Clinical characteristics of obese boys and girls in a high school: focused on abdominal fat indices, fatty liver and carotid intima-media thickness
Article information
Abstract
Purpose
Our study aimed to evaluated sex differences in clinical features of obese high school students.
Methods
One hundred three obese high school students (body mass index [BMI]≥85th percentile) and 51 control students (BMI<85th percentile) were enrolled in this study. Anthropometric measurements were performed. Fasting serum glucose, insulin, aspartate aminotransferase, alanine aminotransferase, total cholesterol, triglyceride, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and high-sensitive C-reactive protein were measured. Abdominal fat thickness, degree of fatty liver, and carotid intima-media thickness were measured by ultrasound.
Results
In control and obese groups, waist circumference was significantly longer in boys but body fat mass was significantly higher in girls. In the control group, total cholesterol and LDL-C were higher in girls. In the obese group, however, aspartate aminotransferase, alanine aminotransferase and triglyceride were higher and HDL-C was lower in boys. Preperitoneal fat thickness was significantly higher in obese girls. In obese group, the degree of fatty liver was significantly higher in boys. Carotid intima-media thickness was not significantly different between boys and girls.
Conclusion
Obese adolescents had distinguishable sex differences in body measurements, metabolic abnormalities, abdominal fat thickness and fatty liver. We can infer that these characteristics may extend into adult obesity.
Introduction
Recently in Korea, childhood and adolescent obesity has increased rapidly because of socio-economic development, westernization of eating lifestyles, and the increased use of computers. Obesity leads to complications such as hypertension, hyperlipidemia, insulin resistance, and non-alcoholic hepatitis. The prevalence of these complications has increased and they are life-threatening factors on adolescent health, on which lifelong health is based. Childhood obesity ultimately contributes to the prevalence of adult diabetes, hypertension, and cardiovascular disease.
Marked sex differences have been reported in regards to the degree of insulin resistance, body composition and energy balance in adults1). Adolescents in high school present some features like abdominal fat distribution of both childhood and adulthood. To date, most researches have focused on adolescent obesity itself without mentioning sex differences. Physiological changes during this period include increased secretion of sex hormone and growth hormone, and the development of insulin resistance, which influences differences in sex hormone and subcutaneous fat between the two sexes2-5).
In this study, we evaluated clinical features of obese high school students according to the sex, and we focused on the finding relations between metabolic index, cardiovascular risk factors and abdominal fat indices.
Materials and methods
1. Subjects
One hundred fifty four students (68 boys, 86 girls) aged between 15 and 17 in a high school participated in this study. They were divided into two groups: the obese group and control group. The obese group (48 boys, 55 girls) included those who had body mass index (BMI) above the 85th percentile for age and sex and the control group (20 boys, 31 girls) included those who had BMI below the 85th percentile for age and sex by the survey of Korean Centers of Disease Control and Prevention in 2007. Persons with endocrine dysfunction or other illnesses were excluded. We obtained informed consents from the guardians after explaining the procedure and purpose of the test thoroughly, and the study was approved by the Institutional Review Board.
2. Methods
1) Anthropometric measurement
We obtained height, weight, BMI, and body composition with Segmental Multi-frequency Bioelectrical Impedance Analysis (InBody J10, Biospace, Seoul, Korea). Waist circumference was measured with a tapeline at the expiratory phase on the horizontal plane between the lowest margin of the 12th rib and the mid portion of the superior iliac crest to the nearest 0.1 cm on standard physician's beam scales, and hip circumference was measured from the most protruding part of the hip to the nearest 0.1cm on standard physician's beam scales.
2) Blood pressure measurement
We checked each subject's blood pressure in his/her right arm with a standard mercury sphygmomanometer. A cuff with a width that encircles 40 to 50% of the upper arm was chosen. After the subject was stabilized for at least 5 minutes, we checked blood pressure twice and used the average.
3) Biochemical analysis
Venous blood was drawn after overnight fasting. Samples were kept at -70℃ for subsequent assay. The serum concentrations of glucose, insulin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), total cholesterol, triglyceride (TG), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and high-sensitive C-reactive protein (hs-CRP) were evaluated.
4) Abdominal ultrasound for abdominal fat indices and fatty liver
We used abdominal ultrasound Acuson XP128 (Acuson, Mountain View, CA, USA) and placed it above the navel and measured abdominal fat thickness including subcutaneous fat thickness, visceral fat thickness and preperitoneal fat thickness. The measurements were taken by an experienced radiologist. The subjects were comfortably placed in a supine position and we measured subcutaneous fat thickness from skin to anterior abdominal muscle, visceral fat thickness from posterior abdominal muscle to abdominal anterior wall of aorta, and preperitoneal fat thickness from the subcutaneous layer to the peritoneum, by placing a 3.5 MHz linear-array probe 1 cm above the navel at the end-expiratory phase. Fatty liver grading was recorded: grade 0 - no fatty liver; grade 1 - mild; grade 2 - moderate; and grade 3 - severe6).
5) Carotid artery ultrasound
Carotid intima-media thickness (IMT) was measured when the subjects were supine for at least 30 minutes with neck ultrasound iU22 (Intelligent Ultrasound System, Philips Medical System, Amsterdam, The Netherlands) on 3 points of the thickest part of the intima-media 1 cm below, and the average was recorded.
6) Statistical analysis
The average and standard deviation of all measurements were collected. Statistic analysis between the groups was processed using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). We used the Mann-Whitney nonparametric method to compare the average between the obese group and the control group. The degree of the fatty liver in obese group was compared between boys and girls using Chi-square test. Spearman's rho nonparametric correlation analysis was used to confirm the relationship between cardiovascular risk factors and visceral fat thickness measured by ultrasound. A P value of less than 0.05 was regarded as significant.
Results
1. Anthropometric analysis
In control and obese groups, there was no significant difference of BMI between boys and girls, but waist circumference, waist-hip circumference ratio and blood pressure were higher in boys than in girls. However, body fat mass and body fat percentage were significantly higher in girls than in boys in both groups (Table 1).
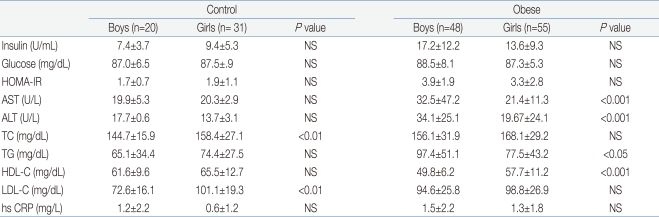
2. Biochemical analysis
In the control group, there was no significant difference in insulin, glucose, homeostasis model assessment of-insulin resistance (HOMA-IR), AST, ALT, TG, HDL-C and hs-CRP between boys and girls, but total cholesterol and LDL-C were higher in girls than in boys. In the obese group, there was no significant difference in insulin, glucose, HOMA-IR, total cholesterol, LDL-C and hs-CRP between boys and girls, but AST, ALT and TG were higher and HDL-C was lower in boys than in girls (Table 2).
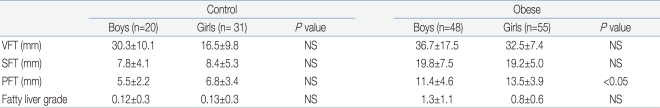
3. Abdominal fat thickness and fatty liver
In the control group, visceral fat thickness, subcutaneous fat thickness and preperitoneal fat thickness showed no significant sex difference. In the obese group, there was no significant sexual difference in visceral fat thickness and subcutaneous fat thickness but preperitoneal fat thickness was significantly larger in girls than in boys (Table 3).
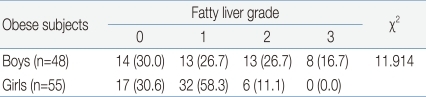
In obese group, the degree of fatty liver was thicker in boys compared to girls but, there was no significant difference between boys and girls. However, cross-analysis of the degree of fatty liver in the obese group showed that boys had a higher degree of fatty liver compared to girls (Table 4).
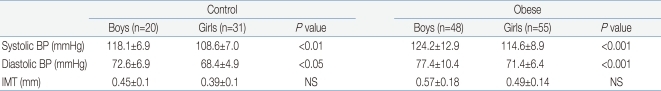
4. Blood pressure and carotid intima-media thickness
In control and obese groups, systolic and diastolic blood pressure was higher in boys than in girls. In control and obese groups, carotid IMT was higher in boys than in girls but there was no significant difference (Table 5). In obese group, the incidence of carotid IMT over 0.6 mm, which is over the 2 standard deviations of carotid IMT of the control group, was higher in boys (26.7%) than in girls (16.7%) but there was no significant difference.
Discussion
For a given body mass index, men are reported to have more lean mass, and women to have higher adiposity7). Men are also found to have more visceral and hepatic adipose tissue, whereas women have more peripheral or subcutaneous adipose tissue. These differences as well as differences in sex hormones and adipokines may contribute to the more insulin-sensitive environment in women than in men8). In our study, although the BMI between boys and girls are not different in control and obesity group, waist circumference and waist-hip ratio were higher in boys but fat masses were higher in girls.
BMI is commonly used as a tool for the evaluation of obesity, but cannot discriminate body fat and muscle mass, and is inaccurate in that it is correlated more with subcutaneous fat than with abdominal fat, which is linked to metabolic disorders. Abdominal visceral fat is known to be a risk factor of insulin resistance and diabetes in both men and women. Waist circumference is easy to estimate and is a common index for epidemiologic research, but is not a direct reflection of visceral fat because abdominal fat is divided into visceral fat and subcutaneous fat. To measure visceral fat correctly, waist circumference, waist-hip circumference ratio, and the length of abdominal median-plane should be used together as they are simple and non-invasive anthropometric methods9).
It has already been reported that waist circumference is more closely correlated with hypertension or metabolic disorder and insulin resistance compared to BMI10). Waist circumference is a good parameter for abdominal obesity, but cannot always be related with cardiovascular risk because waist circumference has a high correlation not only with visceral fat but also with subcutaneous fat11).
Abdominal fat, especially, visceral fat is known to be a risk factor of metabolic disorder, which increases the degradation of fatty acid and is related to the increase of insulin resistance, and visceral fat cells secrete many cytokines and increase the cardiovascular factor12).
Visceral fat and subcutaneous fat have not only a histological difference but also a difference in metabolic activities: visceral fat is more sensitive to lipolysis by catecholamine than to the anti-lipolytic effect of insulin13). Visceral fat transfers fatty acid to the portal circulation, increases glucogenesis and LDC, and reduces insulin degradation in the liver. As abdominal fat lipolysis increases, fatty acid in the portal and systemic circulation increases and finally induces hyperlipidemia, glucogenesis, and insulin resistance14). Visceral fat is known to increase with age and weight gain in both boys and girls. The waist-hip ratio is generally higher in boys, and it seems that visceral fat is larger in boys compared to girls15). In our study, waist circumference and waist-hip ratio were higher in boys than in girls, but body fat mass was larger in girls than in boys, which is similar to the distribution of body fat mass in adults. In addition, it is known that men have much more visceral fat and much less subcutaneous fat than women8,16). Our study revealed that abdominal fat thickness measured by ultrasound was thicker in boys than in girls among high school students but the difference was not significant. Subcutaneous fat thickness and preperitoneal fat thickness were higher in girls than in boys but were not significant. We think that the characteristic difference of fat distribution between normal men and women may be altered by obesity in adolescence. In the regulation of growth and development of puberty, estrogen and growth hormone interact closely. During growth spurt, estrogen and growth hormone take an action and change the physical development and then make a result sex different body composition change17).
Adolescent obesity is known to be a major risk factor of non-alcoholic fatty liver and atherosclerosis, and combined with hyperlipidemia, hypertension, elevation of liver enzymes, and insulin resistance. Non-alcoholic steatohepatitis is a chronic liver dysfunction and has been reported to progress finally to fibrosis, hepatocirrhosis18). Jang et al.19) reported that obese first-year high school students have an abnormal ALT level, 23.7% in boys and 11.8% in girls. In the obesity group, boys had a statistically higher abnormal rate of AST, ALT, and total cholesterol, but in the normal weight group, the abnormal rate of AST, ALT, and total cholesterol was significantly higher in girls than in boys. In a large cohort of overweight and obese European children and adolescents, the markers of nonalcoholic liver disease, especially elevated ALT, were frequently predicted by severe obesity group and male gender20,21).
Recent studies study about estrogen effect to obesity. Pediatric non-alcoholic steatohepatitis is common in boys22) and this sex difference may be due to the defense mechanism of estrogen as non-alcoholic steatohepatitis appears to be more common in menopause women than in premenopausal women as estrogen can reduce the oxidation of fat20).
We can elude that lipid metabolism of sex steroid may start from the adolescent period; eventually these differences can be related with sex steroid, cytokine and lipid metabolism. The association of elevated ALT in obese boys supports the hypothesis that the pubertal increase of sex steroid may be important in predisposition for pediatric non-alcoholic steatohepatitis22). The underlying mechanisms of sex difference appeared to be due to the change of gene expression, which is dependent on estrogen. Estrogen reduced reactive oxygen species with increased antioxidant gene expression and reduced proinflammatory cytokine production24).
Nonalcoholic fatty liver disease (NAFLD) is a disorder associated with obesity. Studies reported the prevalence rate of suspected fatty liver in overweight children between 6 and 23%25).
Interestingly, epidemiological studies and most of published case series demonstrate a clear male predominance in the diagnosis of nonalcoholic fatty liver disease. In this study, the incidence of fatty liver in obese adolescents measured by ultrasound was 30% in both sexes. However, compared to the severity of fatty liver, the boys showed a mild to severe degree but the girls showed mostly a mild or moderate degree and no severe degree. This led to the assumption that estrogen might be an important mediator in the pathogenesis of nonalcoholic fatty liver disease. Changes in estrogen metabolism and physiological insulin resistance may determine susceptibility to fatty liver disease and contribute to the gender-specific prevalence pattern which is supported by previous studies26,27).
Carotid intima-media thickness is a measure of subclinical atherosclerosis and predictive of future myocardial infarction and stroke. Obesity during childhood has been associated with higher carotid IMT during adulthood28,29). Caserta et al.30) reported that NAFLD, BMI, waist circumference, and systolic blood pressure are independent markers of increased IMT in a random sample of adolescents.
Lee et al.31) reported that obesity in adolescence was related to an increase in carotid IMT among healthy young Korean men but not in women. In our study, the incidence of carotid IMT over 0.6 mm, which is over the 2 standard deviations of carotid IMT of the control group, was higher in obese boys (26%) than in obese girls (16.7%) but there was no significant difference.
Limitations of this study were first, only 154 of a high school in Seoul were included and the number of the objectives was small. Second, although, the mean BMI of boys was not different from that of girls, we did not adjust the BMI on the results statistically.
In conclusion, comorbidities of obesity in adolescents are more prevalent and severe in the male sex. We can infer that these characteristics reflect some parts of adult obesity.
Notes
This study was supported by a grant from Korean Heart Research Foundation (2008).