Article Contents
| Clin Exp Pediatr > Volume 56(5); 2013 |
Abstract
Purpose
Sleep onset association disorder (SOAD) is a form of behavioral insomnia observed in children that is caused by inappropriate sleep training. SOAD typically disturbs the sleep of not only infants and children but also their parents. We investigated levels of depression and marital intimacy among parents of infants with typical SOAD, to understand the influence of SOAD on family dynamics, as well as examine ways for improving depression and marital intimacy through behavioral training.
Methods
Depression and marital intimacy were assessed using the Beck Depression Inventory (BDI) and Waring Intimacy Questionnaire (WIQ). These measures were administered to 65 parents of infants (n=50) diagnosed with SOAD. We conducted sleep education and behavioral training for the parents and compared levels of depression and marital intimacy after 2-6 weeks of training.
Results
The 65 parents consisted of 50 mothers and 15 fathers. Depressive symptoms were higher among mothers than fathers (P =0.007). Marital intimacy was negatively correlated with depressive symptoms. Twenty-six parents were assessed again after sleep training. We found that mothers' depressive symptoms and marital intimacy improved post training.
Conclusion
SOAD can be detrimental to both infants and parents, especially for parents who sleep with their infants. For instance, disruption of sleep patterns in such parents can reduce marital intimacy. However, behavioral modification is an effective treatment for infants with frequent nighttime waking, as well as for diminishing the depressive symptoms of sleep-deprived parents.
Sleep onset association disorder (SOAD) is a typical behavioral insomnia in children caused by inappropriate sleep training, which requires special conditioning such as feeding, rocking or swinging while falling asleep. Infants with SOAD awake according to their normal sleep cycle and can not fall asleep by themselves, and constantly demand parents' behavioral intervention1).
Infants with sleep problems are more likely to be tired, inattentive, and irritable, and have difficulty modulating their impulses and emotions2). The sleep problems also negatively impact behavior, cognition, and growth of the infant3), and disturbs the sleep of the infants and the parents. The lack of sleep induces chronic fatigue and parenting stress due to sleep deprivation, and can fuel maternal depression and diminish mother-infant relationship4,5). Maternal depression after the first birth is strongly related to the occurrence of paternal depression, which can increase familial discord and divorce6,7). Cosleeping is associated with increased night waking and sleep problems in infants8,9).
Cosleeping of infants and parents is very prominent in Korean culture and if infants awake during the night inappropriate sleep associations such as feeding and soothing are frequently executed and parents complain of persistent lack of sleep and fatigue. However, little is known concerning the effect of SOAD on the family and the depressive states of parents in Korea.
We investigated depression and marital intimacy level in parents of infants with SOAD to understand the influence of infant SOAD on the family and how the level of depression and intimacy improves with behavioral sleep training.
We conducted a survey on the infants with SOAD and their parents who visited the pediatric sleep clinic of CHA Bundang Medical Center in Seongnam, Korea from January of 2011 to June of 2012.
The inclusion criteria of the infants with SOAD followed the diagnostic criteria of American Academy of Sleep Medicine 2005 (2nd edition)10). The criteria were: infants who require special conditions on falling asleep, or whose sleep-onset associations are highly problematic or demanding, or in the absence of the associated conditions whose sleep onset is significantly delayed or sleep is otherwise disrupted or nighttime awakenings require caregiver intervention for the child to return to sleep. If the sleep disturbance was caused by another sleep disorder, medical or neurological disorder, mental disorder, or medication use, the infant was excluded from the study.
We investigated the types of inappropriate association in infants, the level of depressive state and the marital intimacy in their parents. The parents were directed to complete the brief infant sleep questionnaire (BISQ) at the first interview and a sleep log to record the times of sleep, arousal and nighttime feeding of the infants in period of study. The Beck Depression Inventory (BDI) was used to investigate the depressive level of the parents. The intimacy level of couples was assessed using the Waring Intimacy Questionnaire (WIQ). Following the surveys, parents received sleep education and sleep training. The sleep training consisted of a full description of the normal sleep cycle of the infant, strategies to allow the infant to resume sleep by themselves (e.g., putting the baby to bed when "drowsy but awake", using different bed or room from the parents), gradual increasing of response time of behavioral intervention of the parents (or caregivers) if the infant was unable to fall asleep independently, education on the nighttime feeding (discontinuing nighttime feeding for infants over 6 months of age and avoiding reactive feeding whenever infants awake) and inappropriate sleep association and bedtime routine. Parents were also provided with a sleep training brochure. The parents revisited the outpatient clinic every 1 to 2 weeks to report on changes of frequency of the night waking in the infants and any difficulties that had risen during the behavioral intervention with the physician. Also, if the spouse or grandparents living with them disagreed on the behavioral sleep training on the infants, the dissenting family members were invited to the center and sleep education and training were retried and, after instruction on behavioral intervention, a follow-up was attempted. After 2 to 6 weeks, a prospective study resurveyed the frequency of night waking in infants by referral to the sleep log, and compared the initial BDI and WIQ scores with subsequent scores. If the parents had not revisited the outpatient clinic a follow-up telephone survey was done.
The BDI consists of 21 items. Each item has four possible answers, with a score of 0-3 assigned depending on the response. The total score (range, 0 to 63 points) was interpreted as follows: BDI score of 0-9 points was considered as not depressive, 10-15 points as a mildly depressive state, 16-23 points as a moderately depressive state, and over 24 points as a severely depressive state.
The WIQ is composed of eight independent content scales to assess components of marital intimacy (conflict resolution, affection, cohesion, sexuality, identity, compatibility, autonomy, and expressiveness)11). For each item, a score of 0-4 was assigned. A higher total score was indicative of lower intimacy level. We divided the parents into the groups according to the depressive level and compared the WIQ score of each group.
Means and standard deviations for the BDI and WIQ score were assessed. Paired samples t-test and Wilcoxon signed-rank test were performed to compare the BDI and WIQ scores before and after intervention. Pearson correlation analysis was also done to investigate the relationship between the pretraining BDI and WIQ scores. All statistical analyses were performed using the IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA). This study was carried out with the consent of the parents and was approved by the Institutional Review Board of the CHA Bundang Medical Center.
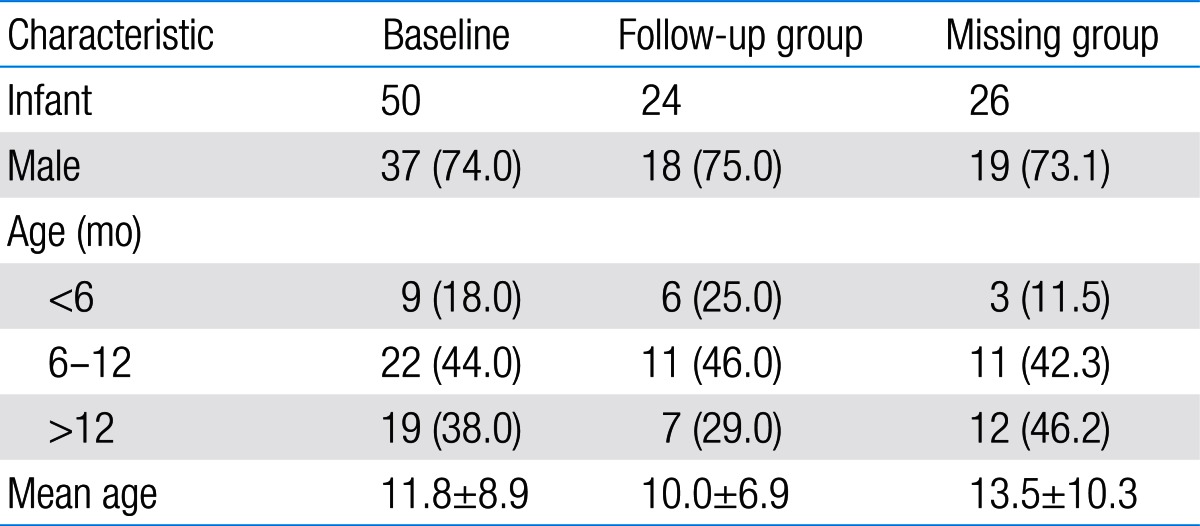
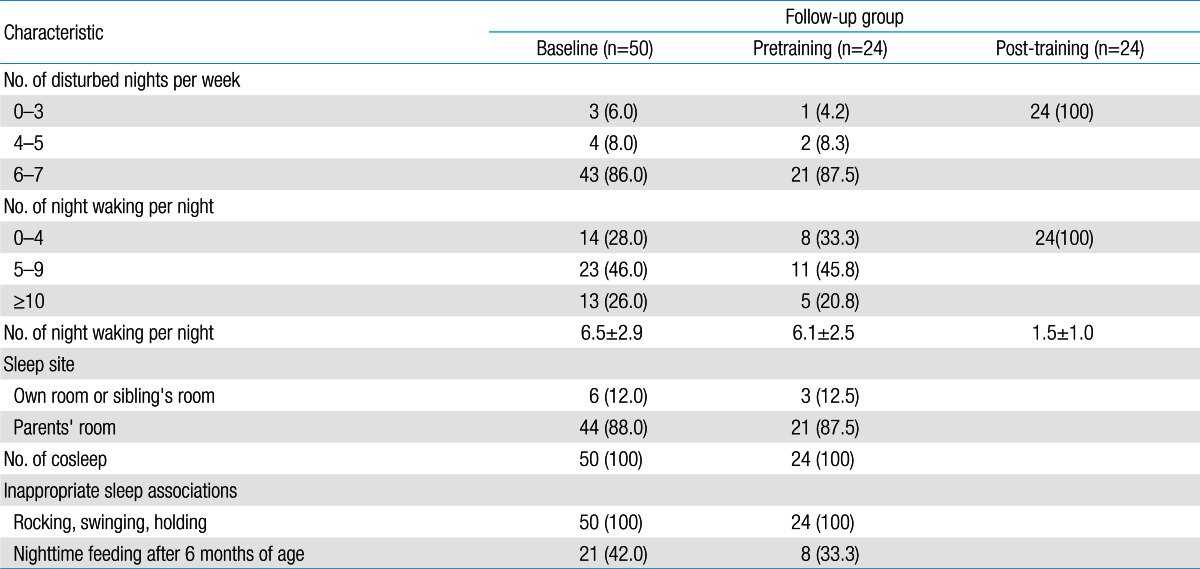
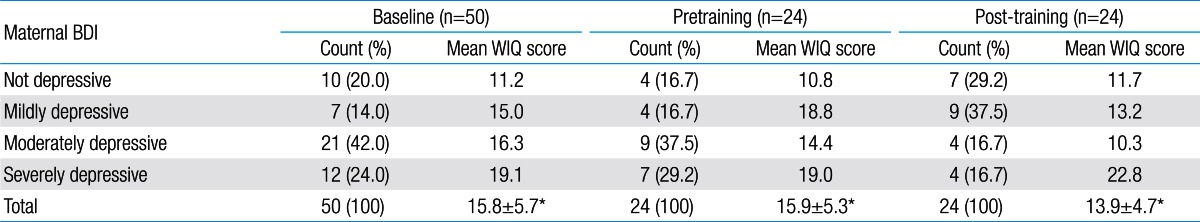
The 50 infants with SOAD consisted of 37 males and 13 females (mean age, 11.8±8.9 months). There were 50 mothers (mean age, 32.6 years) and 15 fathers (mean age, 37.1 years). In the follow-up study, 24 infants (mean age, 10.0±6.9 months) participated. Twenty-four mothers and two fathers were investigated in the follow-up study (Table 1).
Concerning the number of disturbed nights per week, 86.0% of the patients experienced 6 to 7 recorded disturbances. Concerning the frequency of night waking, 46% of the patients awoke 5 to 9 times per night and 28% awoke 1 to 4 times per night. Even when the infants had their own rooms or shared the room with the siblings, all the infants coslept with their parents especially the mothers (Table 2). Rocking, swinging, and holding until falling asleep were the most frequent inappropriate sleep onset associations (n=50), followed by persistent nighttime feeding after 6 months of age (n=21). After sleep education and behavioral sleep training, the mean number of night wakings decreased from 6.1±2.5 (n=24) to 1.5±1.0 (n=24) (P<0.01) (Table 2).
Sixty-five parents participated in the survey. Of these, the responses of 17 (26.2%) were not indicative of a depressive state, 12 (18.5%) displayed mild depression, 23 (35.4%) were in a moderately depressive state, and 13 (20.0%) were in a severely depressive state. Overall 74% of the parents had depressive symptoms. The mean BDI score for the parents was 16.7±9.2 (Table 3). The depressive level of the mothers and fathers was significantly different. The mean BDI score of the mothers of the infants with SOAD (n=50) was 18.4±9.2. Sixty-six percent showed moderately to severely depressive state and 14% displayed a mildly depressive state. A total of 80% of the mothers were in a depressive state. Compared to the mothers, the mean BDI score of the fathers was 11.1±7.2; 47% of the fathers were not depressed and only 20% were in the moderately to severely depressive state (Fig. 1). The depressive level of the mothers was more severe than the fathers with statistical significance (P=0.007). After sleep education and behavioral sleep training, the mean BDI score of the parents decreased from 16.7 (n=65) to 14.7 (n=26). For the 24 mothers who were tracked, the BDI score decreased from 20.6 to 15.0 points (P=0.002), and the portion of the moderately to severely depressive state decreased from 66.7% to 33.4% (n=24) (Tables 3, 4).
Initial WIQ score of the mothers seemed to be higher than fathers (15.8±5.7 vs. 14.8±4.4) without significance (Table 3). The WIQ score was the lowest in the group without depression and highest in the most depressive group, and showed that the intimacy level between the couple worsened in proportion to the depressive level (Fig. 2). After behavioral sleep training, the WIQ score of the mothers also significantly decreased from 15.9±5.3 to 13.9±4.7 points (n=24) (P=0.013), providing evidence of the improvement of the marital intimacy (Table 3, Fig. 3).
The results of this study clearly show that SOAD induces sleep deprivation of infants and their parents, and can produce a seriously depressive state in the caregiver, especially the mothers, resulting in deterioration of marital intimacy between the couple. A simple behavioral intervention with proper sleep education for parents can effectively resolve the frequent night awakening in infants and the depressive state of the parents, which can help restore harmonious relations between the couple.
Night awakenings are one of the most common sleep problems in infants, with 25-50% of children over the age of 6 months continuing to awake during the night12). Nighttime arousal normally occurs 4 to 6 times a night at an interval of 60-90 minutes, in a rhythm that follows the sleep cycle. But, if the caregiver feeds or rocks the baby every time when the infant cries or gives a signal, the parental intervention becomes necessary for the onset of sleep, setting the stage for SOAD (also termed sleep onset association type, behavioral insomnia in childhood)13). It has been demonstrated that sleep aids such as a pacifier and a cuddly object such as a teddy bear reduce the occurrence of sleep disorders, whereas prolonged breastfeeding and parental cosleeping interfere with the normal development of sleep14) though it has been debated that roomsharing in the presence of an active caregiver can reduce sudden infant death syndrome (SIDS) among some SIDS prone infants and the increased sensory contact and proximity between the mother and infant induces potentially beneficial behavioral and physiological changes in the infants15). In this study rocking, swinging, and holding until sleep had resumed were the most frequent inappropriate sleep onset associations (n=50), followed by nighttime feeding after 6 months of age (n=21), consistent with previous studies12,16,17).
Parents of infants with SOAD frequently suffered with sleep disruption, resulting in increasing fatigue, emotional instability, and depression17-19). Hiscock and Wake18) reported that sleep problems included the infants sleeping in the parent's bed, and being nursed to sleep were associated with high depression scores in their mothers and tended to increase as depression scores increased. Our results confirm previous findings that child sleep problems and maternal report of depression symptoms are highly associated. Same authors19) followed children aged 3 to 4 years with previous infant sleep problems and found that persistence or recurrence of infant sleep problems in the preschool years was common and was associated with higher child behavior problems and maternal depression scores. The authors suggested that depressive symptoms were a result, rather than a cause, of sleep problems. If left untreated, bedtime problems and night wakings can persist into childhood19,20). In a study involving 33 infants with sleep problems21), parents received sleep education, recorded sleep patterns in a sleep diary and, after 4 days, executed behavioral interventions for 2-4 hours every night by the same nurses. The authors found that both parents of infants with sleep problems similarly experienced a high degree of distress and there was no difference between mothers and fathers, but this stress decreased significantly after the intervention. Echoing this prior study, the present study confirms the effectiveness of the behavioral intervention and great improvement for a brief period of time. However, in our study the depressive level of the mothers was significantly more severe than the fathers, likely reflecting the more prominent role of the mother as the nighttime care giver, necessitating the mother's more frequent awakening. In Korean culture most mothers sleep with the babies, so this kind of discrepancy is expected.
Depression is one of the most common psychiatric diseases in women, particularly in childbearing age6). Postpartum depression affects approximately 10% to 15% of women4). The consequences of postpartum depression of women include not only impairment of maternal infant interactions such as insecurity of attachment, but also paternal depression7). As maternal depression negatively affects the mothers themselves, but also their children and partners, it is important to view depression within its social context, as it is a disease, which affects not only the individual but also the wider community6). Maternal depression is often accompanied by relationship difficulties with a high prevalence of marital disharmony and divorce22,23). According to Brown and Harris24) the lack of a confiding relationship is a vulnerability factor in the development of depression in women. Specifically the variable "low intimacy with husband" was associated with depression in women. In this study 80% of the mothers with the infants with SOAD were depressive. The rate for fathers was 50%. As the depressive level got higher marital intimacy worsened proportionally. These observations confirm that the infants' sleep disorder induces the serious depressive states of the parents, but also causes the conflict between the couple. Especially, the WIQ score of the mothers were higher than the fathers, reflecting the more severe degree of the depressive state in mothers. Even though the degree of depressive state of the fathers was not high as the mothers, almost half of the fathers were determined to be in a depressive state. In this study, the time spent by fathers in infant care was not surveyed; in Korean culture, it is the mother that assumes most of the responsibility for infant care, including during the night. It is conceivable that the depression experienced by the fathers is caused both by the sleep disturbance of the infants and by the deleterious influence of maternal depression, consistent with previous findings7).
In this study for the treatment of the infants with SOAD, proper sleep education and the behavioral sleep training improved the night wakings of the infants in a short period of time and lessened the depressive levels of the parents, especially of the mothers. However, nine parents (eight mothers and one father) out of 26 showed aggravated levels of depression and intimacy in a follow-up survey. In detail, six of nine had not executed behavioral sleep training or had dropped out. For five of the six individuals, the reason was the disagreement within the family on the sleep training; the remaining patient was not trained due to illness. This implicates that the proper sleep training and the education of the behavioral intervention for all the family members is very important for the success of the treatment.
The present findings demonstrate that sleep problems of an infant not only disturbs the infant itself but also induces sleep deprivation for the parents, and can cause a serious depressive state in the parents, particularly maternally, further aggravating the intimacy of the couple. Sleep education of the parents and behavioral interventions can diminish the level of depression of the parents and increase the intimacy level of the couple in a very short period of time. However, the findings are limited by the small number of the patients and lack of investigation of previous psychiatric illnesses such as depression. The male-to-female ratio of the infants with sleep onset association was 3:1 in this study. Thus, it would have been difficult to discern if SOAD is actually more prevalent in male infants. A large scale community-based study is thought to be necessary. Almost all the missing parents from the follow-up answered from the telephone poll that they had not come to the clinic because the infants' sleep problem improved and they perceived no need for the follow-up visits, which may have been a source of bias.
Despite the limitations, this study is meaningful in that it is the first study to investigate the depression and intimacy level among parents of the infants with SOAD in Korea, where infant-parental cosleeping is prevalent. A future study incorporating a larger number of the subjects is mandatory. Particularly in Korean society, where the rate of divorce is increasing, prompt diagnosis of SOAD is important, as it can be one of the hidden but major causes of the conflict between couples, particularly those who have had their first baby. As well, proper sleep education with the sleep training to establish the sound family is an important role of the pediatrician and also a social responsibility.
References
1. Mindell JA, Owens JA. Nightwakings: behavioral insomnia of childhood, sleep onset association type. Mindell JA, Owens JA, editors. A clinical guide to pediatric sleep diagnosis and management of sleep problems. 2010;2nd ed. Philadelphia: Lippincott Williams & Wilkins, :58–60.
2. Lavigne JV, Arend R, Rosenbaum D, Smith A, Weissbluth M, Binns HJ, et al. Sleep and behavior problems among preschoolers. J Dev Behav Pediatr 1999;20:164–169.


3. Bonuck K, Grant R. Sleep problems and early developmental delay: implications for early intervention programs. Intellect Dev Disabil 2012;50:41–52.


5. Byars KC, Yeomans-Maldonado G, Noll JG. Parental functioning and pediatric sleep disturbance: an examination of factors associated with parenting stress in children clinically referred for evaluation of insomnia. Sleep Med 2011;12:898–905.


6. Burke L. The impact of maternal depression on familial relationships. Int Rev Psychiatry 2003;15:243–255.


7. Goodman JH. Paternal postpartum depression, its relationship to maternal postpartum depression, and implications for family health. J Adv Nurs 2004;45:26–35.


8. Mao A, Burnham MM, Goodlin-Jones BL, Gaylor EE, Anders TF. A comparison of the sleep-wake patterns of cosleeping and solitary-sleeping infants. Child Psychiatry Hum Dev 2004;35:95–105.



9. Latz S, Wolf AW, Lozoff B. Cosleeping in context: sleep practices and problems in young children in Japan and the United States. Arch Pediatr Adolesc Med 1999;153:339–346.

10. American Academy of Sleep Medicine. The international classification of sleep disorders: diagnostic and coding manual. 2005;2nd ed. Westchester: American Academy of Sleep Medicine.
11. Waring EM, Reddon JR. The measurement of intimacy in marriage: the Waring Intimacy Questionnaire. J Clin Psychol 1983;39:53–57.


12. Mindell JA, Kuhn B, Lewin DS, Meltzer LJ, Sadeh A. American Academy of Sleep Medicine. Behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep 2006;29:1263–1276.


13. Goodlin-Jones BL, Burnham MM, Gaylor EE, Anders TF. Night waking, sleep-wake organization, and self-soothing in the first year of life. J Dev Behav Pediatr 2001;22:226–233.



14. Benhamou I. Sleep disorders of early childhood: a review. Isr J Psychiatry Relat Sci 2000;37:190–196.

15. McKenna JJ, McDade T. Why babies should never sleep alone: a review of the co-sleeping controversy in relation to SIDS, bedsharing and breast feeding. Paediatr Respir Rev 2005;6:134–152.


16. Morgenthaler TI, Owens J, Alessi C, Boehlecke B, Brown TM, Coleman J Jr, et al. Practice parameters for behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep 2006;29:1277–1281.


17. Mindell JA, Sadeh A, Kohyama J, How TH. Parental behaviors and sleep outcomes in infants and toddlers: a cross-cultural comparison. Sleep Med 2010;11:393–399.


18. Hiscock H, Wake M. Infant sleep problems and postnatal depression: a community-based study. Pediatrics 2001;107:1317–1322.


19. Lam P, Hiscock H, Wake M. Outcomes of infant sleep problems: a longitudinal study of sleep, behavior, and maternal well-being. Pediatrics 2003;111:e203–e207.


20. Gaylor EE, Burnham MM, Goodlin-Jones BL, Anders TF. A longitudinal follow-up study of young children's sleep patterns using a developmental classification system. Behav Sleep Med 2005;3:44–61.



21. Thome M, Skuladottir A. Evaluating a family-centred intervention for infant sleep problems. J Adv Nurs 2005;50:5–11.


Fig. 1
Baseline Beck Depression Inventory (BDI) group for mothers (n=50, A) and fathers (n=15, B). The proportion of moderately to severely depressive state in mothers was higher than that in fathers. The mean BDI for the mothers (18.4±9.2) was higher than the fathers (11.1±7.2) with statistical significance (P=0.007).
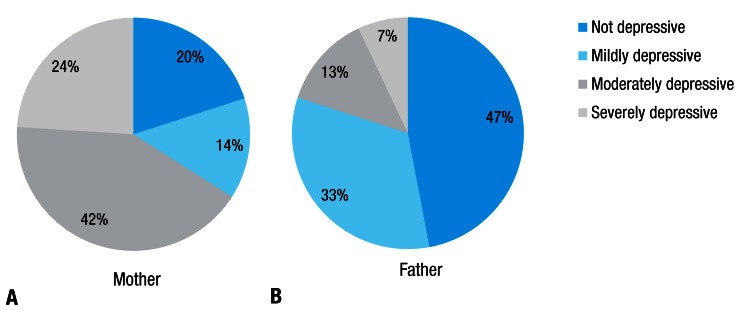
Fig. 2
Correlation between Beck Depression Inventory (BDI) and Waring Intimacy Questionnaire (WIQ) score (baseline n=65). BDI and WIQ positively correlated. The linear equation is WIQ=8.845+(0.402×BDI) and R2 is 0.692 (P<0.001).
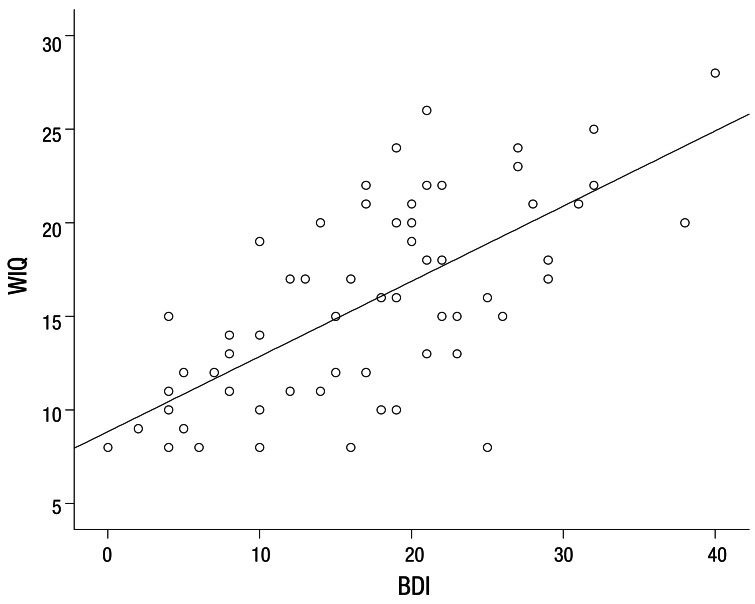
Fig. 3
Change of Beck Depression Inventory (BDI) and Waring Intimacy Questionnaire (WIQ) score of the 24 mothers who were followed after sleep training. The 24 subjects were analyzed by paired t-test and the mean and the standard deviation of initial BDI (A) was 20.6±9.6 and at follow-up the score decreased to 15.0±10.7 (P=0.002). Change of WIQ score of mothers who were followed after sleep training is at the right. A total result of 24 was analyzed by Wilcoxon signed-rank test. The mean±standard deviation of initial WIQ was 15.8±5.7 and was 13.9±4.7 at follow-up (P=0.013).
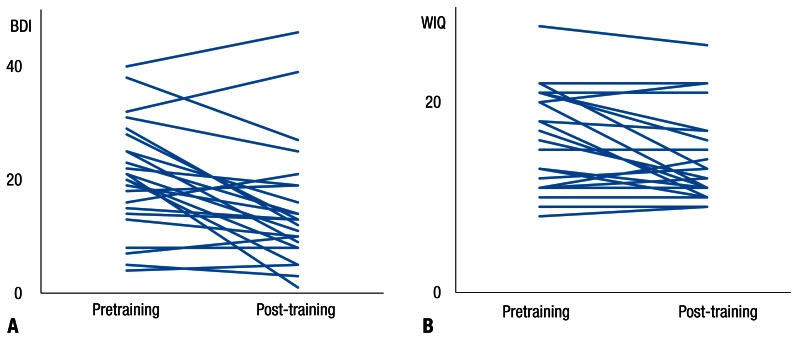
Table 3
Presleep and postsleep training BDI and WIQ in parents

Values are presented as mean±standard deviation (number).
BDI, Beck Depression Inventory; WIQ, Waring Intimacy Questionnaire.
*P value between the pretraining and post-training group. †BDI, score of the mothers (P=0.002) and WIQ score of the mothers (P=0.013) decreased with statistical significance.



 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


