Hematopoietic stem cell transplantation in children with acute leukemia: similar outcomes in recipients of umbilical cord blood versus marrow or peripheral blood stem cells from related or unrelated donors
Article information
Abstract
Purpose
This study compared outcomes in children with acute leukemia who underwent transplantations with umbilical cord blood (UCB), bone marrow, or peripheral blood stem cells from a human leukocyte antigen (HLA)-matched related donor (MRD) or an unrelated donor (URD).
Methods
This retrospective study included consecutive acute leukemia patients who underwent their first allogeneic hematopoietic stem cell transplantation (HSCT) at Samsung Medical Center between 2005 and 2010. Patients received stem cells from MRD (n=33), URD (n=46), or UCB (n=41).
Results
Neutrophil and platelet recovery were significantly longer after HSCT with UCB than with MRD or URD (P<0.01 for both). In multivariate analysis using the MRD group as a reference, the URD group had a significantly higher risk of grade III to IV acute graft-versus-host disease (GVHD; relative risk [RR], 15.2; 95% confidence interval [CI], 1.2 to 186.2; P=0.03) and extensive chronic GVHD (RR, 6.9; 95% CI, 1.9 to 25.2; P<0.01). For all 3 donor types, 5-year event-free survival (EFS) and overall survival were similar. Extensive chronic GVHD was associated with fewer relapses (RR, 0.1; 95% CI, 0.04 to 0.6; P<0.01). Multivariate analysis showed that lower EFS was associated with advanced disease at transplantation (RR, 3.2; 95% CI, 1.3 to 7.8; P<0.01) and total body irradiation (RR, 2.1; 95% CI, 1.0 to 4.3; P=0.04).
Conclusion
Survival after UCB transplantation was similar to survival after MRD and URD transplantation. For patients lacking an HLA matched donor, the use of UCB is a suitable alternative.
Introduction
Allogeneic hematopoietic stem cell transplantation (HSCT) is the only curative option for many diseases, such as hematologic malignancies, immune deficiency syndrome, or bone marrow failure. A human leukocyte antigen (HLA)-matched related donor (MRD) is considered the best hematopoietic stem cell (HSC) donor; however, only about 30% of patients can be transplanted from an HLA-MRD. In the absence of such donor, the search for an unrelated volunteer adult donor is currently performed. Transplantation from an unrelated adult donor, however, is limited by HLA-matching requirements, a high incidence of graft-versus-host disease (GVHD), and donor availability.
Since the first successful cord blood transplantation (CBT) was performed in 1988, the use of CBT has increased substantially, which has extended the availability of this treatment, especially for children. Although several disadvantages of CBT still exist, including a higher rate of graft failure and delayed hematopoietic recovery, CBT still offers many practical advantages as an alternative source of HSC, such as easy procurement without risks to the donor, reduced risk of transmitting infections, fast accessibility, and relatively low incidence and severity of GVHD. In addition, a Eurocord study has shown comparable results after transplantation from unrelated cord blood (UCB) and from other sources of HSC1).
The outcomes of HLA-matched adult unrelated donors have become comparable to that of HLA-MRD, with the development of better characterization of HLA type, improvements in GVHD prophylaxis, and treatments of infection2-4). Furthermore, several studies have shown comparable results after transplantation from UCB and unrelated bone marrow (BM)5,6). Since the number of allogeneic HSCT using alternative donors is increasing, it is becoming critical to choose the best donor for each patient receiving an allogeneic HSCT. Therefore, in this study, we compared the outcomes of children with acute leukemia receiving unrelated cord blood transplantation (UCBT) to those of children receiving BM or peripheral blood stem cells (PBSC) from an HLA-MRD or unrelated donor (URD). The results obtained in this study will help establish the search guidelines for identifying an optimal donor for an allogeneic HSCT.
Materials and methods
1. Study patients and transplantations
A retrospective chart review was performed on children with acute leukemia who received an allogeneic HSCT at the Samsung Medical Center, Korea from January 2005 to December 2010. We excluded recipients who received two or more types of stem cell sources. Patients who had received previous allogeneic transplantation were excluded. UCBT was performed if no suitable HLA-MRD or URD were available. HLA compatibility was determined by high-resolution typing for HLA-A, -B, and -DRB1 as well as by serotyping for HLA-C for HSCT from URD. UCBT grafts were matched with at least 4-6 HLA-A and -B at antigen level and -DRB1 at the allele level to the recipient and in patients receiving 2 UCB units to each other. Double unit UCBT was performed if no suitable UCB unit with nucleated cell counts>3.0×107/kg or CD34+ cell count>1.7×105/kg was available. All patients underwent a myeloablative conditioning regimen. The GVHD prophylaxis was as follows: cyclosporine alone for HSCT from related BM or PBSC (MRD), cyclosporine and methotrexate for HSCT from unrelated BM or PBSC (URD), and cyclosporine and mycophenolate mofetil for HSCT from UCB. While antithymocyte globulin (ATG) was mostly used in the conditioning regimen for the UCBT, ATG was not administered for HSCT when other stem cell sources were used. All included recipients were divided into three groups according to the donor source as follows: MRD, URD, and UCB.
2. Definitions
Neutrophil recovery was defined as the estimated time from transplantation to the first of three consecutive days when an absolute neutrophil count (ANC) of at least 0.5×109 per liter was obtained. Platelet recovery was defined as the achievement of a platelet count of 20×109 per liter without support of transfusions for seven continuous days. Graft failure was defined as the lack of donor-derived neutrophil recovery or the requirement for either a boost from the same donor or a second transplant for lack of count recovery. Advanced disease was defined as more than a complete remission (CR)1 for acute myeloid leukemia (AML), more than CR2 for acute lymphoblastic leukemia (ALL), and refractory disease. Diagnosis and grading of acute and chronic GVHD were based on standard clinical criteria and biopsy when available7,8). Recipients who survived at least 100 days with sustained engraftment were evaluated for chronic GVHD. Relapse was defined as a recurrence of leukemia. Non-relapse mortality (NRM) was defined as death after transplant that was not preceded by recurrent or progressive malignancy. Event-free survival (EFS) was defined as survival in a state of continuous complete remission.
3. Statistics
Patient characteristics and the outcomes of transplantation were compared across groups using the chi-square and Fisher exact tests. Continuous variables were compared using the Kruskal-Wallis test with the Tukey test using ranks. The five-year probabilities of overall survival (OS) and EFS were estimated with the Kaplan-Meier methodology and compared using the log-rank test for univariate comparisons. For analyzing EFS, leukemic relapse or death was considered an event. For analysis of OS or EFS, data from recipients without an event were censored at the last follow-up after HSCT. The cumulative incidence was estimated for NRM and relapse in order to take competing risks into account according to the method of Fine and Gray. Multivariate analysis using Cox proportional hazard regression model and logistic regression model of outcomes after transplantation was performed using variables with a P value of 0.1 or less according to groups. The variable for graft type was retained in all steps of model building. Results were expressed as hazard ratios that represented the relative risk (RR) of occurrence of the outcomes with URD or UCB as compared to MRD. Other variables that were considered in multivariate analysis for GVHD included age of transplant recipient, status of the disease at transplantation, the conditioning regimen (i.e., with irradiation vs. without it), the use of ATG, and the total dose of nucleated cells. In multivariate analysis for relapse, NRM, and EFS, other variables were age of transplant recipient, status of the disease at transplantation, the conditioning regimen (i.e., with irradiation vs. without it), acute GVHD, and extensive chronic GVHD. All statistical analyses were performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) and STATA release 11 (StataCorp LP., College Station, TX, USA).
Results
1. Characteristics of patients
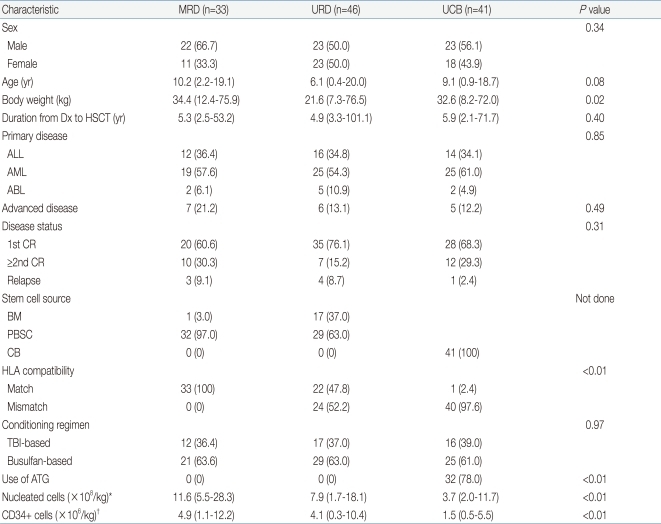
The characteristics of the patients are shown in Table 1. All of the recipients included in the study were classified under three groups: MRD (n=33), URD (n=46), and UCB (n=41). The median age of all study patients was 8.3 years. The male to female ratio was 1.3:1. Three groups were similar with respect to sex, age at HSCT, and conditioning regimens. Among the patients, the proportions with AML, ALL, and acute biphenotypic leukemia were similar in all three groups (P=0.85). The three groups also had a similar disease status (P=0.31). Although ATG was not administered to recipients of MRD and URD, 78% of UCB recipients received ATG (P<0.01). All UCB grafts, with the exception of one, were HLA-mismatched, whereas 48% of URD transplants were HLA-matched (P<0.01). In 24 recipients of HLA-mismatched URD graft, four patients received 3-5 loci mismatched grafts, seven patients from 2 loci mismatched graft, and 13 patients from 1 locus mismatched grafts. Among 13 recipients of 1 locus mismatched graft, mismatched locus was HLA-A in 3 patients, HLA-B in 2 patients, HLA-C in 5 patients, and HLA-DRB1 in 3 patients. Among 41 recipients of UCB, 31 patients received double-unit UCBT. The median number of nucleated cells and CD34+ cells infused in the UCB group were lower than other groups.
2. Hematopoietic recovery
Table 2 shows the outcomes after HSCT. All recipients in the MRD and URD groups showed successful engraftment, whereas graft failure occurred in 4 recipients in the UCB group (P<0.01). Neutrophil and platelet recoveries were significantly delayed after UCBT compared to HSCT from MRD or URD (both P<0.01).
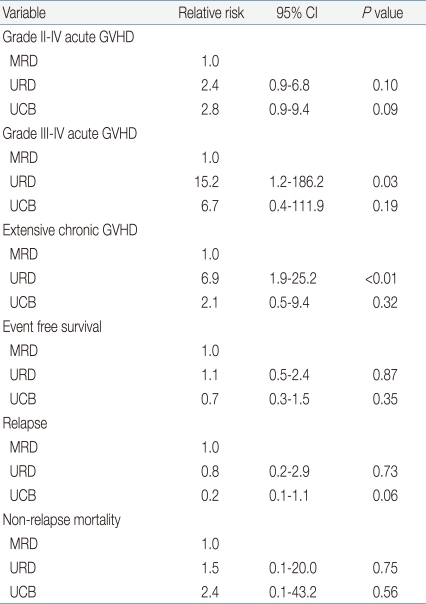
3. GVHD
In univariate analysis, the rate of grades II to IV acute GVHD was higher in recipients of URD and UCB transplants compared to MRD recipients (P=0.04). Using the MRD group as the reference category in a multiple regression analysis, the risk of grades II-IV acute GVHD was similar among recipients of transplants from URD and UCB and the RR was 2.4 and 2.8, respectively, however; which did not reach the statistical significance (P=0.1 and P=0.09, respectively) (Table 3). The rate of grades III to IV acute GVHD was 20% in the URD group. In the multiple regression analysis, there was a higher risk of grade III to IV acute GVHD (RR, 15.2; 95% confidence interval [CI], 1.2 to 186.2; P=0.03) in recipients of URD grafts (Table 3). Despite the high-degree of HLA mismatch between donor and recipient, the risk of acute GVHD grades III to IV after UCB transplant was not significantly higher than those after MRD transplant (Table 3). The rate of extensive chronic GVHD was 53.8% in the URD group, which was significantly higher than the MRD and UCB groups (Table 2). In the multiple regression analysis, the RR of extensive chronic GVHD was 6.9 (95% CI, 1.9 to 25.2) compared to the MRD group (P<0.01). The risk of extensive chronic GVHD was not higher in the UCB group compared to the MRD group (P=0.32).
When the risk of GVHD was compared in URD group according to the HLA disparity, the rate of grades III to IV acute GVHD was 9.5% and 29.5% in recipients of HLA-matched URD graft and HLA-mismatched URD graft, respectively (P=0.1). The rate of extensive chronic GVHD was 50.0% and 57.9% in recipients of HLA-matched URD graft and HLA-mismatched URD graft, respectively (P=0.6).
4. Relapse and non-relapse mortality
There was a trend toward a higher cumulative incidence of relapse in the MRD group, but this trend did not reach statistical significance (Fig. 1A). In a multivariate regression analysis, the only factor that had a significant impact on the risk of relapse was the advanced disease (RR, 12.7; 95% CI, 2.3 to 66.9; P<0.01). Moreover, the extensive chronic GVHD showed a protective effect on the relapse (RR, 0.1; 95% CI, 0.04 to 0.6; P<0.01).
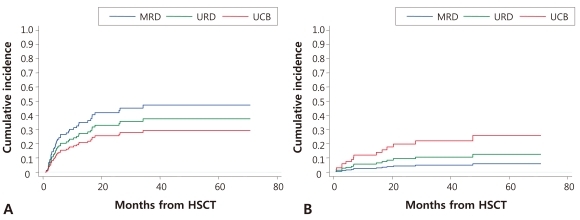
(A) The cumulative incidence of relapse by donor. There was a trend toward a higher cumulative incidence of relapse in the matched related bone marrow or peripheral blood stem cells (MRD) group (P=0.13). (B) The cumulative incidence of non-relapse mortality (NRM) by donor. The cumulative incidence of NRM was higher in unrelated umbilical cord blood (UCB) transplants (P=0.03). HSCT, hematopoietic stem cell transplantation; URD, unrelated bone marrow or peripheral blood stem cells.
The cumulative incidence of NRM was higher in transplants with UCB (Fig. 1B). In a multivariate analysis, extensive chronic GVHD increased the risk of NRM (RR, 9.0; 95% CI, 1.5 to 54.1; P=0.02). When evaluating the causes of death according to the donor source, disease recurrence was the most frequent cause of death in recipients of MRD (8/9, 86.3%) and URD (9/14, 64.3%). However, the most frequent cause of death in recipients of UCB was infection (7/15, 46.7%). The proportion of GVHD as the cause of death was 11.1% in the MRD group, 28.6% in the URD group, and 13.3% in the UCB group (P=0.46).
5. Survival
EFS and OS were similar among all groups (Fig. 2). The 5-year EFS was 48.7% for the MRD group, 48.3% for the URD group, and 45.9% for the UCB group, respectively (P=0.98). The factors associated with EFS advanced disease at transplantation (RR, 3.2; 95% CI, 1.3 to 7.8; P<0.01) at transplantation and total body irradiation (RR, 2.1; 95% CI, 1.0 to 4.3; P=0.04) based on multivariate analysis. The 5-year OS was 53.3% for the MRD group, 56.6% for the URD group, and 55.2% for the UCB group, respectively (P=0.80).

(A) The 5-year event-free survival (EFS) and (B) overall survival (OS). There were no significant differences in EFS of OS among the groups. HSCT, hematopoietic stem cell transplantation; MRD, matched related bone marrow or peripheral blood stem cells; URD, unrelated bone marrow or peripheral blood stem cells; UCB, unrelated umbilical cord blood.
Discussion
Since the National Health Insurance began allowing UCBT in children under the age of 16 years in January 2003, the number of UCBT cases has increased dramatically in Korea. A multicenter analysis of 236 children who underwent UCBT in Korea suggested that UCBT was a reasonable alternative as an HSC source9).
The data in the present study indicate that allogeneic HSCT for patients with acute leukemia can result in durable EFS between 46% and 49% at 5 years using MRD, URD, or UCB sources. Remarkably, the OS was similar between the MRD, URD, and UCB HSCT groups, which was nearly 55% at 5 years. Importantly, our results are not inferior to other studies. A Eurocord study of children with acute leukemia showed 2-year OS of 49% and 35% in URD and UCB groups, respectively6). In another study, the 5-year leukemia free survival was 41% in recipients of MRD and 43% in recipients of UCB in children with ALL in second CR, respectively10). According to the studies of HSCT outcomes that included adult data, the survival of HSCT using UCB was comparable to HSCT using URD and even MRD11-14).
The adjusted risk of acute and chronic GVHD was not higher in transplants from UCB than transplants from MRD, despite a high degree of disparity in HLA between donor and recipient in the UCB group. Although most UCB recipients received ATG as a part of conditioning regimen, the use of ATG was not associated with the incidence of acute and chronic GVHD (P=0.55 and P=0.43, respectively). From the early experiences of UCBT, the incidence of GVHD was less than expected given the degree of HLA disparity. The exact reasons for the relatively lower incidence of GVHD are unknown, but likely result from the functional immaturity of the infused lymphocytes, including decreased cytotoxicity, an altered cytokine profile, decreased HLA expression and increased regulatory T-cells15). However, graft-versus-leukemia (GVL) effect might be preserved in transplants from UCB, which indicates a trend toward a lower incidence of relapse in the UCB group (Fig. 1A). The results in the present study are in agreement with the previous reports suggesting that there is no increased risk of leukemia relapse when UCB is used as a stem cell source6). Furthermore, Verneris et al.16) suggested that double-unit UCBT might decrease the risk of relapse due to enhanced GVL effect. In the present study, most recipients of UCB (75.6%) underwent double-unit UCBT and we also found a trend toward less relapse in recipients of UCB (Fig. 1A).
The success of UCBT has been limited by the low cell number, which results in a higher rate of graft failure, delayed hematopoietic recovery, and increased infection complications. In the present study, we also found that neutrophil and platelet recovery was delayed significantly in the UCB group compared to the other HSC sources. In addition, the incidence of graft failure was higher than other HSC sources (Table 2). The delayed hematopoietic recovery in the UCB group might adversely affect recipients, since the NRM was significantly higher in the UCB group, which was mainly due to infection. To overcome these engraftment problems, several clinical experiments with ex vivo expanded cord blood cells have been explored, which have not resulted in a clinical benefit to date17,18). Recently, mesenchymal stem cells (MSCs) were investigated to support hematopoiesis in HSCT when co-transplanted with HSCs, and several studies have shown positive results19,20). In this context, we assessed the co-transplantation of MSCs with UCBT in our center as a way to overcome the cell dose limitation of UCBT and the initial results were promising (SHL, manuscript submitted Aug 2011). We also found in an animal model that the augmentation of HSC engraftment with MSCs co-transplantation was dependent on the number of MSCs implanted21). Therefore, the benefit of MSCs co-transplantation may facilitate the application of UCBT in patients lacking a suitable donor, even in adults, and may further decrease the complications associated with low cell number. Importantly, long-term follow-up is needed to assess the influence of co-transplantation with MSCs on the relapse of leukemia.
The limitation of this study was that patients were not randomized to each group. Although UCBT was performed, when there was no suitable HLA-MRD or unrelated adult donor available, several factors such as the urgency of HSCT, cell dose, HLA typing, and the size of the patient were taken into account for choosing the stem cell sources. However, the patient characteristics among the groups were very similar in our study.
In conclusion, this study has shown that survival in the MRD, URD, and UCB groups was similar, but that the type of complications differed, with a higher occurrence of acute and chronic GVHD in the URD group, higher trend of occurrence of relapse in the MRD group, and more NRM in the UCB group. These findings suggest that both URD and UCB represent alternative stem cell sources for children with acute leukemia who lack a MRD donor. Moreover, the rapid availability of a UCB may be a particular advantage for patients who require urgent transplantation.
Acknowledgment
This study was supported by a grant from the National R&D Program Cancer Control, Ministry for Health, Welfare and Family affairs, Republic of Korea (0520290).