Article Contents
| Clin Exp Pediatr > Volume 55(10); 2012 |
Abstract
Purpose
Although benign rolandic epilepsy (BRE) is a benign condition, it may be associated with a spectrum of behavioral, psychiatric, and cognitive disorders. This study aimed to assess the cognitive and other neuropsychological profiles of children with BRE.
Methods
In total, 23 children with BRE were consecutively recruited. All children underwent sleep electroencephalography (EEG) and were assessed on a battery of comprehensive neuropsychological tests including the Korean versions of the Wechsler intelligence scale for children III, frontal executive neuropsychological test, rey complex figure test, Wisconsin card sorting test, attention deficit diagnostic scale, and child behavior checklist scale.
Results
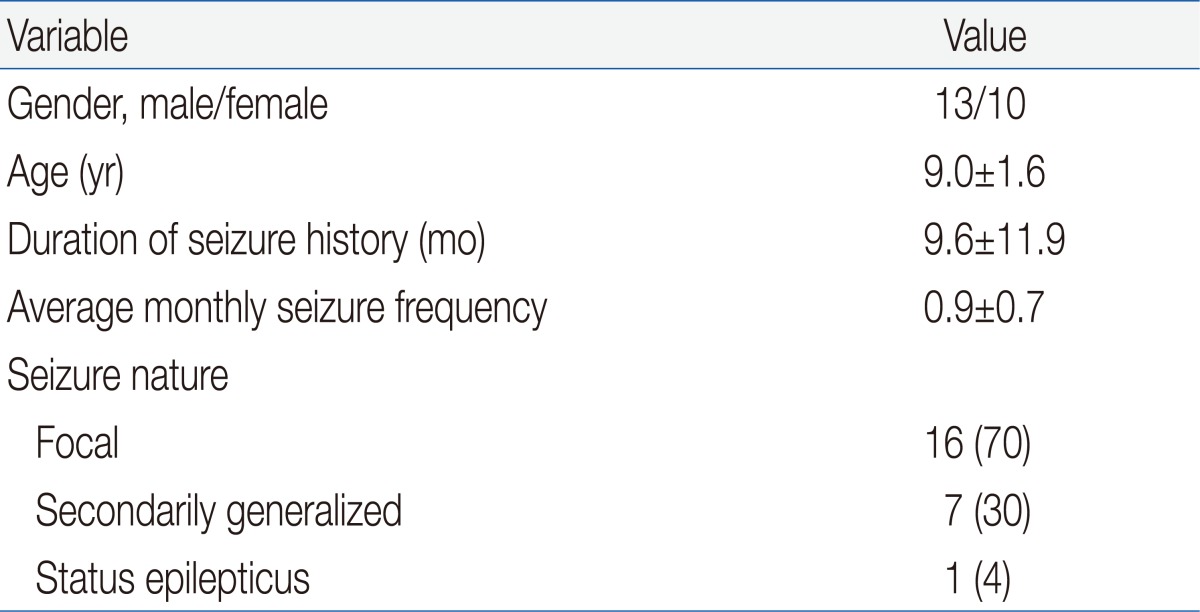
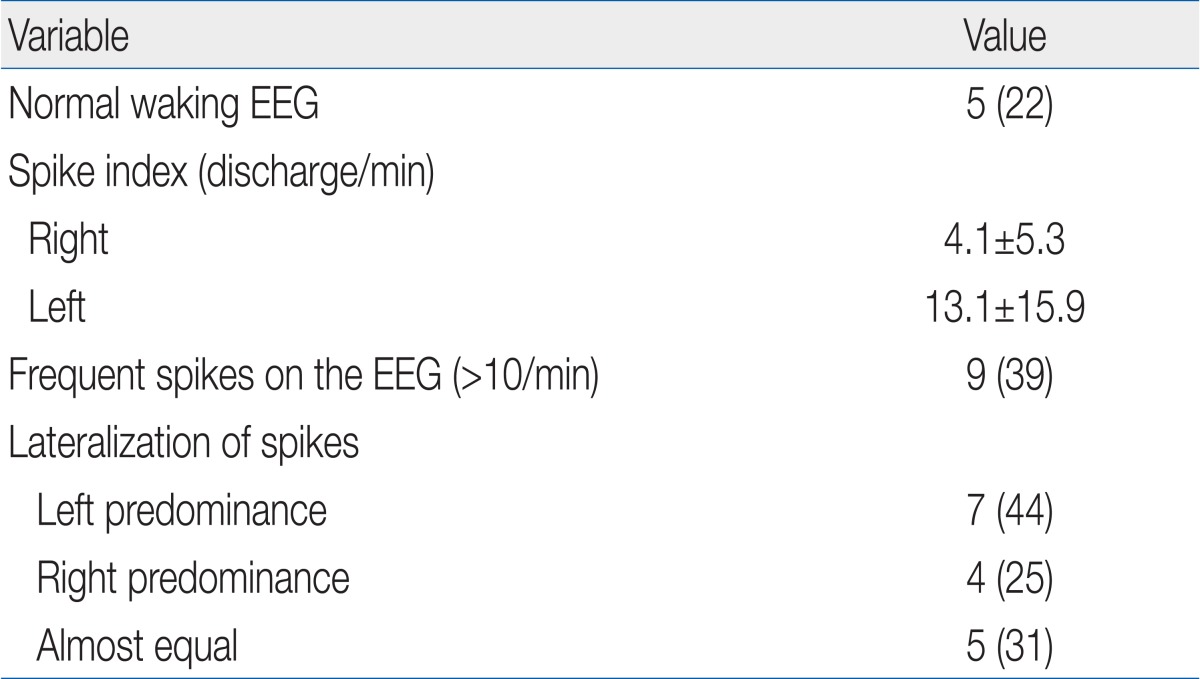
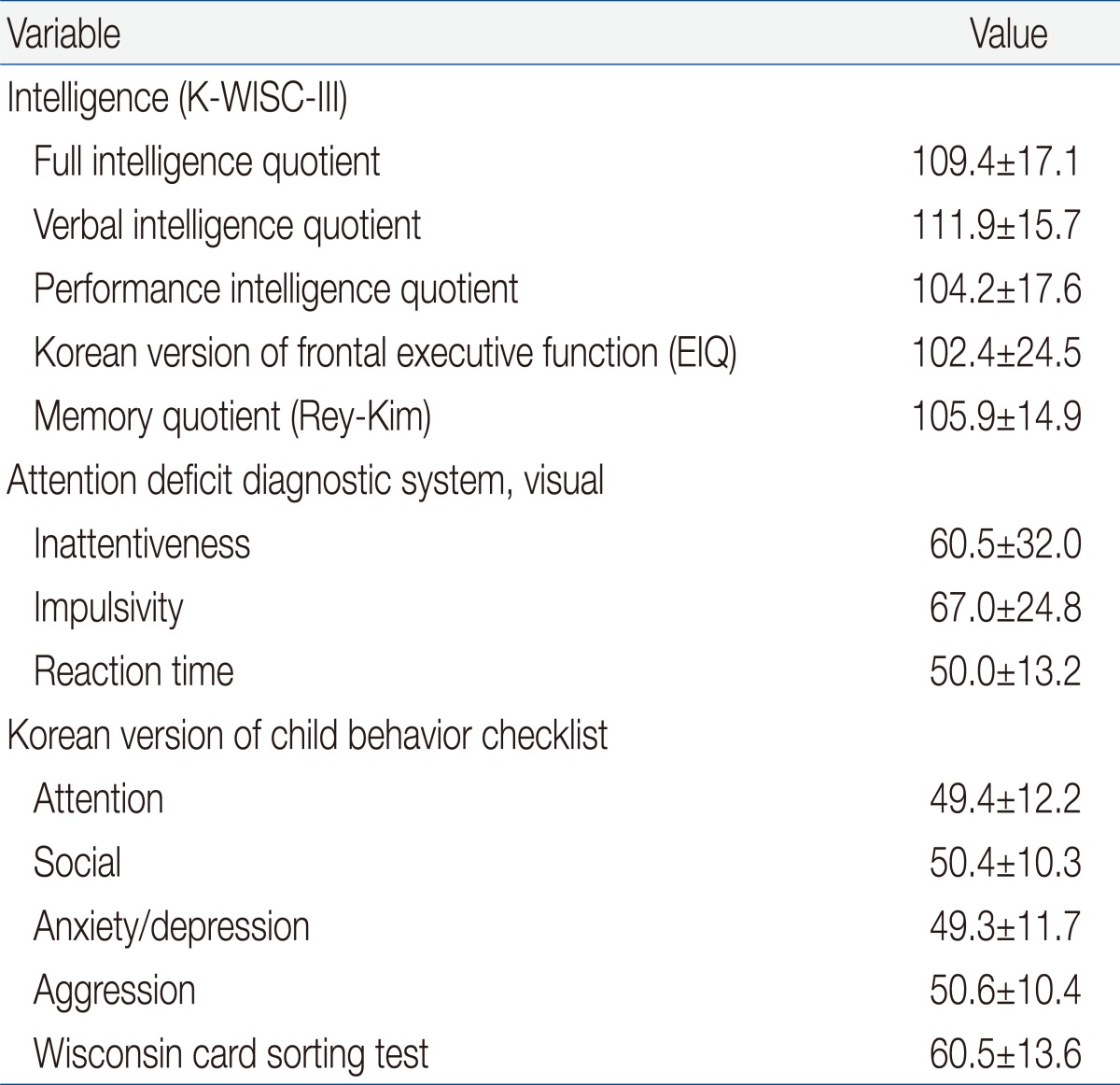
The study subjects included 13 boys and 10 girls aged 9.0±1.6 years. Our subjects showed an average monthly seizure frequency of 0.9±0.7, and a majority of them had focal seizures (70%). The spike index (frequency/min) was 4.1±5.3 (right) and 13.1±15.9 (left). Of the 23 subjects, 9 showed frequent spikes (>10/min) on the EEG. The subjects had normal cognitive and frontal executive functions, memory, and other neuropsychological sub-domain scores, even though 8 children (35%) showed some evidence of learning difficulties, attention deficits, and aggressive behavior.
Conclusion
Our data have limited predictive value; however, these data demonstrate that although BRE appears to be benign at the onset, children with BRE might develop cognitive, behavioral, and other psychiatric disorders during the active phase of epilepsy, and these problems may even outlast the BRE. Therefore, we recommend scrupulous follow-up for children with BRE.
Benign rolandic epilepsy (BRE) or benign childhood epilepsy with centrotemporal spikes is the most common condition of idiopathic focal epilepsies in children. Generally speaking, it is known to be benign because of the absence of neurological deficits, infrequent focal somatosensory or motor seizures predominantly occurring during sleep, reasonable response to the medication and spontaneous resolution before the age of 15 to 16 years.
Recently, several studies have demonstrated that children with BRE are at a higher risk for cognitive, behavioral or emotional difficulties in association with frontal lobe dysfunctions1-8). However, there is no clear delineation of a uniform neurocognitive profile for the children with BRE. The aim of the present study was to assess the cognitive, behavioral and other neuropychological aspects in children with newly diagnosed BRE, just prior to the active phase of epilepsy. The study may be a useful investigative tool to examine the subjects without brain damage, therapies, and other environmental influences. Thus, neuropsychological dysfunction in these children may support the idea that epilepsy itself plays an important role in both cognitive and other neuropsychological difficulties.
A total of 23 children with BRE were involved in the study. They were consecutively recruited from the pediatric neurology clinic, Kyungpook National University Hospital, Daegu, Korea. Based on the clinical features and EEG findings, a diagnosis of BRE was made by two pediatric neurologists. Subjects were included when they had experienced two or more seizures over the past one year and their parents or legal guardians consented to their participation in the study. Exclusion criteria included primarily generalized seizures, partial epilepsy of a symptomatic etiology, and a history of taking antiepileptic drugs over the previous three months.
All children underwent both a waking and a sleep EEG, and data from each was acquired by two experienced specialists. The location and frequency of spikes were quantified for each subject. The spike index was calculated by dividing the number of spikes by the time spent, and was classified as "very frequent" (>10 discharges/min).
Each participant went through a comprehensive neuropsychological battery of tests to evaluate various aspects of mental function including cognition, behavior, emotion, attention, memory and executive function. The test battery has been provided in Table 1.
The data were statistically analyzed using PASW ver. 18.0.0 (IBM Co., Armonk, NY, USA). Statistical analysis of the results was performed using the means and their corresponding standard deviations (SD). Statistical significance was regarded at a P value of <0.05.
The present study was formally approved by the Institutional Review Board (74005-1379).
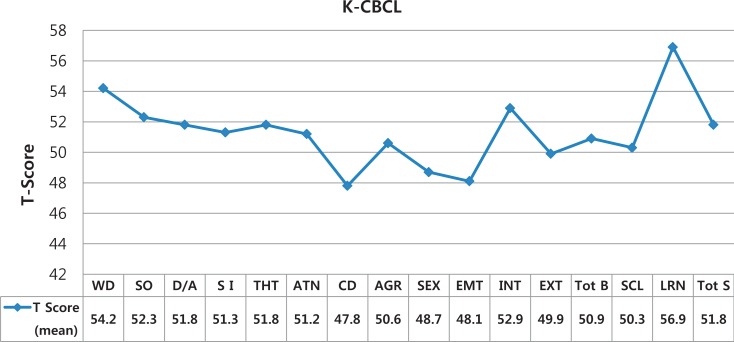
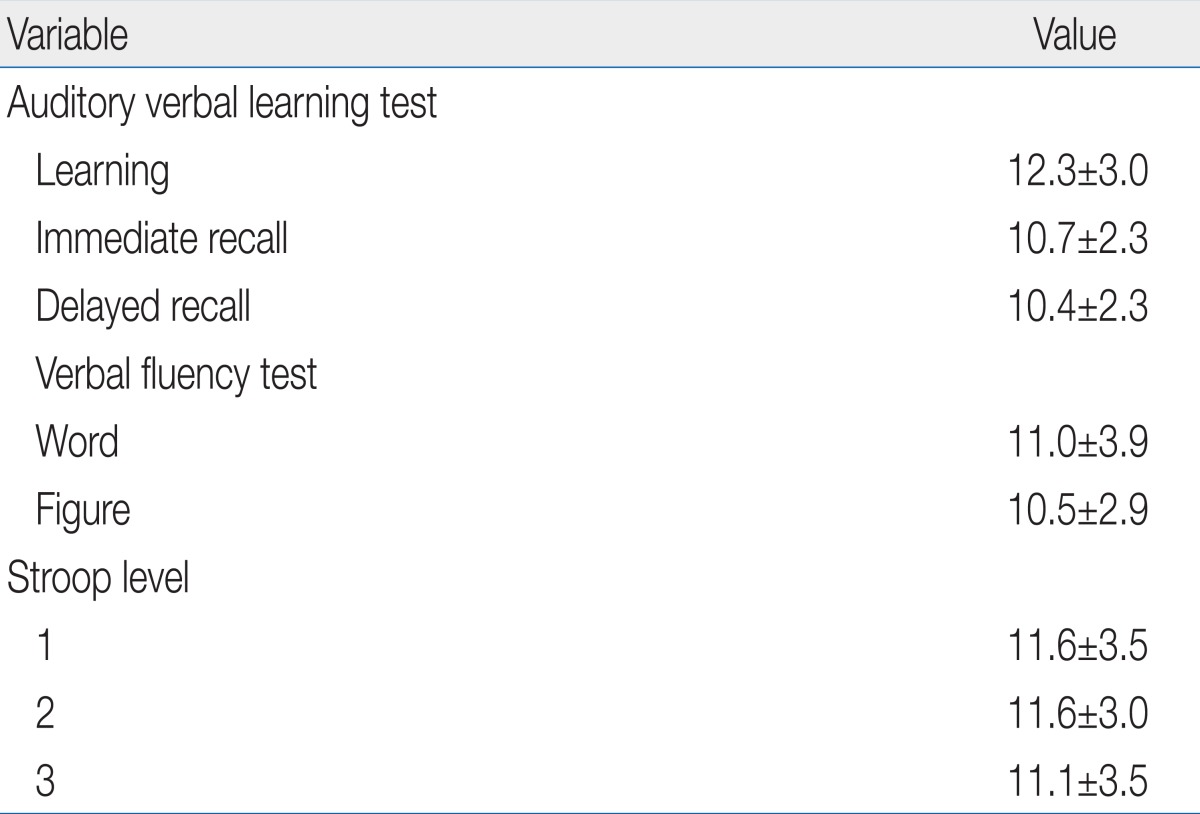
A total of 23 children with BRE (13 males/10 females, 9.0±1.6 years) were evaluated in the study. As illustrated in Table 2, the average monthly seizure frequency of the subjects was 0.9±0.7. Sixteen out of 23 (70%) had focal seizures and 7 (30%) had secondarily seizures, in which a child presented with status epilepticus. Table 3 shows EEG findings of the subjects. Five out of 23 (22%) initially had a normal waking EEG. The spike index was 4.1±5.3 (right) and 13.1±15.9 (left). Nine out of 23 subjects had very frequent spikes on the EEG (>10/min). With respect to lateralization of spikes, seven (44%) were predominant on the left, 4 (25%) were predominant on the right, 5 (31%) were almost equal. Table 4 presents results of the neuropsychological assessment of the subjects. Overall, they exhibited normal cognitive function (full intelligence quotient [FIQ], 109.4±17.1; verbal IQ [VIQ], 111.9±15.7; performance IQ [PIQ], 104.2±17.6), frontal executive function (EIQ, 102.4±24.5), memory (MQ, 105.9±14.9), attention, and other neuropsychological measurements, even though a child revealed borderline cognitive function (FIQ, 71; VIQ, 73; PIQ, 75). Table 5 depicts information on the major sub-domain scores in the frontal executive function and memory. The subjects exhibited normal function on the major sub-domains such as auditory verbal learning test, verbal fluency (VF) and stroop tests. However, individualized test scores demonstrated that one child scored much lower on the rey complex figure test (<3), two with the VF (<6) and one failed level 1 of the stroop test (<3). In addition, five out of 23 children (22%) scored worse (>70) on the vision based attention deficit diagnostic scales (ADS). As illustrated in Fig. 1, the subjects appeared to have no significant behavioral, emotional or other problems. However, three out of 23 subjects (13%) scored greater than 70 on the attention problem, aggressive behavior and externalization items and four scored higher (65 to 70) on withdrawal, somatic problems, depression/anxiety and social immaturity items of the Korea-Child Behavior Checklist.
Despite the presumed benign nature of BRE, some evidence now exists that patients with this disorder may have cognitive, behavioral, emotional and other neuropsychological deficits2,4,5,7,9-15). In general, they have demonstrated that the full scale IQ is usually within the normal range, but lower scores have been noted on language related tasks, some executive functions, attention, memory, auditory and verbal learning tasks and a variety of behavioral and emotional difficulties. It is not easy to investigate the complex links between BRE and neuropsychological dysfunction, but the present study focused on evaluating the neuropsychological status in various aspects in newly diagnosed BRE, which is drug free, at the beginning of the active phase.
In the present study, five out of 23 children (22%) showed atypical clinical features such as status epilepticus, developmental delay and the existence of cognitive, behavioral, emotional or attention problems as reported in other studies16,17). With respect to the EEG findings, twenty children (87%) revealed a rolandic focus. Nine (39%) belonged to "very frequent spikes' of the definition proposed by Weglage et al.18). There was no clear significance on the lateralization of spikes in the subjects.
Based on the statistical scores of neuropsychological tests, even including sub-domains, the subjects of this study exhibited normal cognitive function, frontal executive function, memory, attention, and other neuropsychological measurements. However, individualized test scores on several sub-domains revealed a different aspect. Like many previous studies1,4,6,8,19-26), this study also revealed that 8 children (35%) had memory impairment, problems in VF, frontal executive dysfunction and attention deficits which led to poor academic performance. The language impairment in children with BRE and the acquired aphasia in Landau-Kleffner syndrome (LKS) indicate a large spectrum of interactions between language function and epilpsy. As a result, whether specific language impairment and LKS should rather be considered along a continuum or as two entirely distinct entities is to be answered in the future.
Furthermore, 4 children (17%) were noted to have attention deficits, aggressive behavior and other behavioral or emotional disturbances.
This study is limited stemming from a relatively small sample size, the heterogeneity of subjects, and poor performance due to immature grapho-motor skills on some neuropsychological tests including ADS. As a result, large scale, more objective studies are needed in the future.
In conclusion, the data have shown that BRE appears to be benign at the onset but, may be at risk for cognitive, behavioral and other psychiatric disorders during the active phase of epilepsy and these problems might even outlast it. We therefore recommend that close follow-up with regular neuropsychological tests, if necessary is needed in children with BRE.
References
1. Danielsson J, Petermann F. Cognitive deficits in children with benign rolandic epilepsy of childhood or rolandic discharges: a study of children between 4 and 7 years of age with and without seizures compared with healthy controls. Epilepsy Behav 2009;16:646–651.


2. Ay Y, Gokben S, Serdaroglu G, Polat M, Tosun A, Tekgul H, et al. Neuropsychologic impairment in children with rolandic epilepsy. Pediatr Neurol 2009;41:359–363.


3. Hoie B, Sommerfelt K, Waaler PE, Alsaker FD, Skeidsvoll H, Mykletun A. The combined burden of cognitive, executive function, and psychosocial problems in children with epilepsy: a population-based study. Dev Med Child Neurol 2008;50:530–536.


4. Wirrell E, Sherman EM, Vanmastrigt R, Hamiwka L. Deterioration in cognitive function in children with benign epilepsy of childhood with central temporal spikes treated with sulthiame. J Child Neurol 2008;23:14–21.


5. Deltour L, Quaglino V, Barathon M, De Broca A, Berquin P. Clinical evaluation of attentional processes in children with benign childhood epilepsy with centrotemporal spikes (BCECTS). Epileptic Disord 2007;9:424–431.


6. Sart ZH, Demirbilek V, Korkmaz B, Slade PD, Dervent A, Townes BD. The consequences of idiopathic partial epilepsies in relation to neuropsychological functioning: a closer look at the associated mathematical disability. Epileptic Disord 2006;8:24–31.


7. Nicolai J, Aldenkamp AP, Arends J, Weber JW, Vles JS. Cognitive and behavioral effects of nocturnal epileptiform discharges in children with benign childhood epilepsy with centrotemporal spikes. Epilepsy Behav 2006;8:56–70.


8. Vinayan KP, Biji V, Thomas SV. Educational problems with underlying neuropsychological impairment are common in children with Benign Epilepsy of Childhood with Centrotemporal Spikes (BECTS). Seizure 2005;14:207–212.


9. Goldberg-Stern H, Gonen OM, Sadeh M, Kivity S, Shuper A, Inbar D. Neuropsychological aspects of benign childhood epilepsy with centrotemporal spikes. Seizure 2010;19:12–16.


10. Verrotti A, D'Egidio C, Agostinelli S, Parisi P, Chiarelli F, Coppola G. Cognitive and linguistic abnormalities in benign childhood epilepsy with centrotemporal spikes. Acta Paediatr 2011;100:768–772.


11. Genizi J, Shamay-Tsoory SG, Shahar E, Yaniv S, Aharon-Perez J. Impaired social behavior in children with benign childhood epilepsy with centrotemporal spikes. J Child Neurol 2012;27:156–161.


12. Metz-Lutz MN, Filippini M. Neuropsychological findings in Rolandic epilepsy and Landau-Kleffner syndrome. Epilepsia 2006;47(Suppl 2): 71–75.

13. Besag FM. Behavioral aspects of pediatric epilepsy syndromes. Epilepsy Behav 2004;5(Suppl 1): S3–S13.
14. Baglietto MG, Battaglia FM, Nobili L, Tortorelli S, De Negri E, Calevo MG, et al. Neuropsychological disorders related to interictal epileptic discharges during sleep in benign epilepsy of childhood with centrotemporal or Rolandic spikes. Dev Med Child Neurol 2001;43:407–412.


15. Zenkov LR, Konstantinov PA, Shiriaeva IIu, Miasnikov VN, Sirazitdinova EB, Shevel'chisnkiĭ SI. Mental and behavioral disorders in idiopathic focal epileptiform spikes. Zh Nevrol Psikhiatr Im S S Korsakova 2007;107:39–49.
16. Verrotti A, Latini G, Trotta D, Giannuzzi R, Cutarella R, Morgese G, et al. Typical and atypical rolandic epilepsy in childhood: a follow-up study. Pediatr Neurol 2002;26:26–29.


17. Wirrell EC, Camfield PR, Gordon KE, Dooley JM, Camfield CS. Benign rolandic epilepsy: atypical features are very common. J Child Neurol 1995;10:455–458.


18. Weglage J, Demsky A, Pietsch M, Kurlemann G. Neuropsychological, intellectual, and behavioral findings in patients with centrotemporal spikes with and without seizures. Dev Med Child Neurol 1997;39:646–651.


19. Fonseca LC, Tedrus GM, de Oliveira ED, Ximenes VL. Benign childhood epilepsy with centrotemporal spikes: word and pseudoword discrimination. Arq Neuropsiquiatr 2009;67(2B): 450–456.


20. Tedrus GM, Fonseca LC, Melo EM, Ximenes VL. Educational problems related to quantitative EEG changes in benign childhood epilepsy with centrotemporal spikes. Epilepsy Behav 2009;15:486–490.


21. Pinton F, Ducot B, Motte J, Arbues AS, Barondiot C, Barthez MA, et al. Cognitive functions in children with benign childhood epilepsy with centrotemporal spikes (BECTS). Epileptic Disord 2006;8:11–23.


22. Fonseca LC, Tedrus GM, Tonelotto JM, Antunes Td Tde A, Chiodi MG. School performance in children with benign childhood epilepsy with centrotemporal spikes. Arq Neuropsiquiatr 2004;62(2B): 459–462.


23. Soria C, Callu D, Viguier D, El Sabbagh S, Bulteau C, Laroussinie F, et al. Parental report of cognitive difficulties, quality of life and rehabilitation in children with epilepsy or treated for brain tumour. Dev Neurorehabil 2008;11:268–275.


24. Vago C, Bulgheroni S, Franceschetti S, Usilla A, Riva D. Memory performance on the California Verbal Learning Test of children with benign childhood epilepsy with centrotemporal spikes. Epilepsy Behav 2008;13:600–606.


Fig. 1
Sub-domain scores in Korean version of child behavior checklist (K-CBCL) of the subjects (n=23). WD, withdrawn; SO, somatic problems; D/A, depressed/anxious; SI, socially immature; THT, thought problems; ATN, attention problems; CD, conduct problems; AGR, aggressive behavior; SEX, sexual problems; EMT, emotional problems; INT, internalization; EXT, externalization; TBH, total behavioral problems; SCL, social problems; LRN, learning performance; TSO, total social problems.




 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


