Regionalization of neonatal intensive care in Korea
Article information
Abstract
In the current era of low-birth rate in Korea, it is important to improve our neonatal intensive care and to establish an integrative system including a regional care network adequate for both high-risk pregnancies and high-risk newborn infants. Therefore, official discussion for nation-wide augmentation, proper leveling, networking, and regionalization of neonatal and perinatal care is urgently needed. In this report, I describe the status of neonatal intensive care in Korea, as well as nationwide flow of transfer of high-risk newborn infants and pregnant women, and present a short review of the regionalization of neonatal and perinatal care in the Unites States and Japan. It is necessary not only to increase the number of neonatal intensive care unit (NICU) beds, medical resources and manpower, but also to create a strong network system with appropriate leveling of NICUs and regionalization. A systematic approach toward perinatal care, that includes both high-risk pregnancies and newborns with continuous support from the government, is also needed, which can be spearheaded through the establishment of an integrative advisory board to propel systematic care forward.
Introduction
The fertility rate in Korea has reduced to 1.149 per woman of childbearing age in 2009, which is one of the lowest in the world1). This low birth rate is emerging as one of the nation's most serious problems in Korea. Recently, the average age of mothers giving birth has significantly increased due to social and economic changes, and the fertility rate is dropping with this increasing maternal age2). In addition, the increased use of recently developed assisted reproductive technologies has led to a simultaneous increase in multiple and preterm births3). Providing adequate neonatal intensive care for high-risk newborns is essential for decreasing their mortality and morbidity, which ultimately reduces the future costs for their morbidity of whole nation. Therefore, in the current period of low birth rate, absolute increases in the number of high-risk newborns, including premature and low-birth weight infants, requiring neonatal intensive care, has to be considered as the nation's most urgent health problem. Solving this problem requires a systematic national health plan, which needs to be established and followed as soon as possible. Most developed countries, including the United States (US) and Japan, despite having higher fertility rates compared to Korea, have already recognized the importance of improvement and regionalization of neonatal intensive care. Governments in many developed countries systemically support and manage the neonatal intensive care and the linked perinatal centers, and provide a health care system in which high-risk pregnancies and high-risk newborns can be treated adequately and efficiently, in a timely manner. To deliver efficient perinatal and neonatal intensive care, the governments have built a network through nationwide regionalization.
The neonatal intensive care unit (NICU) in Korea has been developed since the 1980s and there has been much progress until now. However, there is still a lack of a large number of NICU beds. Moreover, sufficient official investment and discussion for achieving a well-distributed nationwide network and regionalization has not been undertaken yet.
Recently, the Committee for Data Collection and Statistics in the Society of Korean Neonatology has undertaken the survey for the nationwide status of NICU in 2010 with the support of the Management Center for Health Promotion4). Here, a short review of the status of neonatal care in developed countries, including the US and Japan, and the current condition for networking and regionalization of neonatal intensive care in Korea are described.
Status and regionalization of neonatal intensive care in the US
In the US, more than 30 years earlier than in Korea, in 1970s, management and regionalization of not only neonatal intensive care, but also perinatal care, including high-risk pregnancies, was systemized and established5). The system focused on decreasing perinatal morbidity and mortality, along with providing high quality of care for high-risk pregnancies and high-risk newborns by the most efficient use of facilities and equipment, as well as highly trained personnel, and maximizing the effect of medical resource investments6). In 1975, the perinatal and neonatal management was classified into 3 levels under the motto "Toward Improving Outcome of Pregnancy (TIOP)" (Committee on Perinatal Health, 1975)5,7) as follows.
-
<Level I: Primary medical center>
Pregnancies without complications
Nursery for normal newborns and newborns with minor medical problems
-
<Level II: Secondary medical center>
Pregnancies with mild complications
Neonatal intensive care unit for newborns with moderate medical problems
-
<Level III: Tertiary medical center>
Pregnancies with severe complications
Neonatal intensive care unit for newborns with severe medical problems.
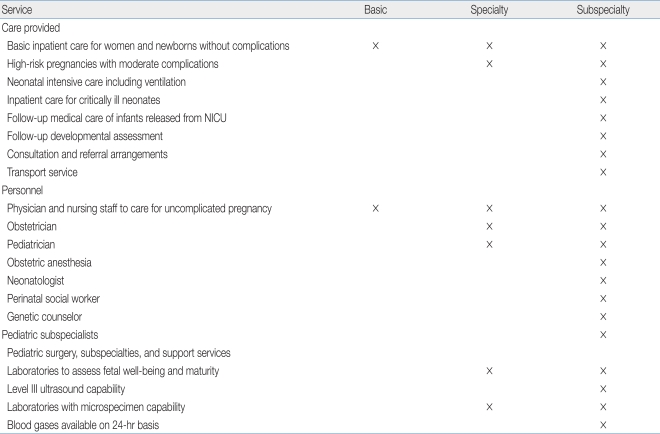
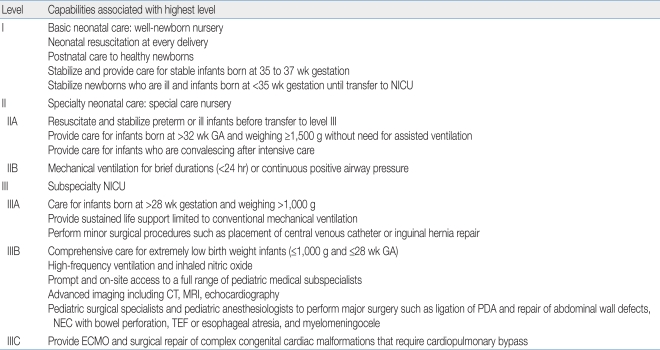
Quantitative and qualitative improvement in NICUs, as well as NICU regionalization, resulted in integrative improvement of neonatal intensive care around the nation. In 1993, TIOPII (Toward Improving Outcome of Pregnancy II, The 90s and Beyond) was launched to emphasize the importance of integrated and regionalized care system and classify the previous classification in more detail (Committee on Perinatal Health, 1993)8,9). The levels of perinatal (Table 1)9) and intensive neonatal care treatment recently used in US are as following (Table 2)10). Newborn transfer system holds a great value in the regionalized medical system. Transfer between levels I, II and III neonatal care centers is an important tool used to effectively distribute medical resources around the region. Transfer team is composed of nurses, respiratory treatment personnel, neonatal care doctors, residents or by other personnel, and ambulances, helicopters and fixed-wing aircrafts were being used as transport vehicles11). Following the introduction of a centralized neonatal transfer service, response times improved significantly12).
Status and regionalization of neonatal intensive care in Japan
Neonatal care in Japan was supported by the government early on. Medical support for premature infants and reporting system for low-birth weight infants were introduced in 1958. In 1979, parts of obstetric and pediatric departments were combined as perinatal care system and operated regionalized perinatal medical centers based on the "Regionalization of neonatal care to improve newborn death rate" project. In 1984, Maternal Fetal Intensive Care Unit was set up as perinatal care units. In 1991, "Doctor Car" was first introduced to operate ambulances that focus on transfer of high-risk newborns between the medical centers. In 1995, Maternal and Child Health Law was revised and from the following year, one general perinatal care medical center per 1 million began to be built around the nation. These medical centers have been maintained and supported until today. A total of 242 regional perinatal care centers and 77 integrated general maternal-fetal medical centers now serve as the backbone of Japan's perinatal care. Three central (super) perinatal care units were established in the most populated regions of Tokyo to deal with the highest-risk pregnancies and neonates from the entire nation13). A total of 80 million Yens (Japanese currency) (1 billion KRW [Korean currency]) for regional centers, 140 million Yens (1.8 billion KRW) for integrated general centers, and 190 million Yens (2.5 billion KRW) for central centers are being supported by the government14).
According to the Ministry of Health and Welfare in Japan, the Japanese government allocated 1.7 billion Yens (17.9 billion KRW) for the care of premature infants and 2.3 billion Yens (24.4 billion KRW) for perinatal care. The support and network for perinatal care is still increasing in Japan15).
The death rate of low-birth weight newborns has been decreasing for the past 30 years in Japan due to continuous and systemic efforts driven by the government. The survival rate of extremely-low-birth weight newborn infants (<1,000 g) that requires the highest intensive care was improved from 44.7 in 198016) to 83.0% in 200517). Currently, 80% of newborns survive regardless of their birth weight and finally, Japan currently has the lowest premature infant death rate in the world.
Status and regionalization of neonatal intensive care in Korea
1. Changes in the number of total and regional NICU beds
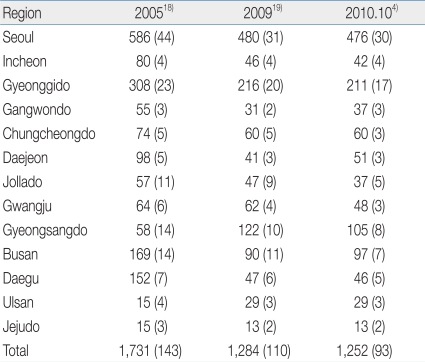
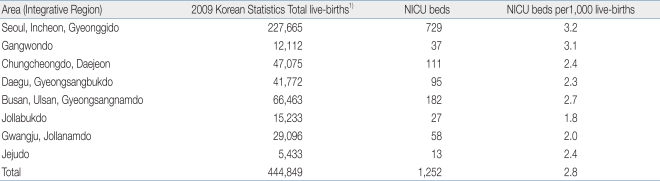
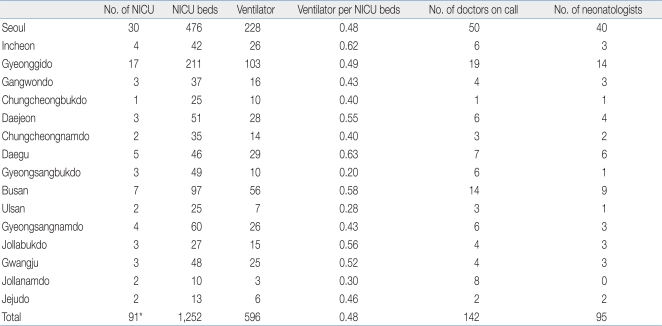
From the national survey of the Committee for Data Collection and Statistics in the Society of Korean Neonatology for NICU status reported at October, 20104), number of real operating NICUs was 93 hospitals and operating NICU beds were 1,252. Compared to previous reports in 200618), the 2010 survey showed markedly decreased operating NICUs and NICU beds throughout the nation. Although a few NICUs and NICU beds were added or expanded due to regional demands, with or without support from the government, such as the project of "Regional NICU expansion" and "Regional Children's Hospital" of the Ministry of Health and Welfare, a considerable number of NICUs have been closed or cut in size over the last 5 years (Table 3). The reasons behind this reduction were manifold. First, the inability of the hospital running the NICU to meet the requirement of legal NICU classification and standards for the facility and manpower enacted in 2006, thereby closing their NICU or reducing the number of beds. Secondly, a reduction in the number of obstetrical staff, which led to a decrease in deliveries, and a lack of medical staff available to treat high-risk newborns in NICU also led to the decrease in of functioning NICU beds. All of the regional operating NICU and NICU beds were reduced, except in the Gyeongsangdo and Ulsan areas, as shown in Table 3.
2. Shortage of regional beds and medical resources of NICU
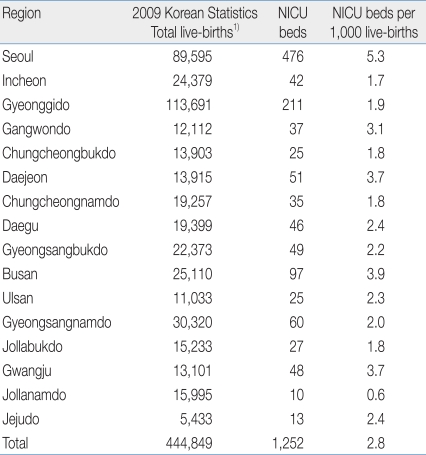
There were 444,849 total live births in 2009, in Korea1). Comparison of the number of regional NICU beds to the total number of regional live births is shown in Table 4. Number of NICU beds are 0.3 to 5.3 per 1,000 live births, depending on the region, with large variability. Seoul has the highest number of beds and Jollanamdo has the lowest number of beds. Large cities such as Seoul, Daejeon, Busan, and Gwangju have more than 3.2 beds per 1,000 live births. However, the number of beds is very small in regions neighboring the 4 areas Gyeonggido, Chungcheongnamdo, Gyeongsangnamdo, and Jollanamdo. When the regions are classified based on larger geographical features, or areas (Table 5), variability in the number of NICU beds are slightly decreased, to 1.8 to 3.2 per 1,000 live births, depending on the area. It can be expected that high-risk newborns are being transferred to neighboring regions. For instance, Seoul may be used to compensate for the required beds in the Gyeonggido region.
On the scope of medical resources, Gyeongsangbukdo, Ulsan, and Jollanamdo, still have less than 0.3 mechanical ventilators per NICU bed (Table 5), and only 1 or 0 neonatologists (Table 6), as well as the lowest number of NICU beds per 1000 live births amongst all the national regions. Therefore, those regions do not have enough medical resources to provide adequate emergency neonatal intensive care.
According to the national survey report for 200618) and 20104), 3.2 to 3.4 neonatal intensive care beds are needed per 1,000 live births, and 4.1 to 4.5 beds per 1,000 live births are needed, including the operation of supplementary beds. Therefore, more than 1.0 bed per 1,000 live births is needed in all of the regions, and even more in larger areas. Therefore, it is required to increase the number of beds and medical resources, including medical equipment and manpower, nationwide with proper allocation for the establishment of regionalization and network for neonatal care.
3. Transfer flow of high-risk newborn
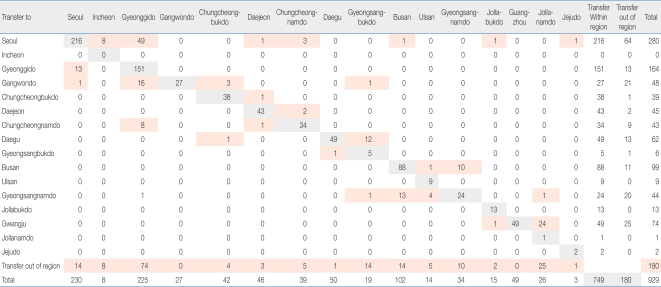
Table 7 shows the flow of 929 neonatal patients in July 2010, reported in the 2010 survey4). When the nation is divided into 16 regions by cities and provinces, 749 newborns (80.6%) were transferred within the region and 180 newborns (19.4%) were transferred out of region. Therefore, approximately 20% of the high-risk newborns were transferred out of the region. If the nation was divided into 8 integral areas by grouping: Seoul, Incheon, and Gyunggido as Region 1; Gangwondo as region 2; Chungcheongbukdo, Chungcheongnamdo, and Daejeon as Region 3; Daegu and Gyeongsangbukdo as Region 4; Jollabukdo as Region 5; Gwangju and Jollanamdo as Region 6; Gyeongsangnamdo, Busan, and Ulsan as Region 7; and Jejudo as Region 8. Except the transfer to Seoul from all other integral regions, all of the transfers were made within each integral area. Therefore, in the future, regionalization of neonatal intensive care has to be set up by establishment of integral area NICU centers with careful consideration of proximity of neighboring regions, availability of traffic routes, and effective use of available beds. It is also evident that there are special needs for transfer of high-risk newborns, because of the need for highly-selective specialized surgery or high-end specialized care, or of lack of availability of regional NICU beds for super-emergent cases. Like super perinatal care centers in Tokyo, Japan, we need to create national integrative care centers to serve the purpose of high-end and super-emergency neonatal care, and a final referral center. Since very large NICUs that handle more than 100 very-low birth weight newborn infants are located in Seoul, rather than to expand NICU beds in the Seoul area, it is advisable to set up or use big centers in Seoul as the final referral super center for the entire nation. Moreover, it is important to create a network with other regional and more integrative area NICUs around the nation. There is a need to classify the level of neonatal intensive care units in Korea, like in the US. Therefore, it is needed to effectively distribute the medical resources for neonatal care through proper leveling, regionalization and networking of neonatal care in Korea.
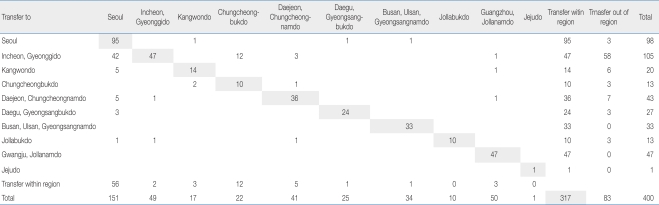
4. Transfer flow of high-risk pregnancies
Table 8 shows the transfer flow of high-risk pregnancies during 2 weeks of July 2010, reported in the 2010 survey4). A total of 400 high-risk pregnant women were transferred to other hospitals and 83 patients (21%) were transferred out of region. Among 447 transfer contacts, 311 patients (69.6%) were actually accepted in the first hospital/ medical center to which they were requested for being transferred; however, 127 patients were denied their transfer in the first contact to transfer. The reason for denying the transfer was, 50% due to lack of NICU beds, 29.3% due to unavailability of mechanical ventilator in the NICU, 7.1% due to difficulties in surgery and special care, and 5.0% due to lack of medical personnel resources in NICU and delivery room. The transfer flow of high-risk pregnant women was very similar to transfer flow of high-risk newborns. Approximately 20% of the patients were transferred out of region and 70% of the patients were accepted on the first hospital/medical center to which they were requested for being transferred whereas the remaining 30% were wandering to find a hospital for their care. Since most of the denials for transfer were due to lack of medical resources in the NICU, management of high-risk pregnancies and high-risk newborns cannot be separated from one another. A perinatal approach, that includes both high-risk pregnancies and newborns, is needed when establishing the policies for their care.
Conclusion
Neonatal intensive care for high-risk newborns is a major health issue that should be supported by the government, as discussed in the cases of the US and Japan. Neonatal intensive care policies of advanced countries may be summarized as follows. First, the policies accommodate perinatal care and transport systems, including high-risk pregnant women and high-risk newborns. Second, the policies level and regionalize the high-risk newborn infant care system using expert groups and instating clear legislation. Third, there is continuous support from the government for systematically constructing high-risk neonatal and perinatal care systems. Fourth, there is an effective distribution and use of medical resources, by establishment of a clear transfer system and regionalization.
In Korea, it is evident that there is a shortage of NICU beds and medical resources nationwide, with varying degrees across regions, and a lack of systemic perinatal and neonatal regional networking. In the recent analysis on transferred high-risk newborns and pregnant women, about 20% were transferred beyond their location, while most of them were transferred in the vicinity of their original location. Seoul tended to have patients transferred from all the parts of the country. As most high-risk newborn infants are transferred within the neighboring region, regional care centers should be upgraded, and there seems to be a need to bolster a few national central centers in Seoul for taking care of patients transferred from other regional medical centers, to provide challenging high-end treatments. The main cause for the transfer of high-risk pregnant women was the deficits of beds and medical resources of NICU, which were the same deficits that applied to high-risk newborn transfers. The success rate of transfers was only about 70%. Ultimately, to complete the health care system of high-risk newborns in the era of low-birth rates, an absolute increase in the number of NICU beds, along with proper equipment, facilities, and manpower, and the completion of proper transfer system through regionalization and leveling of NICUs are needed. Further, a systematic approach toward perinatal care that includes both high-risk pregnancies and newborns is needed, as well as the establishment of an integrative advisory board to drive the momentum of systematic approach. Establishment of regionalized perinatal centers, including those that can accommodate high-risk pregnancies and neonatal intensive care through a nationwide network will result in improving the outcome of high-risk newborns. Such a system will help improve the health and save the lives of thousands of newborns and provide an effective solution for low-birth rate issues in Korea.
Acknowledgement
This study was supported by the Health Promotion Fund, Ministry for Health, Welfare and Family Affairs, Republic of Korea (Policy 10-11).