A case of pyogenic liver abscess in a 10-year-old girl
Article information
Abstract
Pyogenic liver abscesses are rare in children. In pediatric patients, altered host defences seem to play an important role. However, pyogenic liver abscess also occurs in healthy children. We experienced a case of pyogenic liver abscess in a healthy immunocompetent 10-year-old-girl. The patient presented two distinct abscesses: one subphrenic and the other intrahepatic. The intrahepatic abscess resolved with percutaneous drainage and 3 weeks of parenteral antibiotic therapy but the subphrenic abscess which could not be drained needed prolonged parenteral antibiotic therapy in addition to oral antibiotic therapy. We performed follow-up serial CT scan of the abscess cavity to decide on the duration of antibiotic therapy. Here we present this case with a brief review of the literature.
Introduction
Pyogenic liver abscess (PLA) is a rare pediatric disease across geographic regions1-3). Typically, PLA is found in adults with biliary disease2, 3). In Korea, articles about PLA in children have rarely been published1). In developed countries, PLAs occur most frequently in immunocompromised hosts and in infections originating within the abdominal cavity3, 4). Advances in imaging techniques and treatment by drainage of the liver abscess and new antibiotics, have decreased the morbidity and mortality of PLA. Nevertheless, in a recent series of studies, mortality in PLA has been found up to 15%3, 5). Opinions vary on the proper duration of intravenous and oral antibiotics for pediatric PLA therapy3-5), which differs from that needed by adults6, 7). This case describes a immunocompetent 10-year-old girl presenting with pyogenic intrahepatic and subphrenic abscesses without underlying disease. We performed follow-up serial CT scan of the abscess cavity to decide on the duration of antibiotic therapy.
Case report
A 10-year-old girl was admitted to Konkuk University Medical Center for evaluation of a hepatic mass. She was previously healthy and had no notable travel or food history. There was no family history of inherited diseases or immunological disorders. 10 days before admission, fever and right upper quadrant abdominal pain had developed. There were no other gastrointestinal complaints, including vomiting or diarrhea. Abdominal ultrasonograpy (US) at local pediatrics revealed a hepatic mass. Her body temperature was 37.4℃, heart rate was 110 beats/min, blood pressure was 110/57 mmHg, and respiratory rate was 24 beats/min. On admission, both scleras were clear, and neither her liver nor spleen were palpable. Right upper quadrant tenderness was examined but rebound tenderness was not. The laboratory findings on admission day were Hb 12.4 g/dL, Hct 35.7%, WBC 10,660/mm3 (neutrophil 75.6%, lymphocyte 20.0%, monocyte 3.1%, eosinophil 0.9%), platelet 199,000/mm3, ESR 75 mm/h. The blood chemistry showed AST/ALT 26/37 IU/L, total bilirubin 0.3 mg/dL, total protein 8.1 g/dL, albumin 4.0 g/dL, alkaline phosphatase 321 IU/L, r-GT 76 IU/L, alpha-fetoprotein 1.47 ng/mL, CRP 2.98 mg/dL, and amoeba Ab <1:8. Culture of blood was negative. A chest radiograph showed an elevated right hemidiaphragm. An abdominal CT scan revealed a 36×31 mm pocket of multiloculated fluid on the right liver dome and a 38×24 mm localized fluid collection on the subphrenic area (Fig. 1A).
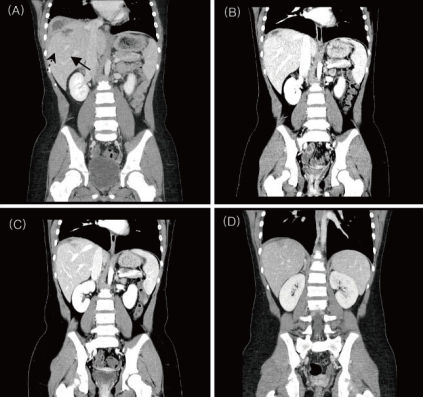
A) Enhanced CT scan on admission day shows liver abscess in the posterior aspect of the right dome (S7) of the liver (dotted arrow) and subphrenic abscess (arrow). B) The third follow-up CT scan on hospital day 22 revealed that the abscess of the right lobe was completely healed and the subphrenic abscess reduced to 10×10 mm. C) The fourth follow-up CT scan on hospital day 34 revealed granulation tissue on the S7 dome of the liver and slight improvement in the subphrenic fluid collection. D) The fifth follow-up CT scan on 74th day from the beginning of therapy shows the right dome of the liver completely healed and the subphrenic fluid collection improved over the previous CT.
On hospital day 2, the patient was treated with empiric parenteral antibiotics, metronidazole (30 mg/kg/day) and ceftriaxone (100 mg/kg/day). Drainage of the liver abscess was performed by percutaneous catheter, which was inserted in the abscess in the right dome. However, it was not performed on the subphrenic abscess because the lesion was inaccessible. Two distinct abscesses, one intrahepatic and the other subphrenic, had non-communicating pathways. The aspirate was turbid and old blood-colored. Culture of the aspirate grew penicillin-sensitive alpha streptococci. On hospital day 6, the laboratory findings were Hb 12.0 g/dL, Hct 35.5%, WBC 5,750/mm3 (lymphocyte 40%, neutrophil 52.9%), platelet 410,000/µL, ESR 40 mm/h, and CRP 0.37 mg/dL. Fever and right upper quadrant abdominal pain were improved. On hospital day 8, a follow-up abdominal CT scan showed that the abscess of the right lobe was completely removed and the abscess of the subphrenic area had decreased in size from 36×31 mm to 10×10 mm. The abscess on the right dome of the liver decreased more rapidly than that on the subphrenic area. The percutaneous catheter was removed on hospital day 9 because the amount of drainage was scanty. On hospital day 22, a subsequent abdominal CT scan revealed that the abscess of the right lobe was completely healed and the size of the liquefied abscess cavity on subphrenic area was 10 mm (Fig. 1B). On hospital day 34, the fourth follow-up abdominal CT scan revealed granulation tissue on the S7 posterior aspect of the dome of the liver and a slightly improved state of the subphrenic fluid collection than the previous result (Fig. 1C). Laboratory findings on that day were improved as follows: WBC 5,200/mm3 (neutrophil 48.8%), CRP below 0.01 mg/dL, AST 31 IU/L, ALT 27 IU/L. The patient was discharged on hospital day 34 and was swithched to oral forms of treatment. The oral antiboitics, cefpodoxime and metronidazole, were administered for 26 days. 40 days after discharge, the fifth follow-up abdominal CT scan was performed in an outpatient setting: the abscess of the right lobe was completely healed and the right posterior subphrenic fluid collection showed improvement over previous results (Fig. 1D). Nine months later, the patient is now under follow-up care without any specific problems.
Discussion
Early diagnosis and antibiotic therapy with drainage of the pus collection is the mainstay of therapy for PLA3, 4). Pediatric PLAs are difficult to diagnose8). The classic symptoms of fever, right upper quadrant tenderness, and jaundice are only present in approximately 10% of patients. Approximately half of the patients have both fever and is right upper quadrant pain2).
Drainage of the liver abscess is a core therapy, that can detect causative organisms and can shorten the treatment period. Methods of drainage include an open surgical approach, laparoscopic drainage, radiographic guided percutaneous drainage, percutaneous aspiration, and needle aspiration9). Percutaneous continuous catheter drainage is more effective, and catheters placed are generally left in place until abscess collapse, usually from 24-72 hours to 2-3 weeks3, 4).
In our case, percutaneous drainage was feasible in the intrahepatic abscess, but the subphrenic abscess was not accessible to percutaneous drainage due to its location. The sizes of the two abscesses were similar on admission. The size of the intrahepatic abscess decreased more rapidly than that of the subphrenic abscess. With percutaneous drainage and 3-week-long intravenous antibiotic therapy, the intrahepatic abscess resolved. The catheter was removed after 8 days' placement in the intrahepatic abscess. A third follow-up CT scan on hospital day 22 revealed nearly complete resolution of the intrahepatic abscess. In contrast, the subphrenic abscess in which percutaneous drainage was not feasible had to be treated with 5-week-long intravenous antibiotic therapy, and a fourth follow-up CT scan on hospital day 34 revealed residual fluid collection in the subphrenic abscess cavity. In sum, the therapeutic responses were different for the two abscesses.
Duration of antibiotic therapy in pediatric PLA is variable3-5). Antibiotic therapy is intravenous and prolonged for at least 4-8 weeks, although no evidence-based data exist to guide duration5). According to another opinion, treatment periods of 3-6 weeks are generally accepted4). In adults, antibiotic therapy is recommended intravenously for at least 2 weeks and then orally for up to 6 weeks6, 7). In a recent report on PLA in adults, sequential intravenous therapy for 3 weeks followed by oral antibiotics for 3 weeks was safe and equally effective compared with 6-week intravenous antibiotic therapy10). According to another report in children, when percutaneous continuous drainage is maintained during 2 to 4 weeks, parenteral antibiotic therapy should also be maintained for at least 2 to 4 weeks, followed by oral antibiotics for a total of 4 to 6 weeks3). This opinion coincides with the outcomes of our case, in which 3-week intravenous antibiotic therapy followed by 4-week oral antibiotics administration was necessary. However, in case the lesion is not amendable to continuous drainage, it needed to be treated with 5-week intravenous antibiotic therapy followed by oral antibiotics for 3 weeks. In light of our experience, longer than 3-week treatment may be required in multiple hepatic microabscesses or left lobe seated lesions that are not amendable to drainage.
Our patient was a 10-year-old girl with two distinct abscesses and without a underlying disease. Antibiotics and drainage led to resolution of the abscess. Our experience indicates the abscesses not amenable to continuous drainage need prolonged intravenous antibiotic therapy. Also, it is thought that relatively longer intravenous antibiotic therapy is required in pediatric PLA than in that of adults. Serial radiologic imaging of the abscess cavity and clinical response are helpful in deciding on a duration for antibiotic therapy.