Article Contents
| Clin Exp Pediatr > Volume 60(12); 2017 |
|
Abstract
Purpose
Atrioventricular nodal reentry tachycardia (AVNRT) is less common in pediatric patients than in adult patients. Thus, data for pediatric AVNRT patients are insufficient. Hence, we aimed to analyze the patient characteristics, treatment, and any recurrences in pediatric AVNRT patients.
Methods
We reviewed the records of 50 pediatric AVNRT patients who had undergone radiofrequency catheter ablation (RFCA) between January 1998 and December 2016 at a single regional center. The patients were aged Ōēż18 years.
Results
Among 190 pediatric patients who underwent RFCA for tachyarrhythmia, 50 (26.3%; mean age, 13.4┬▒2.6 years) were diagnosed as having AVNRT by electrophysiological study. Twenty-five patients (25 of 50, 50%) were male. Twenty patients (20 of 50, 40%) used beta-blockers before RFCA. All patients had no structural heart disease except 1 patient with valvular aortic stenosis and coarctation of the aorta. RFCA was performed using the anatomic approach under fluoroscopic guidance. The most common successfully ablated region was the midseptal region (25 of 50, 50%). Slow pathway (SP) ablation and SP modulation were performed in 43 and 6 patients, respectively. Complication occurred in 1 patient with complete atrioventricular block. During follow-up, 6 patients had recurrence of supraventricular tachycardia, as confirmed by electrocardiography. Among them, 5 underwent successful ablation at the first procedure. In 1 patient, induction failed during the first procedure.
In pediatric patients with supraventricular tachycardia (SVT), atrioventricular nodal reentry tachycardia (AVNRT) occurs less frequently than atrioventricular reentry tachycardia1,2). Despite their small proportion, pediatric AVNRT patients are reported to be as successfully and safely treated with radiofrequency catheter ablation (RFCA) as adult patients3,4). This study evaluated the efficacy of RFCA by retrospectively analyzing data on pediatric AVNRT patients who underwent RFCA at a single regional center.
This study evaluated data on pediatric patients aged Ōēż18 years who underwent electrophysiology studies (EPSs) and RFCA between January 1998 and December 2016 in accordance with the Kyungpook National University Hospital guidelines5,6). Of 190 patients who underwent EPS and RFCA, 50 (26.3%) had AVNRT. Patients with concomitant AVNRT and other arrhythmias were excluded. The medical records of the 50 AVNRT patients were reviewed for baseline characteristics, type of procedure, results of the procedure, and characteristics of patients with postprocedure recurrent AVNRT.
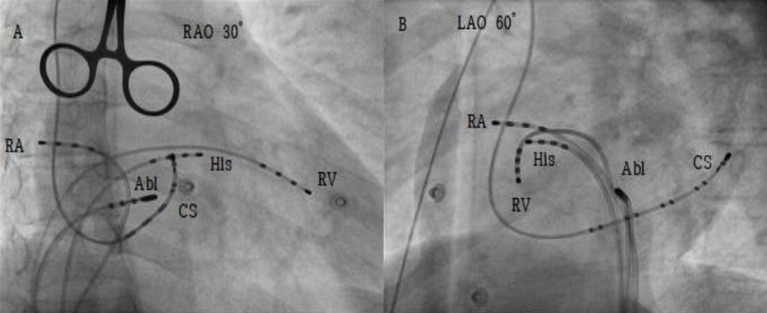
Written informed consent was obtained from all the patients before the procedure. Procedures were performed mostly under local anesthesia with lidocaine, but conscious sedation was also used depending on the age and preference of the patients. AVNRT was induced in each patient by using programmed electrical stimulation (PES) (Fig. 1). In the patients whose AVNRT could not be induced by PES or tachycardia were nonpersistent, PES induction was performed again when the heart rate was increased by 20%ŌĆō30% above the basal heart rate by using isoproterenol (1ŌĆō1.5 ┬Ąg/min). The procedure was performed with the anatomical approach under fluoroscopic guidance (Fig. 2). Radio frequency pulse was applied to the appropriate position at the maximum power of 50ŌĆō60 W and maximum temperature of 60Ōäā. Ablation began from the posterior region of the triangle of Koch and progressed anteriorly as deemed necessary. Junctional rhythm that occurs during ablation masks the atrioventricular (AV) block and increases the risk of an AV block. To prevent this, ablation was performed with atrial pacing at a rate 20%ŌĆō30% higher than the basal heart rate. Thirty minutes after successful ablation, we tried to reinduce AVNRT with PES by using isoproterenol. The success of an ablation was defined as zero echo beat and jump during induction after ablation, and 1 echo beat or jump observed after ablation without the induction of tachycardia was defined as modification. Patients who were asymptomatic after RFCA were followed up for at least 2 years after the procedure, and those with symptoms or recurrence were followed up long-term.
Fifty patients underwent EPS and RFCA for AVNRT, of whom 25 were male and 25 were female. The mean age and body weight of the patients were 13.4┬▒2.6 years and 49.6┬▒12.4 kg, respectively. One of the patients had structural heart diseases (valvular aortic stenosis and coarctation of the aorta), which was surgically corrected prior to the procedure. Twenty patients (40%) received beta blockers for recurrent tachycardia prior to the procedure. Eleven patients needed conscious sedation during EPS and RFCA, and 13 (26%) needed tachycardia induction with isoproterenol due to failure of induction with PES. The mean procedure time was 138.3┬▒28.4 minutes, and the mean fluoroscopy time was 31.4┬▒14.2 minutes. Of the 50 patients who underwent EPS and RFCA, 43 successfully completed slow pathway (SP) ablation and 6 completed SP modification. One patient had a failed ablation due to failed tachycardia induction caused by damage to the AV node fast pathway during insertion of the catheter in the coronary sinus os. Of the regions that were successfully ablated, the midseptal region showed the highest success rate (25 of 50, 50%). Five patients developed transient AV block during ablation (5 of 50, 10%), and they all improved during the procedure. However, 1 patient developed complete AV block during the procedure (1 of 50, 2%), which persisted to this day and is being followed up. The patients were followed up for at least 2 years after ablation. Before discontinuing follow-up, patients without notable symptoms were educated to revisit if symptoms or other problems develop. Seventeen patients were reassessed during follow-up for short bouts of palpitation that lasted a few seconds, chest discomfort, or dizziness (17 of 50, 34%), and 6 of them had confirmed SVT on electrocardiography (6 of 50, 12%). The mean time to recurrence in the patients with recurrent AVNRT was 49.6┬▒12.4 months (Table 1). Of the patients with recurrence, 3 had successful reablations with EPS and RFCA, and are being followed up without particular symptoms. One of the 3 patients was the patient who had an unsuccessful RFCA at the first procedure due to induction failure (Table 2). Of the 6 patients who underwent modification during the first RFCA, 4 have no issues so far and 2 reported symptoms of short bouts of palpitation (a few seconds) but were not confirmed on electrocardiography and 24-hour Holtor.
The success rate of RFCA in pediatric AVNRT cases reported by the Pediatric Radiofrequency Catheter Ablation Registry and the Pediatric Electrophysiology Society was 95%, which was similar to that noted in adults7). The results of this study were consistent with those of this report, which reported a success rate of 98%. Reported complications of RFCA include AV block, bleeding, stroke, and infection, but in this study, transient AV block during ablation was the most frequent8). Recent reports show that transient AV block occurs in 2% of adult AVNRT patients, and permanent AV block occurs in 0.2% of adult AVNRT patients. However, in this study, the incidence rates of transient AV block and permanent AV block were higher at 10% and 2%, respectively, owing to the smaller number of patients compared to adult AVNRT patients9). Cases of transient AV block in this study were temporary, and all improved during the procedure or 1ŌĆō2 days. Transient AV block can occur due to the edema in tissues surrounding the AV node during ablation, but it usually improves as edema improves10). However, there have been reports of adult AVNRT patients with intra-ablation transient AV block who later developed delayed AV block; hence, long-term follow-up of patients who develop transient AV block during the procedure is warranted11,12).
The recurrence rate in adult AVNRT patients after successful ablation is reported to be 3%ŌĆō5.8%13,14,15). In this study, recurrence was observed in 12% of patients including those in whom the initial ablation failed. Many studies reported residual SP conduction to be a risk factor for recurrence16,17). However, other studies reported that residual SP conduction is not a risk factor for recurrence18,19). In this study, 5 patients, excluding 1 in whom the initial ablation failed, underwent complete SP ablation during the initial ablation. Conversely, of the 6 patients who underwent SP modification during the initial ablation, 4 have not reported any issues thus far, and 2 are being followed up for symptoms of palpitation that lasts a few seconds, although electrocardiography or 24-hour Holtor findings did not reveal any abnormalities. Although statistical significant could not be verified owing to the small number of subjects with recurrent AVNRT, it can be presumed that the increase in the recurrence rate is not related to SP modification at the initial ablation. Further research is needed to re-establish the endpoint of ablation in pediatric AVNRT patients. In adult AVNRT patients, being female less than 20 years of age is reported to be another risk factor for recurrence after ablation, but this study only included patients aged less than 18 years, and the recurrent rate did not differ between sexes20). A multicenter study is necessary to identify risk factors of recurrence, considering that our study had a small number of pediatric AVNRT patients and that recurrent AVNRT is more prevalent in adult patients than in pediatric patients.
This study has a few limitations. First, it is a retrospective study with a small number of enrolled subjects. Second, EPS was recommended for accurate evaluation of recurrence, but only 3 out of the 17 symptomatic patients agreed to undergo EPS. This study highlights the need for the establishment of ablation endpoint for pediatric AVNRT patients as well as research on risk factors for AVNRT recurrence. However, this was difficult to achieve via a single-center analysis with a limited number of patients. Therefore, an additional multicenter study with large pediatric patient cohorts is necessary.
Notes
Conflicts of interest:
No potential conflict of interest relevant to this article was reported.
References
1. Ko JK, Deal BJ, Strasburger JF, Benson DW Jr. Supraventricular tachycardia mechanisms and their age distribution in pediatric patients. Am J Cardiol 1992;69:1028ŌĆō1032.


2. Wu MH, Lin JL, Lai LP, Young ML, Lu CW, Chang YC, et al. Radiofrequency catheter ablation of tachycardia in children with and without congenital heart disease: indications and limitations. Int J Cardiol 2000;72:221ŌĆō227.


3. Kugler JD, Danford DA, Houston KA, Felix G. Pediatric Radiofrequency Ablation Registry of the Pediatric Radiofrequency Ablation Registry of the Pediatric Electrophysiology Society. Pediatric radiofrequency catheter ablation registry success, fluoroscopy time, and complication rate for supraventricular tachycardia: comparison of early and recent eras. J Cardiovasc Electrophysiol 2002;13:336ŌĆō341.


4. Van Hare GF, Javitz H, Carmelli D, Saul JP, Tanel RE, Fischbach PS, et al. Prospective assessment after pediatric cardiac ablation: recurrence at 1 year after initially successful ablation of supraventricular tachycardia. Heart Rhythm 2004;1:188ŌĆō196.



5. Brugada J, Blom N, Sarquella-Brugada G, Blomstrom-Lundqvist C, Deanfield J, Janousek J, et al. Pharmacological and non-pharmacological therapy for arrhythmias in the pediatric population: EHRA and AEPC-Arrhythmia Working Group joint consensus statement. Europace 2013;15:1337ŌĆō1382.


6. Page RL, Joglar JA, Caldwell MA, Calkins H, Conti JB, Deal BJ, et al. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2016;67:e27ŌĆōe115.


7. Van Hare GF, Carmelli D, Smith WM, Kugler J, Silka M, Friedman R, et al. Prospective assessment after pediatric cardiac ablation: design and implementation of the multicenter study. Pacing Clin Electrophysiol 2002;25:332ŌĆō341.



8. Greyling A, Ector J, Garweg C. Radiofrequency catheter ablation in infants and children. SA Heart 2017;14:16ŌĆō20.
9. Wasmer K, Dechering DG, K├Čbe J, Leitz P, Frommeyer G, Lange PS, et al. Patients' and procedural characteristics of AV-block during slow pathway modulation for AVNRT-single center 10year experience. Int J Cardiol 2017;244:158ŌĆō162.


10. Shailesh F, Sewani A, Paydak H. Recurrent AV block following ablation for AVNRT. Indian Heart J 2014;66:710ŌĆō713.



11. Fenelon G, d'Avila A, Malacky T, Brugada P. Prognostic significance of transient complete atrioventricular block during radiofrequency ablation of atrioventricular node reentrant tachycardia. Am J Cardiol 1995;75:698ŌĆō702.


12. Williamson BD, Man KC, Daoud E, Niebauer M, Strickberger SA, Morady F. Radiofrequency catheter modification of atrioventricular conduction to control the ventricular rate during atrial fibrillation. N Engl J Med 1994;331:910ŌĆō917.


13. Estner HL, Ndrepepa G, Dong J, Deisenhofer I, Schreieck J, Schneider M, et al. Acute and long-term results of slow pathway ablation in patients with atrioventricular nodal reentrant tachycardia--an analysis of the predictive factors for arrhythmia recurrence. Pacing Clin Electrophysiol 2005;28:102ŌĆō110.


14. Bastani H, Schwieler J, Insulander P, Tabrizi F, Braunschweig F, Kenneb├żck G, et al. Acute and long-term outcome of cryoablation therapy of typical atrioventricular nodal reentrant tachycardia. Europace 2009;11:1077ŌĆō1082.


15. Rostock T, Willems S. Atrioventricular nodal reentrant tachycardia in the elderly: efficacy and safety of radiofrequency catheter ablation. Pacing Clin Electrophysiol 2007;30:828ŌĆō829.


16. Liberman L, Hordof AJ, Fishberger SB, Pass RH. The role of isoproterenol testing following radiofrequency catheter ablation of accessory pathways in children. Pacing Clin Electrophysiol 2003;26(2 Pt 1): 559ŌĆō561.


17. Stellbrink C, Diem B, Schauerte P, Brehmer K, Schuett H, Hanrath P. Differential effects of atropine and isoproterenol on inducibility of atrioventricular nodal reentrant tachycardia. J Interv Card Electrophysiol 2001;5:463ŌĆō469.


18. Fujii E, Kasai A, Omichi C, Matsuoka K, Teramura S, Uchida F, et al. Electrophysiological determinants of persistent dual atrioventricular nodal pathway physiology after slow pathway ablation in atrioventricular nodal reentrant tachycardia. Pacing Clin Electrophysiol 2000;23(11 Pt 2): 1916ŌĆō1920.


19. Kose S, Amasyali B, Aytemir K, Kilic A, Can I, Kursaklioglu H, et al. Atrioventricular nodal reentrant tachycardia with multiple discontinuities in the atrioventricular node conduction curve: immediate success rates of radiofrequency ablation and long-term clinical follow-up results as compared to patients with single or no AH-jumps. J Interv Card Electrophysiol 2004;10:249ŌĆō254.


Fig.┬Ā1
Intracardiac electrogram which shows jump and initiation of atrioventricular nodal reentry tachycardia (AVNRT).

Fig.┬Ā2
Fluoroscopic position of intracardiac electrode and ablation catheter. RAO, right anterior oblique; LAO, left anterior oblique; RA, right atrium; His, his hundle; RV, right ventricle; Abl, ablation catheter; CS, coronary sinus.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


