diagnose in patients with inguinal cystic mass. The differential diagnosis of a cystic mass in the female groin region includes round ligament cysts, varicosities of the round ligament, inguinal herniation of the ovary, cystic lymphangiomas, epidermal inclusion cysts, abscesses, and pseudoaneurysms14).
The final diagnosis is made during surgery and confirmed by pathological examination6). Surgical resection of the hydrocele and ligation of the neck of the processus vaginalis should be considered as standard therapy.
Han et al.15) reported that in 2.6% of the patients who had been operated of unilateral hydrocele, contralateral hernia occurred. They also reported that the occurrence of the contralateral hydrocele after the operation of unilateral hydrocele was 2.0% in males. Flum et al.16) reported that the recurrence rate in inguinal hernia is about 10% but has not been reported for a hydrocele of the canal of Nuck yet. In our cases, the occurrence of inguinal hernia was on the contralateral side from the hydrocele and operation was needed in one case. Therefore, one should be aware that the ocurrence rate of the contralateral hernia is not low in patients with hydrocele of the canal of Nuck. So, we should consider the hydrocele of the canal of Nuck in patients who have a inguinal cystic mass and have a history of inguinal hernia on the other side.
In these cases, we suggest that MR imaging can help to identify an inguinal cystic mass when the diagnosis is vague by its sonographic findings in female. Because the inguinal hernia on the other side was detected either before or after the operation of hydrocele in both cases, we should consider the hydrocele of the canal of Nuck in patients who have an inguinal cystic mass and have a history of an inguinal hernia on the other side. Also, we should consider the risk of occurrence of contralateral inguinal hernia in patients with hydrocele of canal of Nuck.