Wolff-Parkinson-White syndrome in young people, from childhood to young adulthood: relationships between age and clinical and electrophysiological findings
Article information
Abstract
Purpose
The aim of the present study was to evaluate the characteristics of electrophysiologic studies (EPS) and radiofrequency ablation (RFA) performed in subjects aged less than 30 years with Wolff-Parkinson-White (WPW) syndrome, particularly pediatric patients under 18 years of age, based on our experience.
Methods
Two hundred and one consecutive patients with WPW syndrome were recruited and divided to 3 groups according to age: group 1, 6 to 17 years; group 2, 18 to 29 years; and group 3, 30 to 60 years. The clinical, electrophysiological, and therapeutic data for these patients were evaluated by a retrospective medical record review.
Results
A total of 73 (36%) of these patients were <30 years of age. Although there were more males than females in group 2 (male:female, 31:11), there was no sex difference in group 1 (male:female, 16:15). Left accessory pathway was detected less frequently in group 1 (32%, 10/31) than in group 2 (57%, 24/42) and group 3 (63%, 81/128) (P=0.023 and P=0.002, respectively).
Conclusion
The present study describes several different electrophysiological characteristics in children and adolescents with WPW syndrome. Therefore, when EPS and RFA are performed in children and adolescence with WPW syndrome, we recommend that these characteristics be considered.
Introduction
Wolff-Parkinson-White (WPW) syndrome presents the risk of sudden cardiac death (SCD) from ventricular fibrillation related to atrial fibrillation (AF) or flutter in individuals whose accessory pathway (AP) shows a short anterograde refractory period1), although the frequency of SCD is low (0.3%)2-4). Radiofrequency ablation (RFA) of the AP has been shown to be both safe and effective in symptomatic and asymptomatic WPW patients, and provides a 'cure' in more than 95% of the patients5-9). Recent studies have described the active use of electrophysiologic studies (EPS) for the risk stratification of arrhythmia in asymptomatic WPW patients, and have emphasized that the electrophysiologic findings, such as, the locations and numbers of APs, should be considered when considering a procedure involving RFA10-12). The clinical and electrophysiological characteristics of subjects with WPW syndrome may vary according to age13-17). The aim of the present study was to evaluate the characteristics of EPS and RFA performed in subjects aged less than 30 years with WPW syndrome, especially pediatric patients under 18 years of age, based on our experience.
Materials and methods
Two-hundred and one patients with WPW syndrome aged from 6 to 75 who consecutively underwent EPS from January 2003 to May 2010 in Keimyung University Dongsna Medical Center and Kyungpook National University Hospital were recruited for this retrospective study.
Among all patients, seventy-three patients (36%) were <30 years of age, and they were defined as young people. Patients were divided into three age groups group 1, 6 to 17 years, group 2, 18 to 29 years, and group 3, 30 to 60 years. EPS was indicated 1) when WPW patients had suspected or documented tachycardia or syncope, 2) when asymptomatic WPW patients had the need for further evaluation, 3) when asymptomatic WPW patients wanted EPS and RFA. The location of the AP was confirmed by EPS using standard electrophysiological mapping methods. AF or reentrant tachycardia was induced by rapid and continuous atrial (A) or ventricular (V) pacing, or extrastimulus technique. Effective refractory period (ERP) was defined as the longest coupling interval between the basic drive and the premature impulse that fails to propagate through AP. After the location of the AP was confirmed, RFA was tried 1) when AV reentrant tachycardia was induced, 2) when AF was induced, 3) when patient wanted RFA for abnormal electrocardiogram (ECG) findings. Successful RFA was considered if antegrade conduction through AP during A pacing or retrograde conduction during V pacing did not recur for at least 30 minutes after the RFA. The clinical, electrophysiological, and therapeutic data of these patients were reviewed from their medical records.
1. Statistical analysis
Statistical analysis was performed using IBM SPSS ver. 18.0 (IBM, New York, NY, USA). The independent t-test and crosstabulation analysis (the chi-square test) were used to compare clinical and electrophysiological data. P values of <0.05 were considered statistically significant.
Results
1. Clinical data
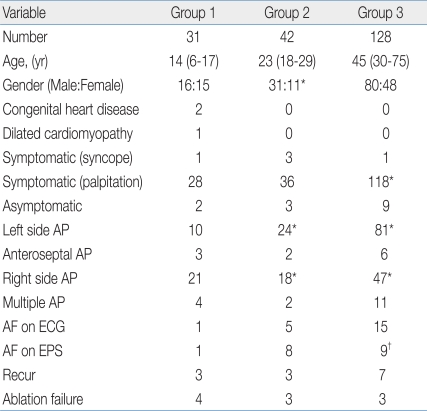
The clinical and electrophysiological characteristics of patients are summarized in Table 1.
Group 1 consisted of 16 boys and 15 girls, group 2 of 31 men and 11 women, and group 3 of 80 men and 48 women. Male preponderance was statistically significant in group 2 (male:female, 31:11), there was no gender preponderance in group 1 (male:female, 16:15).
Patients in group 1 were admitted for supraventricular tachycardia in 28 cases and for unexplained syncope in 1 case. Two patients were totally asymptomatic but had an abnormal surface ECG result, which was found incidentally. Patients in group 2 were admitted for supraventricular tachycardia in 36 cases, for unexplained syncope in 3 cases, and for the evaluation of an abnormal ECG finding in 3 asymptomatic cases. Patients in group 3 were admitted for supraventricular tachycardia in 118 cases, for unexplained syncope in 1 case, and for the evaluation of an abnormal ECG finding in 9 asymptomatic cases. In group 1, two patients had congenital heart disease (Ebstein anomaly, EA) and 1 patient had dilated cardiomyopathy. The mean time for the follow-up was 13.8±16.5 months (range, 1 to 89 months) and 65% of the patients had follow-up duration below 12 months.
2. Electrophysiological data
In terms of surface ECG findings, AF was showed in 15 patients ≥30 years age and 6 patients <30 years age. Five patients in group 2 and 1 patient in group 1 showed AF by surface ECG. Regarding EPS findings, AF was induced in 9 patients ≥30 years age and 9 patients <30 years age. AF induction during EPS was more frequent in group 2 (8/42) than in group 1 (1/31) or in group 3 (9/128) (P=0.069, P=0.036, respectively).
Failure to induce AV reentrant tachycardia by EPS occurred in 14% of the 201 study subjects (2 in group 1, 4 in group 2, and 23 in group 3). The failure rate was not significantly different between patients ≥30 years age (23/128) and <30 years age (6/73) (P=0.063), nor was it significantly different between groups (group 1 vs. group 2, P=1.000; group 2 vs. group 3, P=0.232; group 1 vs. group 3, P=0.168).
Left AP was detected significantly more frequently in group 2 (24/42) and in group 3 (81/128) than in group 1 (10/31) (P=0.023, P=0.002, respectively). However, no significant difference was found between groups 2 and 3 (P=0.722).
Multiple AP was detected in 17 patients (4 in group 1, 2 in group 2, and 11 in group 3, P=0.464). The incidence of multiple AP was not significantly different between patients ≥30 years age (11/128) and <30 years age (6/73) (P=1.000), and was also not significantly different between groups (group 1 vs. group 2, P=0.391; group 2 vs. group 3, P=0.523; group 1 vs. group 3, P=0.495).
An anteroseptal AP location, which is known to be associated with the risk of complete AV block 18,19) was detected in 11 patients (3 in group 1, 2 in group 2, and 6 in group 3). The incidence of anteroseptal AP was not significantly different between patients ≥30 years age (6/128) and <30 years age (5/73) (P=0.532), or between groups (group 1 vs. group 2, P=0.645; group 2 vs. group 3, P=1.000; group 1 vs. group 3, P=0.379).
ERP of the AP was measured in 20 subjects (4 of the group 2, 16 of the group 3). ERP of the AP showed positive correlation with age, but it was not significant (P=0.093).
After RFA of the AP, 13 of the study subjects showed recur of their WPW syndrome (3 in group 1, 3 in group 2, and 7 in group 3). Of the three recurred patients in group 1, 2 had right AP and 1 had left AP. The three recurred patients in group 2 had right AP, and of the seven recurred patients in group 3, 4 had right AP and 3 had left AP.
Ablation failure was occurred in 10 patients (4 of group 1, 3 of group 2, 3 of group 3). The localizations of the APs associated with ablation failure in group 1 were anteroseptal in 2, posteroseptal AP in 1, and lateral in one, in group 2 were anteroseptal in 3, and in group 3 were right sided in 3.
Discussion
In this study, the characteristics of pediatric WPW syndrome are; 1) no gender preponderance and 2) less incidence of left sided AP than in any other age group.
WPW is a developmental anomaly as well as a congenital anomaly20), and WPW syndrome in infancy often disappears and may recur in later childhood21,22). Epidemiological studies suggest that the prevalence of WPW syndrome is significantly lower in children aged 6 to 13 years (0.07%) than in those aged 14 to 15 years (0.17%)23).
Previous studies have also reported gender preponderance for WPW syndrome according to age. One study reported that the male proportion of WPW syndrome was 43% in children aged 6 to 7 years, 50% in children aged 12 to 13 years, and 56% in those aged 14 to 15 years23). Although there are twice as many men as women in the adult WPW syndrome population, no male predominance was found in children23). Another study also reported that the male proportion among WPW syndrome patients was 47% in children aged 14 years or less, 60% in children aged 15 to 16 years, and 69% in those aged 17 years or more24).
In previous studies, the AP ERP increased with age and nature of AP conduction changed13-17), and this is particularly well known in young children. In the present study, we did not evaluate the refractoriness of the AP in the majority of the patients, because the main purposes of EPS in WPW syndrome patients are the detection, localization, and ablation of APs. However, in 20 patients whose the AP ERP was checked, the AP ERP showed positive correlation with age although it was not statistically significant. In relation to the property of the AP ERP, the risk of AF increases with age25). Our study showed lower frequencies of AF by surface ECG and AF induced by EPS in pediatric patients, although these did not differ significantly from that observed in adults. About the more frequent AF induction during EPS in group 2 than in group 3, we think that it may be affected by artificial and aggressive pacing technique and it is questionable whether it is the characteristics for young adult with WPW syndrome.
In addition, the present study showed that the detection of left side AP was less frequent in children and adolescents with WPW syndrome. A previous study on elderly patients with WPW syndrome revealed that left lateral AP was more frequent and AF was induced more in older patients (>60 years of age)26). The present study also showed similar results, that is, left AP was more frequent in patients ≥18 years age (105/170) than <18 years age (10/31).
The anteroseptal location of AP, which is associated with a risk of complete atrioventricular block, was not found to differ significantly with age. However, a previous study reported that an anteroseptal AP location is more frequent in children than in adults and that its incidence decreases after 40 years of age 18,19).
In the present study, 3 children and adolescents with WPW syndrome had combined heart disease, but adults had none. Of these three, 2 patients had EA with right side AP and 1 patient had dilated cardiomyopathy with right side AP. All underwent successful RFA. In a previous study, it was reported that patients with EA showed only right-sided APs, and it was suggested that this might be due to malformation of the right side heart in EA27). In this previous study, five of nine patients who underwent RFA of AP were completely symptomfree after the procedure.
Regarding ablation failure cases, most cases in our study had right side APs. For right side AP, due to the structure of the right heart, it might be difficult to keep the tip of the ablation catheter on the annular portion during radiofrequency current application as firmly as during RFA of a left side AP. Therefore, RFA of right side AP requires more radiofrequency current application than left side AP and the process is more frequently interrupted.
The limitations of the present study are a short term follow-up period and a lack of an EPS on AP. Furthermore, we need to perform longerterm follow-up on our patients and to study changes in the characteristics of AP by age.
In conclusion, the present study describes several different electrophysiological characteristics in children and adolescence with WPW syndrome. Therefore, when EPS and RFA are performed in children and adolescence with WPW syndrome, we recommend that these characteristics be considered.